Cutaneous Leishmaniasis Misdiagnosed as Diabetic Foot: Case Study Calls for Increased Vigilance in Endemic Areas
Saudi Arabia: Cutaneous leishmaniasis (CL) is a parasitic infection transmitted by sandflies, affecting millions worldwide. While the disease typically presents as an ulcerated nodule at the site of parasite inoculation, its clinical manifestations can vary significantly. A recent case published in Acta Dermatovenerologica Croatica highlights an unusual presentation of CL that was initially misdiagnosed as diabetic foot, emphasizing the need for heightened awareness and vigilance in diagnosing foot ulcers, particularly in endemic areas.
A 75-year-old man from Afghanistan, residing in a region endemic to CL, presented with a large, progressive necrotic ulcer on his left foot that had persisted for a year. The ulcer was accompanied by pain, but the patient reported no history of trauma or chronic systemic diseases. Despite multiple visits to healthcare providers in his village, where he was repeatedly diagnosed with diabetic foot, the ulcer showed no improvement after several rounds of dressing applications. Blood tests, including fasting blood sugar, revealed normal levels, which raised suspicion for a diagnosis other than diabetic foot.
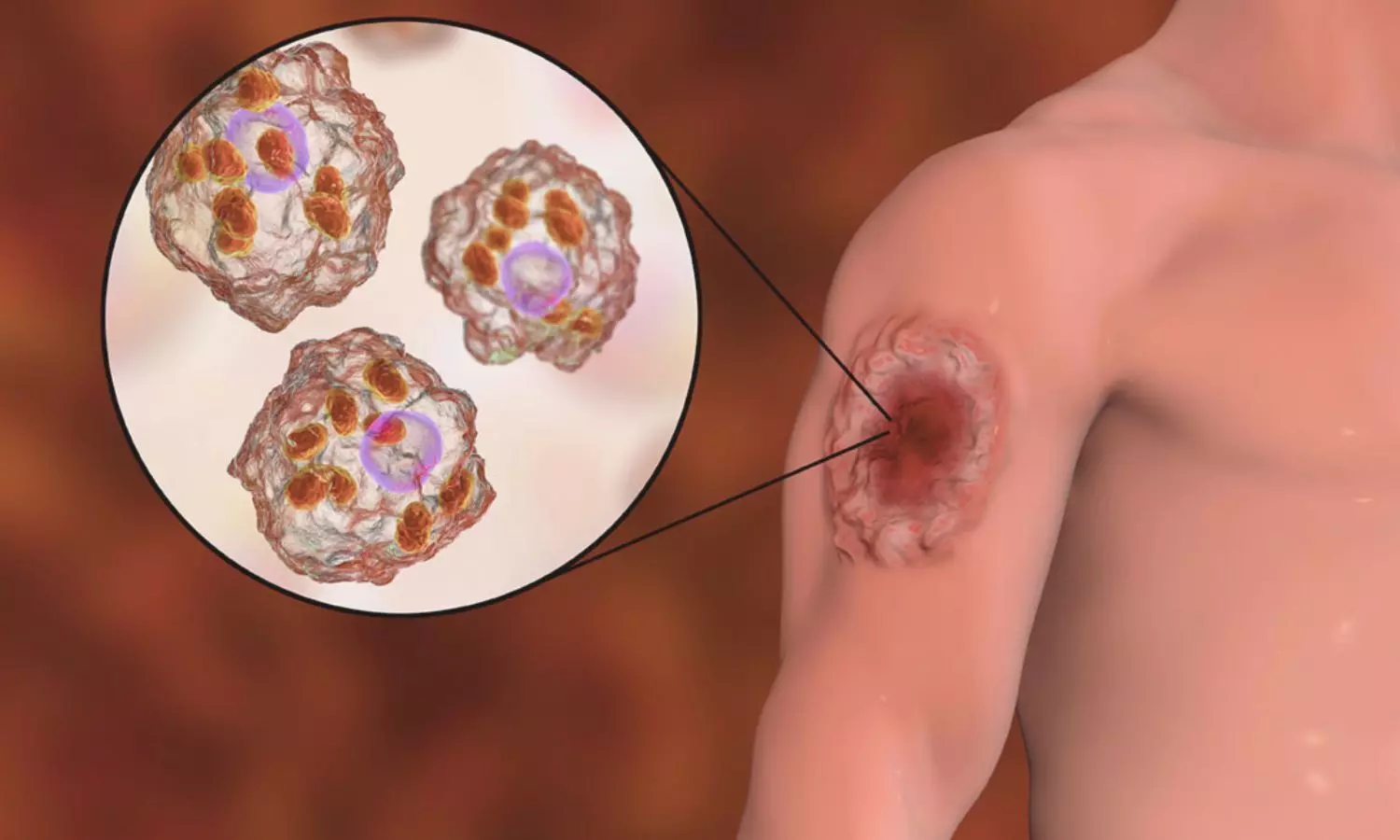
Given the patient’s geographic location and the ulcer’s persistence, CL was considered, and subsequent diagnostic tests confirmed the diagnosis. A slit skin smear and skin biopsy revealed the presence of Leishmania amastigotes in the dermal histiocytic infiltrates, confirming the diagnosis of cutaneous leishmaniasis. The patient is now undergoing treatment with systemic sodium stibogluconate (pentostam), a standard therapy for CL.
Leishmaniasis, particularly CL, is a major health concern in various parts of the world, with over 1.5 million cases reported annually. While the classic form of CL is often easily diagnosed, the disease can present in unusual locations, such as the scalp, genital region, or palms and soles. Foot involvement, though rare, can be mistaken for other conditions that cause ulcerations, such as leprosy, vasculitis, or diabetic foot ulcers. The misdiagnosis of CL as diabetic foot is not uncommon, especially in endemic areas where CL is less frequently considered in differential diagnoses.
This case underscores the importance of considering CL in the differential diagnosis of chronic ulcers, especially in patients from endemic regions. Clinicians should be aware of the possibility of CL when evaluating persistent foot ulcers, particularly when typical treatments for diabetic foot fail. Routine diagnostic biopsies can be invaluable in such cases, aiding in identifying specific pathogens like Leishmania. Early diagnosis and appropriate treatment are crucial to managing CL effectively and preventing further complications.
Reference:
Al Aboud K, Al Aboud A. Cutaneous Leishmaniasis Masquerading as Diabetic Foot: A Call for Vigilance. Acta Dermatovenerol Croat. 2024 Nov;32(2):120-121. PMID: 39803740.
