Tranexamic Acid in Trauma: Case of a Young Woman Highlights Risk of Acute Renal Cortical Necrosis
France: A recent case published in BMC Nephrology highlights the possible role of tranexamic acid (TXA) in precipitating acute bilateral renal cortical necrosis (RCN) in a young trauma patient, raising concerns about its administration, especially in the presence of additional thrombotic risk factors.
The researchers note that TXA is used widely as an antifibrinolytic agent in managing postpartum hemorrhage and severe traumatic bleeding. However, its potential association with renal cortical necrosis remains unclear, with only a few reported cases in non-obstetric settings. Previous reports on TXA-induced RCN suggest a rapid onset of acute kidney injury (AKI), with most cases requiring hemodialysis. The recovery of renal function varies, with some patients remaining dialysis-dependent.
Manal Mazloum, University of Montpellier, Montpellier, France, and colleagues describe the case of a 24-year-old woman with no prior medical history who was admitted to intensive care following a high-energy car accident. Despite stable hemodynamics and the absence of active arterial hemorrhage, she received an initial 1 g dose of TXA along with supportive therapy. Shortly after administration, her blood pressure dropped, necessitating norepinephrine support, which was quickly tapered. Laboratory investigations ruled out disseminated intravascular coagulation (DIC) and thrombotic microangiopathy (TMA), but 48 hours later, she developed AKI with anuria and rising serum creatinine levels, requiring hemodialysis.
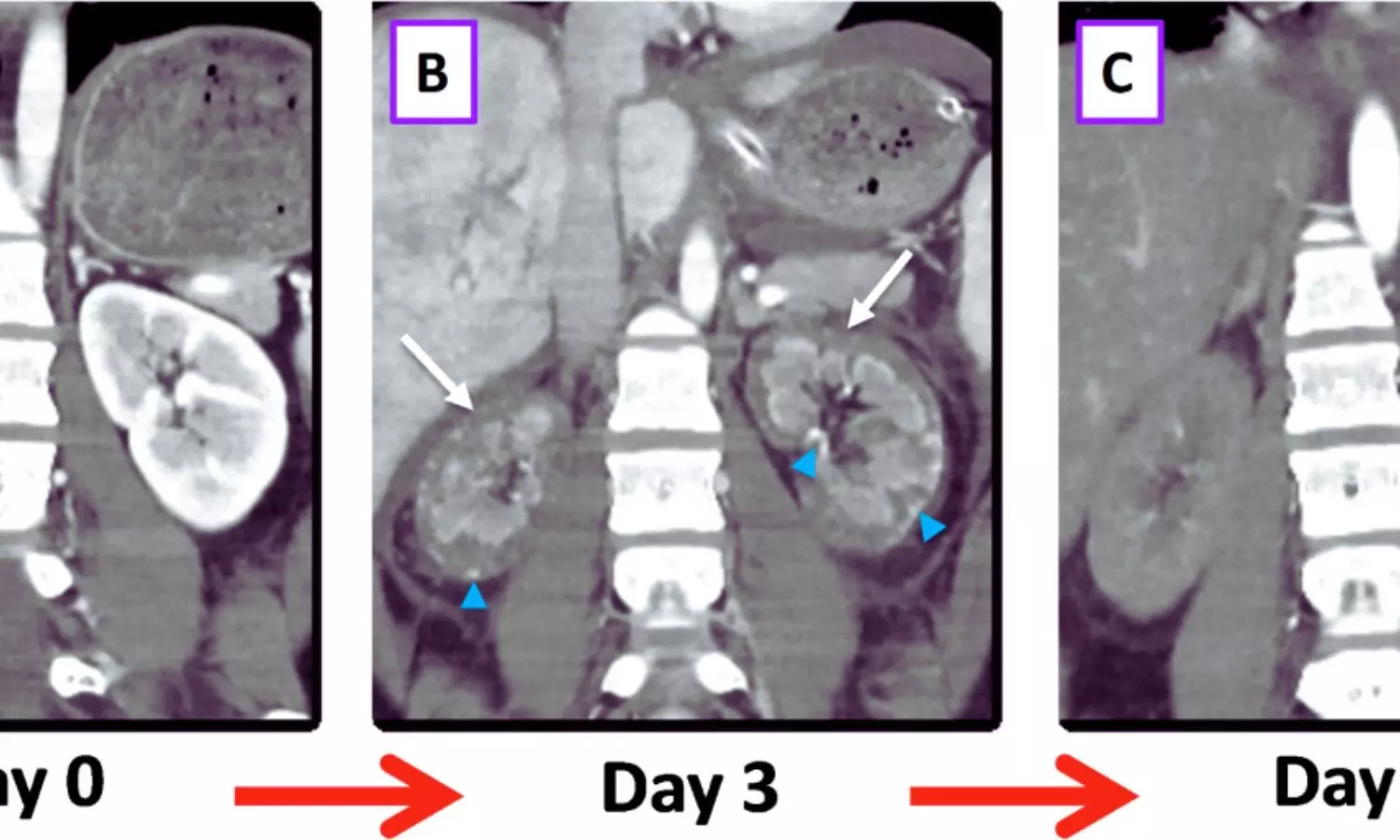
A contrast-enhanced CT scan revealed diffuse cortical enhancement defects in both kidneys, confirming the diagnosis of acute bilateral RCN. According to the authors, some cortical areas remained perfused, particularly in the subcapsular and juxtamedullary regions. Over time, her renal function partially recovered, and she was weaned off dialysis after two months. However, at one-year follow-up, her estimated glomerular filtration rate (eGFR) remained at 40 ml/min/1.73 m².
“The involvement of TXA in RCN development remains a subject of debate, particularly in trauma patients with concurrent bleeding. While TXA has been shown to reduce mortality in trauma patients, its prothrombotic effects cannot be ignored,” the researchers wrote. “In this case, several factors point toward TXA as a potential culprit, given the relatively mild bleeding, stable hemodynamics, and the exclusion of other thrombotic conditions. Additionally, the patient was on hormonal contraception, which may have contributed to the thrombotic event.”
“This case highlights the importance of considering TXA’s potential risks, particularly in patients with additional thrombotic risk factors. It also underscores the predictive value of kidney imaging in assessing RCN severity and guiding prognosis. To mitigate the risk of severe renal complications, further research is needed to establish clear guidelines for TXA use in non-obstetric bleeding scenarios,” they concluded.
Reference:
Berri, J., Quintrec Donnette, M., Millet, I. et al. Tranexamic acid-induced acute bilateral renal cortical necrosis in a young trauma patient: a case report and literature review. BMC Nephrol 26, 95 (2025). https://doi.org/10.1186/s12882-025-03982-y
