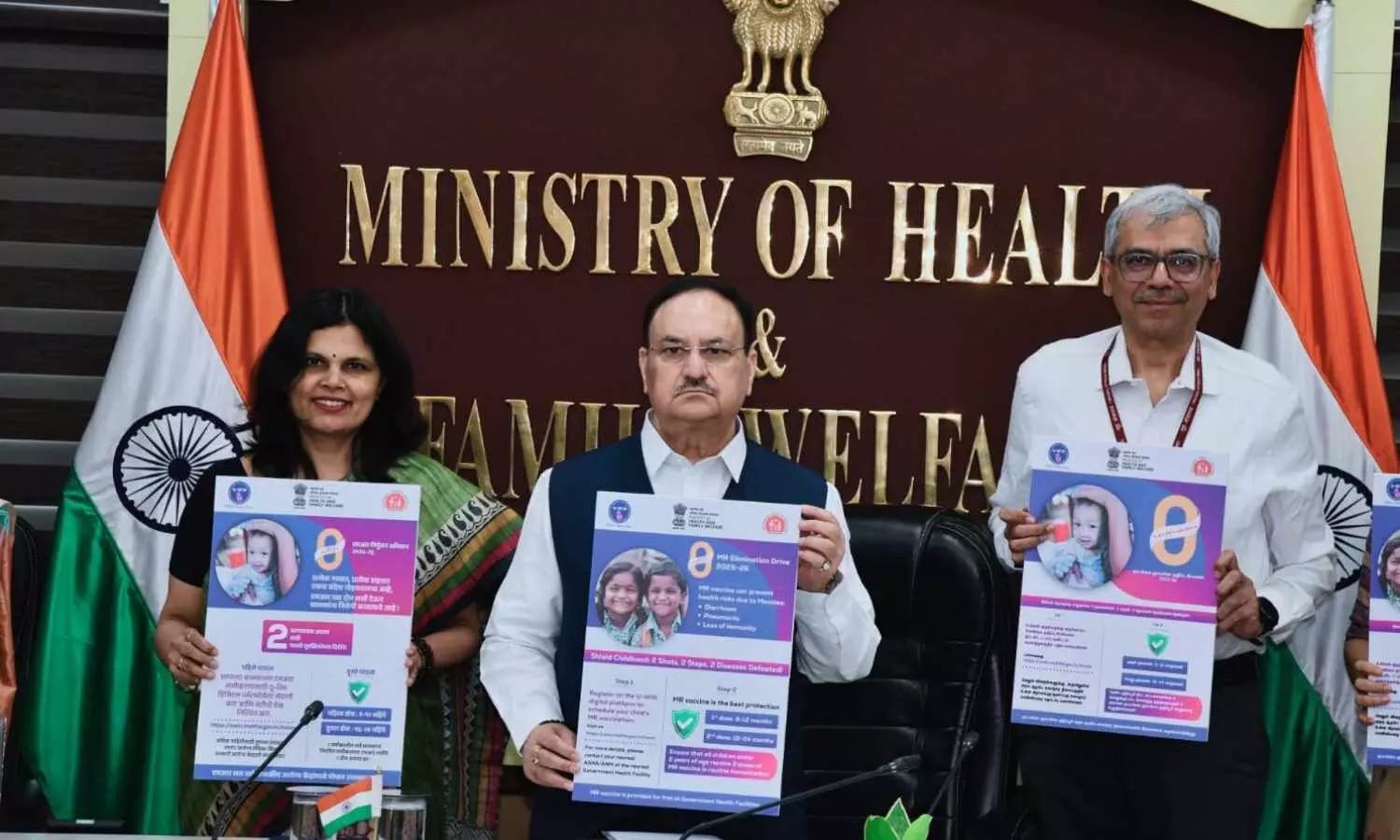
New Delhi: Union Minister of Health and Family Welfare, Shri Jagat Prakash Nadda, recently virtually launched the National Zero Measles-Rubella Elimination campaign 2025-26 on the first day of the World Immunization Week (24-30 April), marking a significant step towards India’s goal of eliminating Measles and Rubella by 2026.
On the occasion, Union Health Minister released multi-language M-R IEC materials (posters, radio jingles, MR elimination and official U-WIN launch film) for creating awareness in the communities. These IEC materials were also shared with all States/UTs for adaptation and rollout during the MR Elimination Campaign 2025-26.
Addressing the occasion, Shri JP Nadda stated that, “Today is momentous occasion as the launch of Measles-Rubella elimination campaign 2025-26 marks an opportunity to achieve 100% immunization coverage to provide high quality lifestyle to children by administering them with the two doses of Measles and Rubella vaccine.” Noting that this disease is of a highly contagious nature that hampers not only children’s life but also cause misery to their parents, Shri Nadda underlined the importance of ensuring that not even a single child is left behind.
