Exercise reduces risk of common postpartum pelvic floor problems
Powered by WPeMatico
Powered by WPeMatico

USA: Researchers have found in a randomized trial that among adults with septic shock, the beta-blocker esmolol showed superior outcomes by significantly reducing 28-day mortality compared to both standard care and landiolol. The randomized trial data were presented at the CHEST Annual Meeting, highlighting the potential role of esmolol in improving survival and key clinical parameters in patients with septic shock.
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

A new study published in the journal of Nature Pediatric Research revealed that by the age of 4, low maternal vitamin D may have a major negative impact on the neurocognitive development of children.
An important micronutrient that is necessary for bone formation and calcium homeostasis management is vitamin D. In addition to its critical role in skeletal growth, vitamin D has several biological activities that are essential to neurodevelopment and function. These include regulating the metabolism of neurotrophic and neurotoxic factors, regulating gene expression, signaling in cell differentiation and synaptic formation, and providing protection during inflammation of the brain. Among Indians, especially pregnant women, vitamin D deficiency is very common despite the country’s abundance of sunshine.
There is little research on the connection between a mother’s vitamin D levels during pregnancy and the cognitive function of her unborn child. Pregnancy-related hypovitaminosis D can impact fetal brain development and result in neurocognitive problems. After adjusting for confounding factors, this study examined the relationship between vitamin D levels during pregnancy and the neurocognitive functioning of 289 mother-child couples.
Prenatal serum 25-hydroxyvitamin D (25(OH)D) concentrations were assessed during the first and third trimesters, and at age 4, the offspring were subjected to a neurocognitive evaluation using the Behavior Rating Inventory of Executive Function—Preschool Version (BRIEF-P), subtests of the Developmental Neuropsychological Assessment-II (NEPSY-II), and the Wechsler Preschool and Primary Scale of Intelligence—Fourth Edition (WPPSI-IV). Data on lifestyle, mother mental health, obstetrics, sociodemographics, and parental intellectual performance were gathered.
According to the adjusted regression models, lower Visual-Motor Precision of the NEPSY-II was linked to inadequate 25(OH)D levels during pregnancy. The behavioral and cognitive tests found worse executive functioning in the third trimester was linked to insufficient 25(OH)D levels. In particular, poorer scores were noted in the metacognitive index, inhibition on the BRIEF-P, and working memory on the WPPSI-IV.
Overall, sustaining enough prenatal 25(OH)D may encourage the best possible neurocognitive development in the early years. The requirement for appropriate vitamin D during pregnancy is highlighted by the fact that third-trimester deficit was connected to lower executive functioning, working memory, inhibition, and metacognitive skills, while inadequate levels of 25-hydroxyvitamin D throughout pregnancy were linked to poor visual-motor accuracy.
Source:
Voltas, N., Cendra-Duarte, E., Canals, J., & Arija, V. (2025). Vitamin D status during pregnancy and child neurocognitive functioning at 4 Years. Pediatric Research, 1–10. https://doi.org/10.1038/s41390-025-04258-9
Powered by WPeMatico

Scientists from the Gray Faculty of Medical & Health Sciences at Tel Aviv University introduced an innovative gene therapy method to treat impairments in hearing and balance caused by inner ear dysfunction. According to the researchers, “This treatment constitutes an improvement over existing strategies, demonstrating enhanced efficiency and holds promise for treating a wide range of mutations that cause hearing loss.”
The study was led by Prof. Karen Avraham, Dean of the Gray Faculty of Medical & Health Sciences, and Roni Hahn, a PhD student from the Department of Human Molecular Genetics and Biochemistry. The study was conducted in collaboration with Prof. Jeffrey Holt and Dr. Gwenaëlle Géléoc from Boston Children’s Hospital and Harvard Medical School and was supported by the US-Israel Binational Science Foundation (BSF), the National Institutes of Health/NIDCD and the Israel Science Foundation Breakthrough Research Program. The study was featured on the cover of the journal EMBO Molecular Medicine.
