Elevated D-Dimer and Non-Glucocorticoid Therapies Risk Factors for Thromboembolic Events in Dermatomyositis: Study
A recent study found that the
prevalence of thromboembolic events is increased in individuals with Dermatomyositis
with elevated D-dimer levels and the lack of glucocorticoid therapy as per the
results that were published in the Journal of Inflammation Research.
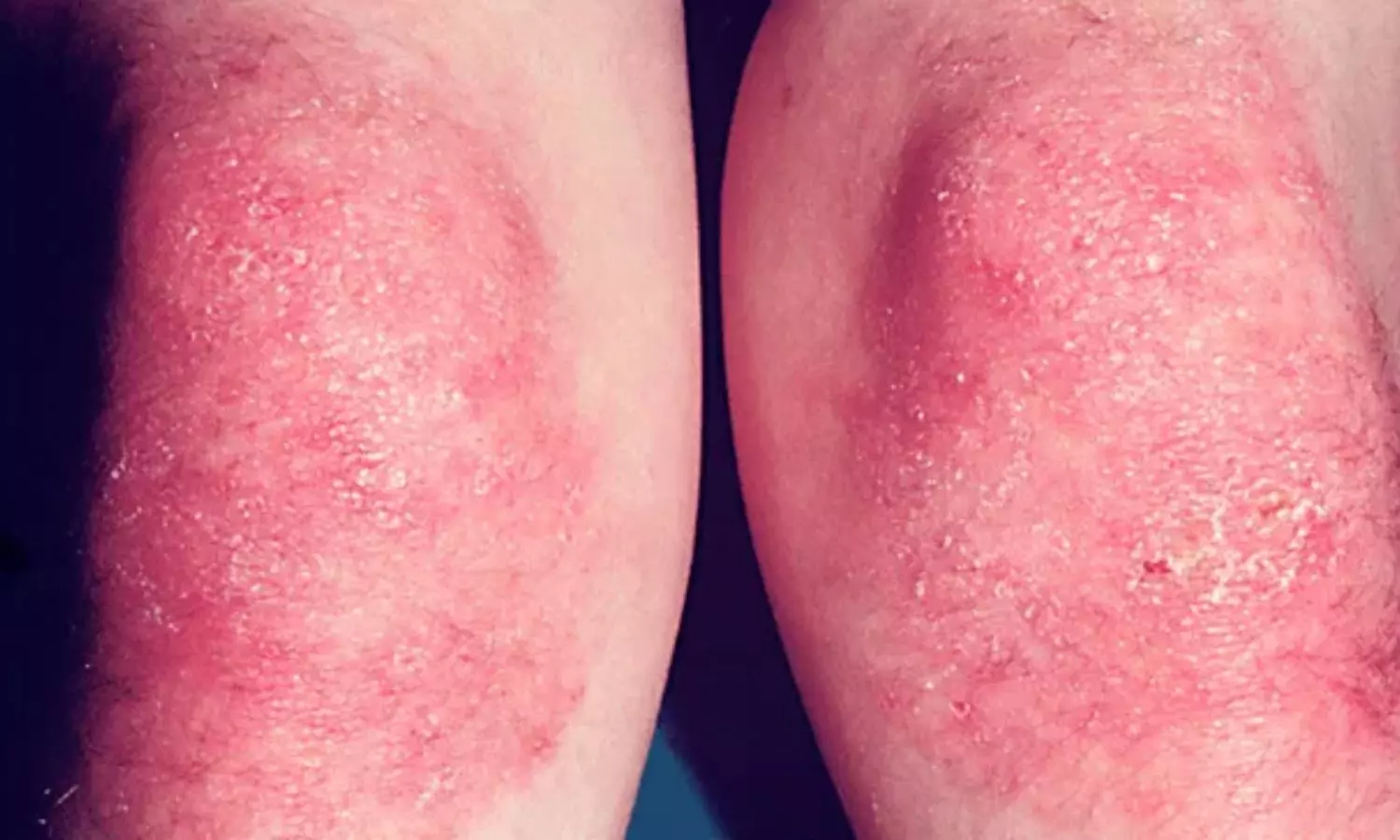
Dermatomyositis (DM) is an
autoimmune disorder and is a common clinical subtype of Idiopathic inflammatory
myopathies. Clinically it presents with skin manifestations, which can affect
the lungs, joints, esophagus, and heart. DM is characterized by a
hypercoagulable state associated with endothelial dysfunction, leading to Thromboembolic
events (TEs). There is uncertainty about the risk factors that cause TEs in DM.
Hence Chinese researchers conducted a retrospective analysis to investigate the
prevalence of TEs in DM in Southeast China and identify the independent
predictors.
A 10-year retrospective analysis included
patients aged ≥18 with at least one ICD code for DM. The European League
Against Rheumatism/American College of Rheumatology 2017 classification
criteria were used to identify a well-defined, relatively homogenous population
of individuals with DM. Individuals with a score ≥7.5 without a muscle biopsy
or ≥8.7 with a muscle biopsy, along with at least one of the three skin
criteria, were considered eligible for the study. TEs were determined by ultrasonography,
computed tomography, magnetic resonance imaging, or angiogram.
About 543 patients hospitalized
for DM within the past 10 years were analyzed retrospectively and compared with
patients with DM with and without TEs for demographic, clinical, and laboratory
characteristics. The independent predictors were analyzed using multivariate
logistic regression analysis. The diagnostic performance was calculated by a
receiver operating curve (ROC).
Findings:
- Twenty-two (4.1%) patients with DM had TEs,
including 12 (54.5%) with venous thromboembolism and 10 (45.5%) with arterial
thromboembolism. - Multivariate logistic regression analysis revealed
that glucocorticoid therapy was a protective factor for patients with DM
developing TEs, whereas increased D-Dimer was a risk factor. - The combined ROC analysis of glucocorticoid
therapy and D-Dimer indicated high diagnostic values in distinguishing patients
with both DM and TEs from patients without TEs, with 86.4% sensitivity, 98.9%
specificity, and 0.983 area under the ROC curve (95% CI 0.962– 1.000, P<
0.001).
Thus, the study concluded that
the prevalence of TE was less in DM. However, the lack of glucocorticoid
therapy and increased levels of D-dimer were risk factors for the development
of TEs in DM patients. Hence, the researchers suggested early screening of
thromboembolic events in all dermatomyositis individuals by evaluating the risk
factors. Physicians should also consider adding anticoagulants in DM patients
to prevent TEs.
Further reading: Prevalence
and Risk Factors of Thromboembolic Events in Dermatomyositis in China: A
10-Year Retrospective Analysis. Doi: https://doi.org/10.2147/JIR.S482055