Transscleral Cyclophotocoagulation effectively lowers IOP among glaucoma patients:Study
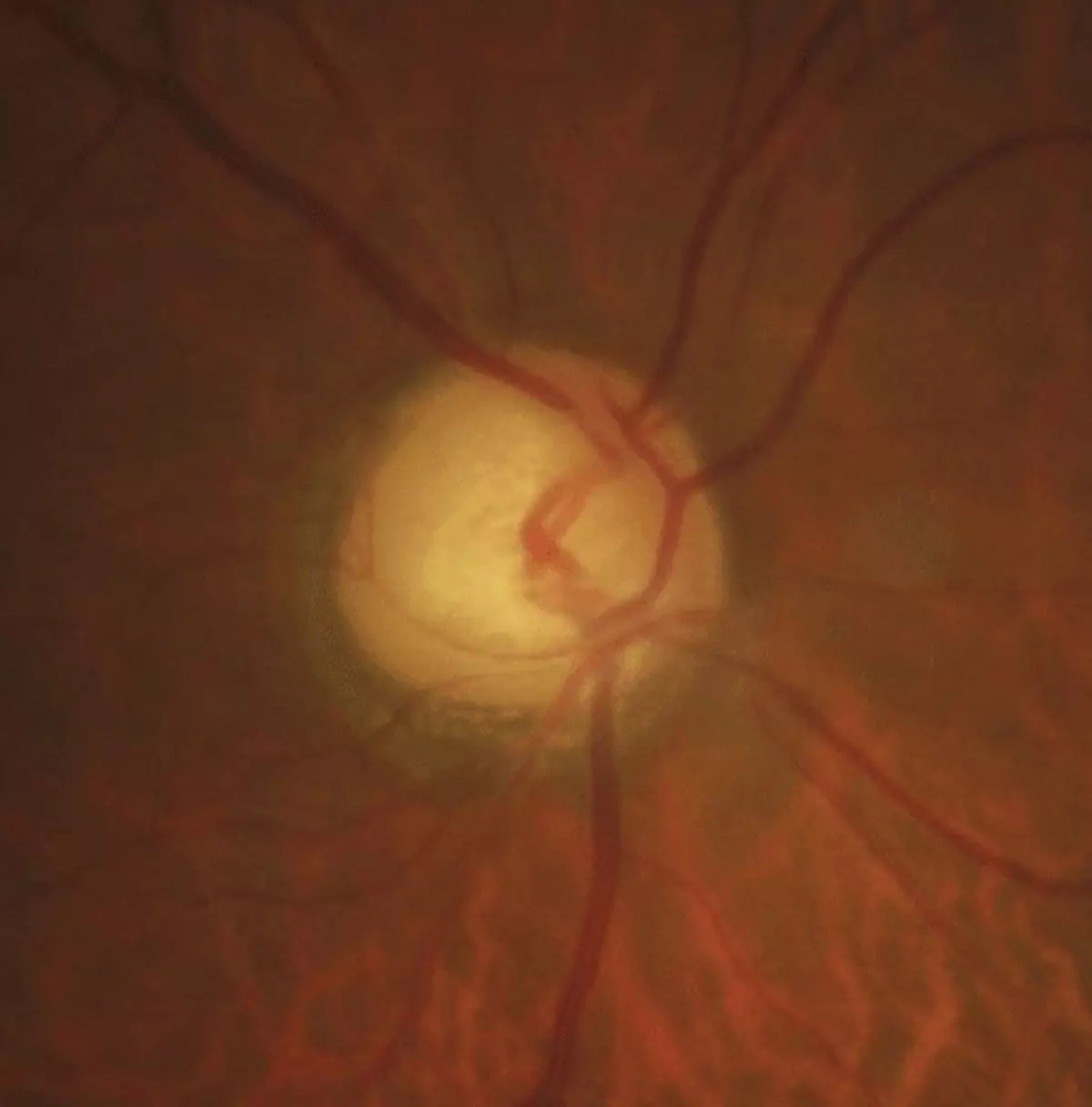
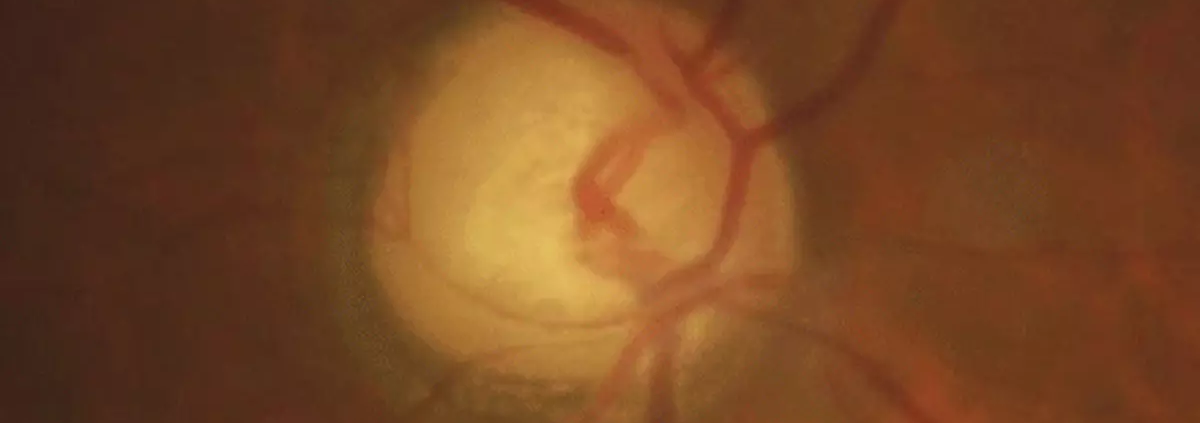
Glaucoma encompasses a heterogeneous group of eye diseases
associated with progressive loss of optic nerve fibers, with consequent loss of
corresponding visual field. Several risk factors have been identified for the
development and progression of this condition, but intraocular pressure (IOP)
is still the primary modifiable risk factor. IOP-lowering can be achieved with
eye drops or laser trabeculoplasty (both currently considered to be first line
options in most glaucoma cases), or surgery, which is mostly reserved for
patients who progress despite non-surgical maximal tolerated treatment or if
there is a very advanced disease stage or glaucoma type where non-surgical
treatment is not expected to be able to lower IOP to the levels that are expected
to stop disease progression. The majority of surgeries performed are filtering
surgeries and aim to lower IOP through an increased outflow, but there are also
options that aim for a reduction of aqueous humour (AH) production, such as the
cyclodestructive or cyclomodulating procedures, which are still usually used as
a last resource or when other types of surgery are deemed very likely to be
unsuccessful.
In cyclodestructive procedures, unlike other surgeries, the
IOP lowering effect is obtained by ablation of the ciliary body with subsequent
reduction of AH production. The most widely used technique is Laser Cyclophotocoagulation
(CPC), namely the Diode Laser Transscleral Cyclophotocoagulation (TSCPC).
During TSCPC, a semiconductor diode laser (810 nm) is transmitted through the
overlying sclera and absorbed by melanin in the ciliary processes, leading to
selective thermal coagulation of the ciliary body. Despite the simplicity of
the procedure (comparing to incisional filtering surgery), cycloablation is
feared among some ophthalmologists due to the risk of persistent hypotony,
phthisis bulbi and loss of visual acuity. The risk of hypotony with TSCPC can
be as high as 18% (namely in cases of neovascular glaucoma (NVG). Moreover, the
reported success rates are highly variable (36.7–94.4%), possibly due to
heterogeneity in methodologies regarding the definitions of patient population,
energy settings, success and follow-up duration. It is also important to
acknowledge that the majority of the studies only established an upper IOP
limit for the definition of success, therefore not excluding patients with
hypotony.