Also Read:Fatty liver is preventable, reversible through healthy lifestyle and food habits: JP Nadda
The Union Health Minister congratulated the Ministry for getting recognition with the prestigious Measles and Rubella Champion Award by the Measles and Rubella Partnership in 2024. He highlighted that “332 districts in the country have reported zero measles cases and 487 districts have reported zero rubella cases during January- March 2025 which underscores the progress achieved in the goal of M-R elimination.”
Shri Nadda highlighted the need for keeping the IDSP activated and strengthening surveillance. “We have to target the elimination of M-R in the same way as Polio and Maternal and Neonatal Tetanus elimination was achieved”, he stated. He urged the states and UTs to be attentive, alert, and proactive and work with a ‘ACT NOW’ policy.
Shri Nadda also urged the State Ministers and Chief Medical Officers to hold public and press meetings where people at large can be informed about the vaccination drive through active Jan Bhagidari. He also called upon States for an inclusive participation of all MLAs, MPs, local and Panchayat heads to spread awareness about the vaccination against Measles and Rubella. He also urged the frontline workers to reach out to remote and hard to reach areas, slums, migratory population, areas with frequent outbreaks. “We have to reach out to people in the last mile to ensure that we achieve 100% coverage”, he stated. He also emphasized on the need for coordinating with line ministries. He concluded his address by stating that “if we work and act from today, we will be able to achieve success tomorrow.”
Background:
Measles and Rubella are highly infectious viral diseases that can lead to serious illnesses, lifelong complications, and even death. Due to their high infection rate, India has set a goal to eliminate these diseases by 2026. Under the Universal Immunization Programme (UIP), two doses of the Measles-Rubella (MR) vaccine are provided free of cost to all eligible children, at 9-12 months and 16-24 months of age, respectively. Currently, India’s MR vaccination coverage stands at 93.7% for the first dose (2024-25 HMIS data) and 92.2% for the second dose.
In 2024, India has recorded a remarkable decline of 73% in Measles cases and a 17% reduction in Rubella cases in comparison with 2023.
India’s plan for eliminating measles and rubella includes a comprehensive framework:
Immunization: Achieve and maintain high population immunity with > 95% vaccination coverage with 2 doses of measles and rubella containing vaccines in each district of the country.
Surveillance: Sustain a sensitive and timely case-based surveillance system for measles & rubella.
Outbreaks: Ensure adequate preparedness and timely response to measles and rubella outbreaks.
Linkages: Strengthen support and linkages to achieve the above strategic objectives.
Demand Generation for Vaccination: Focused mass awareness campaigns to mitigate the risks of non-vaccination and dispel myths related to MR vaccine for addressing vaccine hesitancy and increasing coverage.
In recognition of country’s exceptional efforts in prevention of Measles and Rubella, India was awarded the prestigious Measles and Rubella Champion Award by the Measles and Rubella Partnership at the American Red Cross Headquarters in Washington D.C. on March 6, 2024.
Under the Universal Immunization Programme (UIP), India runs world’s largest vaccination programme for pregnant women and children – reaching out to 2.9 crore pregnant women and 2.6 crore newborns annually. This provides protection against 12 vaccine preventable diseases (VPDs) such as Polio, Measles, Rubella, Diphtheria, Tetanus, Rotavirus diarrhoea, Hepatitis B among others. U-WIN digital platform for vaccination, launched by the Hon’ble Prime Minister is being utilized extensively to record vaccination events, generate vaccination certificate and book appointment for vaccination across the country.
India’s Universal Immunization Programme, has been instrumental in reducing mortality rates and controlling infectious diseases among children under five years of age. From 2014 to 2020, under-5 mortality rates dropped from 45 to 32 per 1,000 live births (Sample Registration System – 2020). Since 2014, under UIP, over 6 new vaccines have been introduced including MR vaccine.
Smt. Punya Salila Srivastava, Union Health Secretary; Dr Rajiv Bahl, Secretary, Dept. of Health Research and DG, ICMR; Smt. Aradhana Patnaik, Addl. Secretary and Mission Director (NHM), Union Health Ministry; Smt. Meera Srivastava, Joint Secretary, Union Health Ministry, Additional Commissioner (Immunization), Additional Chief Secretaries, Principal Secretaries (Health), Mission Directors (NHM) and State Immunization Officers from States/UTs had joined the virtual launch event.
Also Read:Union Health Minister JP Nadda launches Ayushman Bharat scheme in Odisha