Prof. Avraham explains: “The inner ear consists of two highly coordinated systems: the auditory system, which detects, processes, and transmits sound signals to the brain, and the vestibular system, which enables spatial orientation and balance. A wide range of genetic variants in DNA can affect the function of these systems, leading to sensorineural hearing loss and balance problems. Indeed, hearing loss is the most common sensory impairment worldwide, with over half of congenital cases caused by genetic factors. In this study, we aimed to investigate an effective gene therapy for these cases using an approach that has not been applied in this context before.”
Roni Hahn: “Gene therapy has emerged as a powerful therapeutic approach in recent years and is now being applied to a range of genetic disorders, including spinal muscular atrophy (SMA) and Leber congenital amaurosis (LCA), as well as in cancer immunotherapy approaches such as CAR T-cell therapy. One of the treatment strategies includes the use of engineered viral vectors, in which the native DNA is replaced with a functional sequence of the target gene. These vectors utilize the virus’s natural ability to enter cells to deliver the correct gene sequence, thereby restoring normal function. Many gene therapies utilize adeno-associated viruses (AAVs) to introduce therapeutic genetic material into target cells, and AAV-based gene therapy for hearing loss is currently in clinical trials, showing promising early results.
In this study, the researchers investigated a mutation in the CLIC5 gene, which is essential for maintaining the stability and function of hair cells in the auditory and vestibular systems. Deficiency of this gene causes progressive degeneration of hair cells, initially leading to hearing loss and later resulting in balance problems. The researchers utilized an advanced, structurally optimized version of the AAV vector, the self-complementary AAV (scAAV). They found that this vector achieved faster and more efficient transduction of hair cells compared to traditional AAV methods, requiring a lower dose to achieve a similar therapeutic effect. In treated animal models, this approach prevented hair cell degeneration and preserved normal hearing and balance.
In summary, Prof. Avraham states: “In this study, we applied an innovative treatment approach for genetic hearing loss and found that it improves therapeutic effectiveness while also addressing combined impairments in hearing and balance. We anticipate that these findings will pave the way for developing gene therapies to treat a wide range of genetically caused hearing disorders.”
Reference:
Seung Hyun Jang, Hyeong Gi Song, Jinsei Jung, Heon Yung Gee, Recent Preclinical and Clinical Advances in Gene Therapy for Hereditary Hearing Loss, Molecules and Cells, 10.1016/j.mocell.2025.100285, (100285), (2025).
Powered by WPeMatico
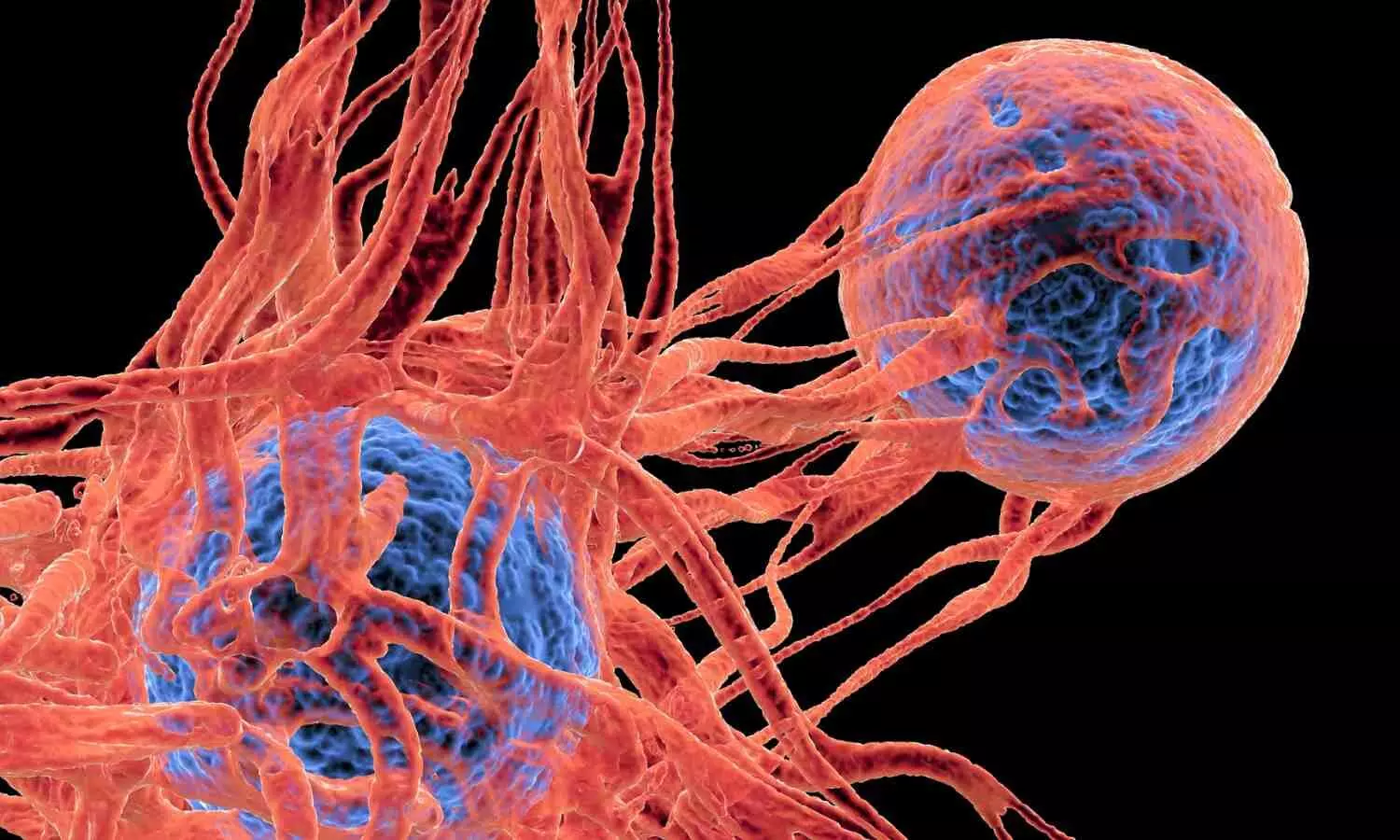
Scientists have developed a promising cancer therapy that uses LED light and ultra-thin flakes of tin to eliminate cancer cells while protecting healthy tissue. Unlike traditional chemotherapy and other invasive treatments, this new method avoids the painful side effects patients often endure.
The breakthrough comes from a partnership between The University of Texas at Austin and the University of Porto in Portugal, made possible through the UT Austin Portugal Program. The collaboration aims to make light-based cancer therapies more accessible and affordable. Current versions of these treatments rely on expensive materials, specialized lab setups, and powerful lasers that can sometimes damage surrounding tissue. By switching to LEDs and introducing tin-based “SnOx nanoflakes” (“Sn” is the chemical symbol for tin), the researchers have created a safer and potentially low-cost alternative.
“Our goal was to create a treatment that is not only effective but also safe and accessible,” said Jean Anne Incorvia, a professor in the Cockrell School of Engineering’s Chandra Family Department of Electrical and Computer Engineering and one of the leaders on the project. “With the combination of LED light and SnOx nanoflakes, we’ve developed a method to precisely target cancer cells while leaving healthy cells untouched.”
In a recent study published in ACS Nano, the approach proved highly effective against both colorectal and skin cancer cells. After only 30 minutes of exposure, the LED-driven treatment destroyed up to 92% of skin cancer cells and 50% of colorectal cancer cells, while leaving healthy human skin cells unharmed. The results highlight the therapy’s precision and safety.
Cancer remains the second-leading cause of death worldwide, and many existing treatments come with severe side effects. Scientists across the globe are exploring new methods to make therapies safer and more targeted. One of the most promising is near-infrared photothermal therapy, which uses light to heat and destroy cancer cells without the need for surgery or toxic drugs. This principle forms the foundation of the UT Austin-Portugal team’s research.
Having shown strong early results, the researchers are now focused on understanding how light and heat interact in the process and on testing other materials that might enhance the treatment. They also plan to design practical medical devices that can deliver the therapy directly to patients.
