Clopidogrel Better Than Aspirin for Long-Term Monotherapy After PCI, reports research
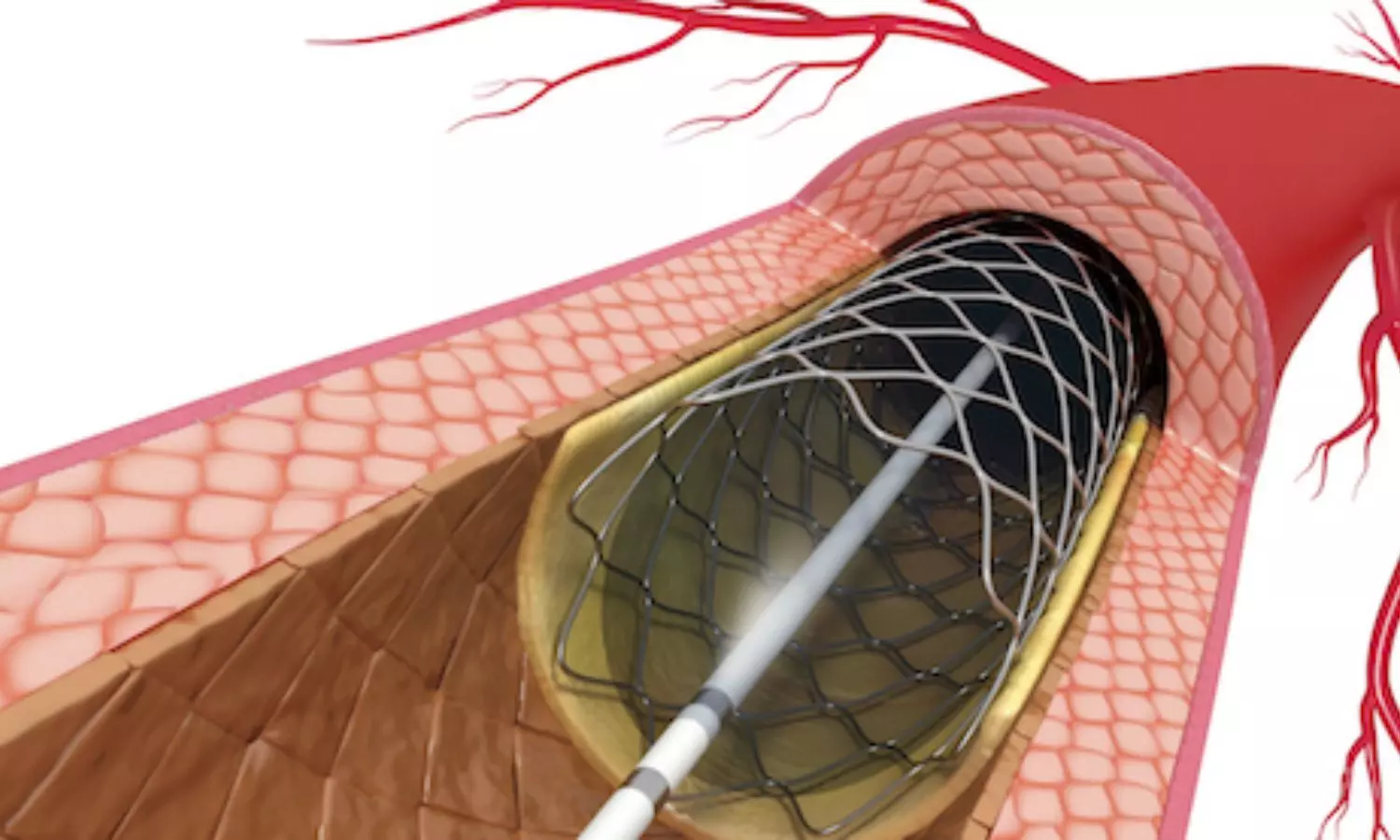
For prolonged antithrombotic treatment after percutaneous coronary intervention (PCI), clopidogrel monotherapy was more effective and at least as safe as aspirin monotherapy in a high-risk population, a Korean randomized trial showed.
The optimal strategy for long-term antiplatelet maintenance for patients who underwent percutaneous coronary intervention (PCI) remains uncertain. This study aimed to compare the efficacy and safety of clopidogrel versus aspirin monotherapy in patients who completed a standard duration of dual antiplatelet therapy (DAPT) following PCI with drug-eluting stents. In this multicentre, randomised, open-label trial, patients aged 19 years or older at high risk of recurrent ischaemic events (previous myocardial infarction at any time before enrolment, medication-treated diabetes, or complex coronary lesions) who completed a standard duration of DAPT after PCI were randomly assigned (1:1) to receive clopidogrel (75 mg once a day) or aspirin (100 mg once a day) oral monotherapy at 26 sites in South Korea.
The primary endpoint was the cumulative incidence of a composite of death from any cause, myocardial infarction, or stroke, assessed in the intention-to-treat population. Adverse events were captured as part of the secondary endpoints. It is closed to accrual and extended follow-up is ongoing. Findings: Between Aug 10, 2020, and July 31, 2023, 5542 patients were assessed for eligibility and 5506 were randomly assigned (2752 to clopidogrel monotherapy and 2754 to aspirin monotherapy).
The median time between PCI and randomisation was 17·5 months (IQR 12·6–36·1 months). During a median follow-up period of 2·3 years (IQR 1·6–3·0), the primary endpoint occurred in 92 patients in the clopidogrel group and 128 patients in the aspirin group (Kaplan–Meier estimated 3-year incidence 4·4% [95% CI 3·4–5·4] vs 6·6% [5·4–7·8]; hazard ratio 0·71 [95% CI 0·54–0·93]; p=0·013). Death from any cause occurred in 50 patients in the clopidogrel group and 70 in the aspirin group (2·4% [1·6–3·1] vs 4·0% [2·9–5·0] at 3 years; 0·71 [0·49–1·02]); myocardial infarction in 23 patients in the clopidogrel group and 42 in the aspirin group (1·0% [0·6–1·4] vs 2·2% [1·4–2·9] at 3 years; 0·54 [0·33–0·90]); and stroke in 23 in the clopidogrel group and 29 in the aspirin group (1·3% [0·7–2·0] vs 1·3% [0·8–1·7] at 3 years; 0·79 [0·46–1·36]).
There was no difference in the risk of bleeding between the clopidogrel and aspirin groups (3·0% [2·0–3·9] vs 3·0% [2·2–3·9] at 3 years; 0·97 [0·67–1·42]). Clopidogrel was not associated with a higher incidence of any adverse event compared with aspirin. Among patients who were at high risk of recurrent ischaemic events and who completed the standard duration of DAPT following PCI, clopidogrel monotherapy, compared with aspirin monotherapy, significantly reduced the cumulative incidence of a composite of death from any cause, myocardial infarction, and stroke, without an apparent increase in the risk of bleeding.
Reference:
Efficacy and safety of clopidogrel versus aspirin monotherapy in patients at high risk of subsequent cardiovascular event after percutaneous coronary intervention (SMART-CHOICE 3): a randomised, open-label, multicentre trial. Choi, Ki Hong et al. The Lancet, Volume 0, Issue 0
