Intravitreal Aflibercept and Faricimab decreases ocular blood flow to optic nerve head and peripapillary retinal vessels: Study
Diabetic retinopathy (DR) is the primary cause of visual
impairment among working-age populations in industrialized nations. Vision loss
may result from various mechanisms, but the most prevalent cause is diabetic
macular edema (DME). The treatment landscape for DME has advanced significantly
over the past decade. Currently, the most frequently employed therapeutic approach
involves intravitreal administration of anti-vascular endothelial growth factor
(VEGF) agents, and the prognosis of patients with DME has markedly improved.
There are various commercially available anti-VEGF agents. Older options
include monoclonal antibodies such as ranibizumab and bevacizumab. While
ranibizumab and bevacizumab alone inhibit VEGF-A, aflibercept, a recombinant
fusion protein, inhibits VEGF-A, VEGF-B, and placental growth factor (Plgf),
and faricimab, a bispecific antibody, inhibits both VEGF-A and angiopoietin-2
(Ang-2).
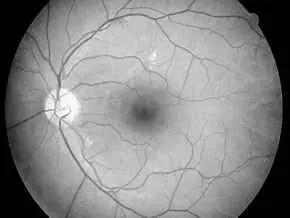
Laser speckle flowgraphy (LSFG) facilitates two-dimensional,
non-invasive measurements of perfusion at the optic nerve head (ONH), retina,
and choroid by utilizing the laser speckle phenomenon and has proven instrumental
in quantifying ocular blood flow in patients with DR, retinal vein occlusion,
age-related macular degeneration, or central serous chorioretinopathy. In this
study, authors aimed to evaluate and compare the effects of intravitreal
aflibercept (IVA) versus intravitreal faricimab (IVF) on blood flow in the
optic nerve head and retinal vessels of the peripapillary region using LSFG in
patients with DME. This was the first study to investigate the effect of
intravitreal faricimab on ocular perfusion and compare the effects of different
anti-VEGF agents on ocular blood flow one month after injection.
This study included 20 eyes of 18 patients treated with IVA
and 15 eyes of 11 patients treated with IVF for DME. The mean blur rate (MBR)
of the ONH and retinal artery and vein of the peripapillary region were
measured using LSFG at baseline and 1 month after injection. Central retinal
thickness (CRT) and best-corrected visual acuity (BCVA) were measured for all
patients.
CRT decreased significantly in both IVA-treated (p = 0.0003)
and IVF-treated groups (p = 0.0004). Some of the MBR-related parameters of the
ONH, such as MBR of all areas (MA), MBR of vascular areas (MV), and MBR of
tissue areas (MT), decreased significantly 1 month after IVA and IVF compared
to baseline values (MA of IVA, p < 0.0001; MT of IVA, p = 0.0220; MA of IVF,
p = 0.0002; MT of IVF, p = 0.0461). MBR of the retinal artery (MBR-A) and vein
(MBR-V) also decreased significantly 1 month after IVA and IVF compared with
baseline values (MBR-A of IVA, p = 0.0002; MBR-V of IVA, p = 0.0010; MBR-A of
IVF, p = 0.0368). No significant difference in ocular perfusion was observed
between the IVA-treated and IVF-treated groups.
In conclusion, the findings demonstrated that both IVA and
IVF resulted in a decrease in ocular blood flow to the optic nerve head and
peripapillary retinal vessels, as evaluated using the LSFG. This decrease was
associated with a reduction in CRT and improvement in BCVA. No significant
difference was observed in MBR reduction between the IVA-treated and
IVF-treated groups. Study findings warrant further long-term investigations to
reveal differences in ocular circulation modifications between aflibercept and
faricimab.
Source: Mizukami et al; Clinical Ophthalmology 2024:18
https://doi.org/10.2147/OPTH.S476307