“Our ultimate goal is to make this technology available to patients everywhere, especially places where access to specialized equipment is limited, with fewer side effects and lower cost,” said Artur Pinto, a researcher at the Faculty of Engineering of the University of Porto and lead researcher of the project in Portugal. “For skin cancers in particular, we envision that one day, treatment could move from the hospital to the patient’s home. A portable device could be placed on the skin after surgery to irradiate and destroy any remaining cancer cells, reducing the risk of recurrence.”
Incorvia and Pinto first teamed up through the UT Austin Portugal Program in 2021. Since then, they have exchanged visits between Texas and Portugal and combined their expertise to explore how two-dimensional materials can be used to advance cancer therapies.
Building on their success, the team recently received additional funding through the UT Austin Portugal Program to create an implant for breast cancer patients using the same LED and nanoflake technology. Their continued collaboration could pave the way for more personalized, affordable, and pain-free cancer treatments in the near future.
Reference:
Hui-Ping Chang, Filipa A. L. S. Silva, Eva Nance, José R. Fernandes, Susana G. Santos, Fernão D. Magalhães, Artur M. Pinto, Jean Anne C. Incorvia. SnOx Nanoflakes as Enhanced Near-Infrared Photothermal Therapy Agents Synthesized from Electrochemically Oxidized SnS2 Powders. ACS Nano, 2025; 19 (38): 33749 DOI: 10.1021/acsnano.5c03135
Powered by WPeMatico

Researchers have determined in a new study that the application of automated insulin delivery (AID) systems in children with type 1 diabetes (T1D) results in gains in blood glucose control, such as decreases in glycated hemoglobin (HbA1c), increases in time-in-range (TIR), and reductions in risks of both hyperglycemia and hypoglycemia. The study was published in JAMA Pediatrics by Hannah S. and colleagues.
A PRISMA-guided systematic review and meta-analysis was performed, with literature searched in MEDLINE, Embase, CINAHL, and Cochrane Central between January 2017 and March 2025. There were randomized clinical trials (RCTs) of youth aged 6 to 18 years with T1D comparing AID systems for over 48 hours in outpatient care with other insulin regimens. Screening, extraction, and quality assessments were conducted by two independent reviewers. Random-effects models were employed to calculate pooled efficacy results, with a main interest in HbA1c and TIR.
Results
After screening 2,363 accessed citations, 11 RCTs with 901 participants with available HbA1c data and 10 RCTs with 786 participants with available TIR data were included.
The average intervention duration was 31 weeks, and the median age of participants was 12 years (range 10.8–15.9 years).
Within participants, 51% were women, mean baseline HbA1c was 8.4% (SD 1.1%), and mean baseline TIR was 51% (SD 9%).
In comparison with conventional insulin regimens, AID systems lowered HbA1c by −0.41% (95% CI: −0.58% to −0.25%; I² = 39%) and increased TIR by 11.5% (95% CI: 9.3%–13.7%; I² = 23%).
Nighttime TIR rose by 19.7% (95% CI: 17.0%–22.4%; I² = 36%).
Moreover, AID use decreased hypoglycemia (<3.9 mmol/L) time by −0.32% (95% CI: −0.60% to −0.03%; I² = 18%) and hyperglycemia (>10 mmol/L) time by −10.8% (95% CI: −14.4% to −7.2%; I² = 55%), especially nocturnal (−14.4%; 95% CI: −19.9% to −8.9%; I² = 79%).
There were no differences in adverse events between groups, and only two studies included quality of life outcomes.
This review found that the application of AID systems among adolescents with type 1 diabetes improves glycemic control by decreasing HbA1c, improving TIR, and decreasing rates of hypoglycemia and hyperglycemia without inducing additional adverse events.
Reference:
de Visser HS, Waraich S, Chhabra M, et al. Automated Insulin Delivery Systems and Glucose Management in Children and Adolescents With Type 1 Diabetes: A Systematic Review and Meta-Analysis. JAMA Pediatr. Published online September 08, 2025. doi:10.1001/jamapediatrics.2025.2740
Powered by WPeMatico

A recent clinical study published in the journal of Polski Merkuriusz Lekarski revealed that daily vitamin E supplementation (100 mg) positively influenced female hormonal indicators, particularly estradiol and luteinizing hormone (LH), potentially improving infertility treatment outcomes. Early-cycle supplementation showed greater increases in these hormones when compared with mid-cycle supplementation, indicating enhanced hormonal activity.