Despite the increasing evidence regarding TSCPC, according
to the latest version of the European Glaucoma Society Guidelines, refractory
glaucoma (glaucoma for which the target intraocular pressure (IOP) has not been
achieved despite maximum tolerated medical treatments and/or conventional,
properly performed filtration surgery) or expected incisional surgery failure
remain the only formal indications for TSCPC use.
There is a need for more evidence concerning this procedure,
in order to try to expand its indications. Therefore, this study intended to
provide more data regarding the efficacy and safety of TSCPC, based on a
Portuguese population with glaucoma or ocular hypertension treated at a
tertiary centre, with a 2-year follow-up post-procedure.
Ribeiro et al carried a retrospective review of the records
of all adult patients who underwent their first TSCPC treatment between 2014
and 2019 at Unidade Local de Saúde de São João, Porto, Portugal. Data regarding
intraocular pressure (IOP), best corrected visual acuity, number of
IOP-lowering medications, use of oral acetazolamide, retreatments and
complications during a 2-year period following TSCPC were registered. The
primary outcome was overall success at 2 years, defined as IOP≥ 6 and ≤21 mmHg,
with at least 20% IOP reduction from baseline, with or without IOP-lowering
medications (qualified and complete success, respectively), without the
development of phthisis bulbi or loss of light perception due to glaucoma and
no further glaucoma procedures except TSCPC retreatment.
Ninety-six eyes from 96 patients were included, mean age was
63 (±14) years. Mean IOP at baseline was 39.1 (±13.3) mmHg. Mean IOP reduction
at 2 years was 18.5 (42.9%) mmHg (±16.0, min −16.0, max 56.0) (p < 0.001)
and a significant reduction in the number of IOP-lowering medications and use
of oral acetazolamide was observed. IOP reduction at 2 years was positively
correlated with baseline IOP (r=0.682; p < 0.001). Overall success (including
complete and qualified) was achieved in 42 patients (43.8%), with 34 (35.4%)
presenting qualified success. Neovascular glaucoma (NVG) was the predominant
diagnosis (n = 30, 31.3%), with a higher mean baseline IOP of 46.3 mmHg (±11.8,
min 21.0, max 70.0) and a larger mean IOP reduction at 2 years of 24.7 (51.0%)
mmHg (±16.4, min −2.0, max 55.0). Thirteen patients (13.5%) developed
persistent hypotony, eight of which converted to phthisis bulbi, of which half
had NVG.
The results of the study demonstrated a significant effect
of TSCPC in reducing both IOP and the need for IOP-lowering topical and/or oral
medications in the management of patients with glaucoma. The overall success
rate was 37.5% at 12 months and 43.8% at 24 months. The majority (23 patients,
64%) of patients with overall success after 12 months also achieved success at
24 months without the need of additional TSCPC, suggesting a sustained effect
of this procedure between the first and second year. Nonetheless, the rate of
complications observed is not negligible, with 13 (13.5%) of the patients
developing persistent hypotony, and of these, 8 evolved to phthisis bulbi.
Regarding BCVA, 26.3% of patients with vision (light perception, hand motion
and counting fingers) progressed to no light perception.
In conclusion, the study shows that TSCPC can be an
effective IOP-lowering procedure, demonstrating a stronger effect when
preoperative IOP is highest. Authors confirmed that there is a wide variability
in the effect and a considerable amount of postoperative complications, such as
persistent hypotony and phthisis bulbi, which are more pronounced in certain
glaucoma types such as NVG. More studies are required, ideally with less
advanced cases, to establish appropriate energy levels, duration and extension,
based on each patient’s clinical characteristics, thus allowing for higher
success rates, more predictability and less complications.
Source: Ribeiro et al; Clinical Ophthalmology 2024:18
https://doi.org/10.2147/OPTH.S473788