What made Sadhguru lose his Consciousness? Subdural Hematoma: A Neurological Emergency – Dr Rahul Chawla
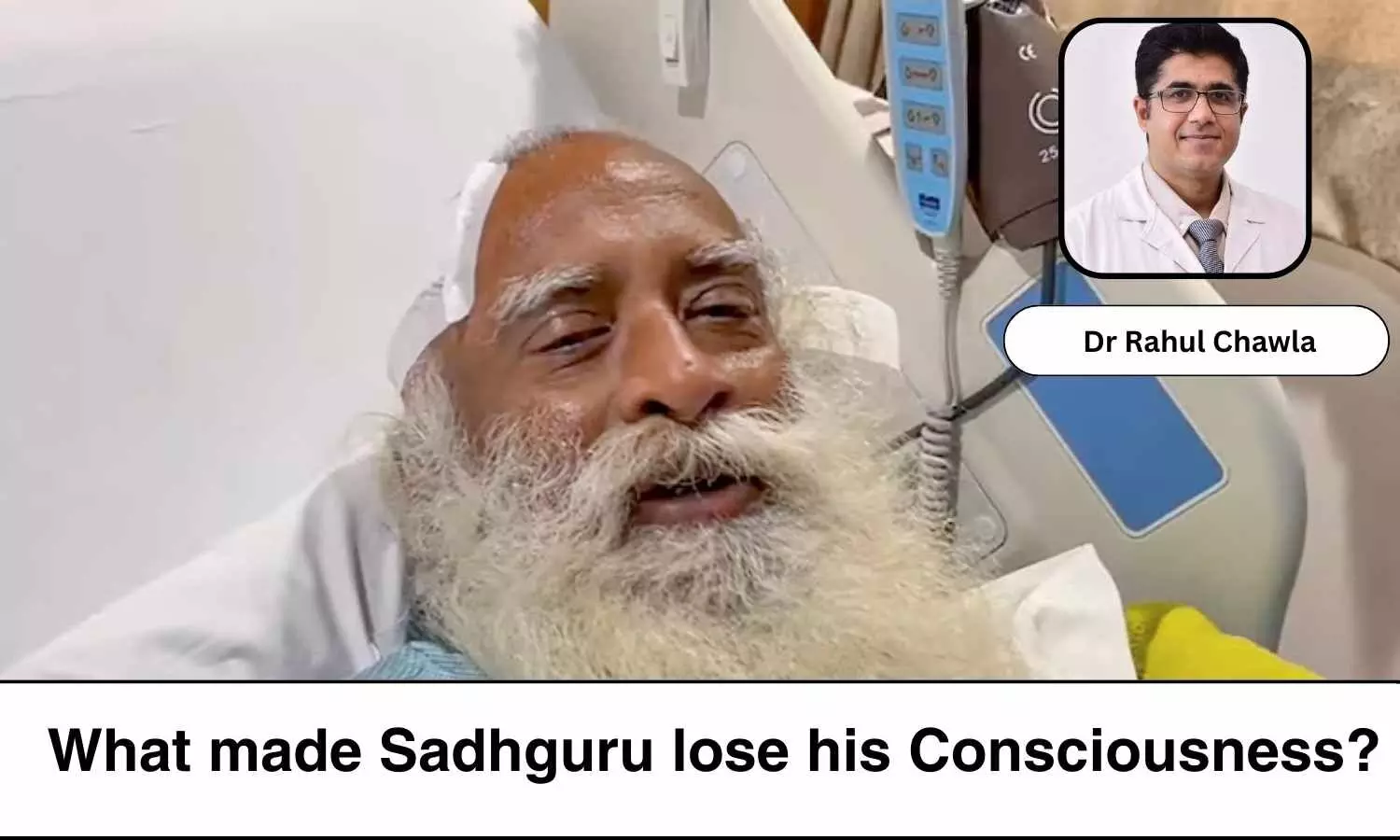
Recently, renowned Spiritual Guru and founder of the Isha Foundation, Sadhguru, underwent surgery for bleeding in the brain, as reported by the media. The condition is known as Subdural hematoma (SDH).
SDH is a neurological emergency condition characterized by the accumulation of blood between the dura mater and the arachnoid membrane, two layers of the meninges that cover the brain. Here, the blood accumulation occurs outside the brain parenchymas and produces neurological symptoms due to the compression of underlying structures of the brain. Acute severe SDH can be life-threatening, with significant morbidity and mortality if not promptly treated.
Etiology and High Risk Factors
Subdural hematomas can occur due to various reasons:
1. Head Trauma, including falls, motor vehicle accidents, and assaults. Chronic alcohol consumers are especially predisposed to SDH due to trivial trauma that patients might not be aware of.
2. Thrombocytopenia or Low platelet counts predispose the patients to bleeding tendencies.
3. Chronic Liver Disease
4. Use of antiplatelet or anticoagulant therapies: Patients on anticoagulant medications such as Warfarin with INR above 3 are at risk for SDH or any internal bleeding. Patients on aspirin are also known to have a risk for SDH.
5. Chronic subdural hematomas can develop spontaneously in the elderly due to the tearing of bridging veins with minor trauma or even without any apparent injury.
Symptoms
The symptoms of SDH include headaches, confusion, vomiting, weakness on one side of the body, difficulty speaking or understanding speech, seizures, behavioural changes, impaired awareness and loss of consciousness.
Diagnosis
Any patient with a history of head trauma with acute onset headache with red flags such as recurrent vomiting, seizures, focal neurological deficit, abnormal behaviour etc. should undergo NCCT Brain to rule out any space-occupying lesion or bleeding inside the brain, whether intraparenchymal haemorrhage or SDH.
NCCT Brain should also be considered in the absence of a red flag on history, but neurological examination is suggestive of signs of raised intracranial pressure, such as altered mental status, pupil abnormalities, and focal neurological deficits.
Brain imaging (NCCT Brain or MRI Brain) helps determine the size, location and extension of SDH, and the management can be decided based on findings on imaging.
Management of SDH
1. Monitoring: Patients with acute SDH are required to be admitted and monitored for any change in sensorium, development of any new onset neurological deficit.
2. Medical Management: Patients are managed with anti-seizure medications and decongestant therapy. Patients can be considered for surgery if a patient has severe SDH, altered mental status or development of neurological deficit.
3. Surgerical therapy: Patients undergo Burr hole surgery or Craniotomy depending on the size of SDH and neurological status of the patient.
What did we learn from Sadhguru?
Sadhguru had been having severe headaches 3 weeks prior, but he neglected the symptoms and continued with his commitments. Since he was having chronic or subacute SDH, the symptoms evolved rather slowly over 2 weeks. Only when he started developing neurological deficits and altered consciousness did he decide to get admitted and operated upon as per the advice of treating physicians.
Hence, it is important to listen to your body, identify symptoms, seek advice from expert doctors, and not become disillusioned by any alternative therapy.
Any patient with new onset severe headache in the presence of any of the red flag signs such as diminution in vision, altered behaviour, seizures, neurological deficit in the form of limb weakness, speech abnormalities or impaired consciousness- should seek urgent help from hospitals with neurological emergency care facilities.
If you know anyone who has these symptoms, get him/her to the hospital at the earliest.
Be Aware! Stay Healthy!
Disclaimer: The views expressed in this article are of the author and not of Medical Dialogues. The Editorial/Content team of Medical Dialogues has not contributed to the writing/editing/packaging of this article.
Facebook Comments



