Plastic wound protector scores over surgical gauze in surgical site infection reduction: unveils clinical trial
Korea: In the realm of surgical procedures, minimizing postoperative complications remains a top priority for medical practitioners worldwide. Among the myriad of concerns, surgical site infections (SSIs) stand out as a significant threat to patient recovery and well-being. In a groundbreaking development, a randomized clinical trial (RCT) has shed light on a potential game-changer in the fight against SSIs in open gastrointestinal (GI) surgeries: the plastic wound protector.
The study, published in JAMA Surgery, has shown the effectiveness of plastic wound protectors in reducing surgical site infections in open gastrointestinal surgeries.
“In the RCT of 458 patients, the wound protector reduced SSI risk by 46.8% across bowel surgeries, with a 43.8% decrease for clean-contaminated wounds and 42.5% for superficial SSIs versus surgical gauze,” the researchers reported. “Its effect on contaminated wounds was less certain.”
SSIs are prevalent hospital-acquired infections with significant patient impacts and global healthcare burdens. The World Health Organization (WHO) recommends using wound protector devices in abdominal surgery as a preventive measure to lower SSI risk despite limited evidence. Considering this, Nina Yoo, The Catholic University of Korea, Seoul, Korea, and colleagues aimed to examine the efficacy of a dual-ring, plastic wound protector in reducing the SSI rate in open gastrointestinal (GI) surgery regardless of intra-abdominal contamination levels.
For this purpose, the researchers conducted a multicenter, patient-blinded, parallel-arm randomized clinical trial from 2017 to 2022 at 13 hospitals in an academic setting. Patients undergoing open abdominal bowel surgery (e.g. for bowel perforation) were eligible for inclusion.
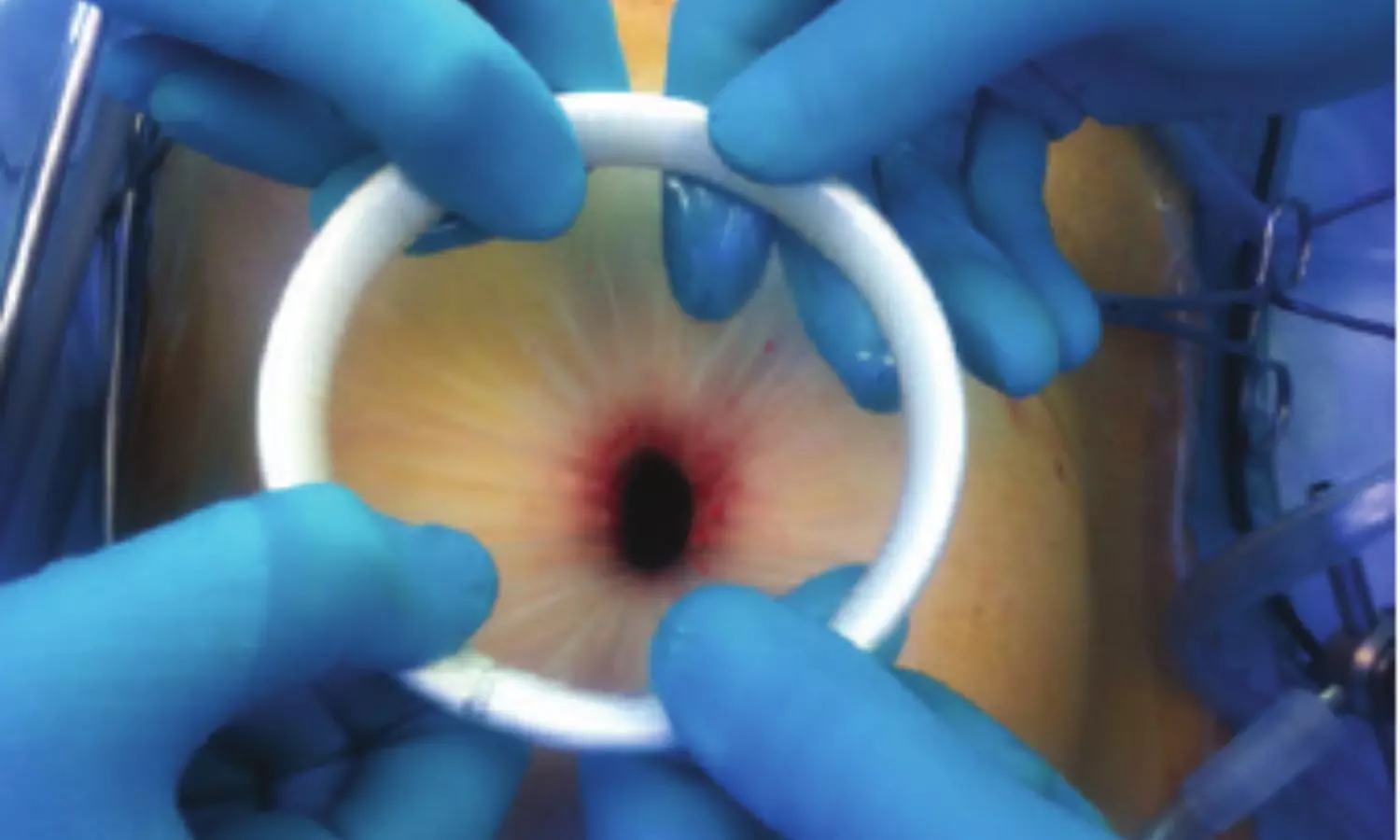
Patients were randomized in a 1:1 ratio to a dual-ring, plastic wound protector to protect the incision site of the abdominal wall (experimental group) or a conventional surgical gauze (control group). The primary endpoint was the SSI rate within 30 days of open GI surgery.
A total of 458 patients were randomized; after one was excluded from the control group, 457 were included in the intention-to-treat analysis (mean age, 58.4 years; 56.0% male; 74.6% with a clean-contaminated wound): 228 in the surgical gauze group and 229 in the wound protector group.
The researchers reported the following findings:
- The overall SSI rate in the intention-to-treat analysis was 15.7%.
- The SSI rate for the wound protector was 10.9% compared with 20.5% with surgical gauze.
- The wound protector significantly reduced the risk of SSI, with a relative risk reduction (RRR) of 46.81%.
- The wound protector significantly decreased the SSI rate for clean-contaminated wounds (RRR, 43.75%), particularly for superficial SSIs (RRR, 42.50%).
- Length of hospital stay was similar in both groups (mean, 15.2 versus 15.3 days), as were the overall postoperative complication rates (20.1% versus 18.8%).
In conclusion, the randomized clinical trial found a significant reduction in SSI rates when a plastic wound protector was used during open GI surgery versus surgical gaze, supporting the WHO recommendation for wound protector devices in abdominal surgery.
Reference:
Yoo N, Mun JY, Kye B, et al. Plastic Wound Protector vs Surgical Gauze for Surgical Site Infection Reduction in Open GI Surgery: A Randomized Clinical Trial. JAMA Surg. Published online April 24, 2024. doi:10.1001/jamasurg.2024.0765