The study enrolled 40 women aged between 18 and 35 years, all receiving infertility treatment. The participants were divided into 2 groups, where the Group A received vitamin E starting on the 4th day of their menstrual cycle, representing early-cycle supplementation and Group B received taking vitamin E during the middle of the cycle, around the expected time of ovulation. Blood samples were analyzed using an immunoassay system (Cobas E 411) to determine the hormone levels before and after supplementation.
The results demonstrated a clear increase in serum vitamin E levels in both groups following supplementation, confirming that even short-term use significantly elevates antioxidant levels in the body. Also, the study found a significant rise in estradiol and LH concentrations after treatment when compared with baseline values. These two hormones play a critical role in ovulation and fertility regulation.
Estradiol is essential for follicle development and endometrial preparation for implantation. Its elevation indicates improved ovarian activity. Luteinizing hormone, meanwhile, is responsible for triggering ovulation and its increase suggests a higher likelihood of successful egg release.
Also, early-cycle supplementation (Group A) showed better hormonal responses than mid-cycle supplementation (Group B). Statistical analysis revealed that estradiol levels were significantly higher in Group A (P=0.04), while luteinizing hormone levels also showed a notable rise (P=0.02). This implies that initiating vitamin E earlier in the menstrual cycle enhances the body’s natural hormonal rhythm, potentially improving fertility outcomes.
While follicle-stimulating hormone (FSH) and prolactin levels showed modest changes, the marked improvements in estradiol and LH are particularly significant. This research explained that vitamin E, being a potent antioxidant, may help stabilize cellular membranes and reduce oxidative stress in ovarian tissues, promoting better hormonal signaling and follicular health.
Overall, the findings suggest that short-term vitamin E supplementation at 100 mg/day positively influences female reproductive hormones, especially when started early in the menstrual cycle. Further studies on larger populations are imperative to confirm the long-term benefits and potential clinical applications of this vitamin-based approach.
Source:
Assi, M. A., Shamran, S. G., Mahdi, K. A., & Al-Fahham, A. A. (2025). Effect of short duration vitamin E supplementation on some reproductive hormones in infertile women. Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego, 53(5), 587–591. https://doi.org/10.36740/Merkur202505101
Powered by WPeMatico

South Africa: A new phase 2b clinical trial has found that Bacille Calmette–Guérin (BCG) revaccination does not offer protection against sustained Mycobacterium tuberculosis (TB) infection in adolescents. The study, conducted by Dr. Alexander C. Schmidt and colleagues from the Gates Medical Research Institute, was published in the New England Journal of Medicine and aimed to assess whether BCG revaccination could reduce the risk of sustained TB infection in a population previously testing negative for TB and HIV.
This latest investigation was prompted by earlier findings suggesting that while BCG revaccination may not prevent primary TB infection, it could reduce the risk of persistent infections. To further explore this potential benefit, researchers carried out a double-blind, randomized, placebo-controlled trial involving 1,836 adolescents between the ages of 10 and 18 years in South Africa. Participants were HIV-negative and tested negative on the QuantiFERON-TB Gold (QFT) test at the start of the study.
Participants were randomly assigned to receive either the BCG vaccine or a placebo and were monitored over a median follow-up period of 30 months. The primary objective was to assess the rate of sustained QFT test conversion, defined as an initial positive QFT result confirmed by two additional positive results at three and six months.
Based on the study, the researchers reported the following findings:
The authors concluded that while the vaccine was generally well tolerated and immunogenic, it did not provide measurable protection against sustained M. tuberculosis infection. They noted that the absence of efficacy in preventing infection casts doubt on the likelihood of BCG revaccination offering disease protection.
These findings emphasize the continued need for novel TB vaccines that are effective in preventing both infection and disease, particularly in high-risk populations such as adolescents in TB-endemic regions.
Reference:
Schmidt AC, Fairlie L, Hellström E, Luabeya Kany Kany A, Middelkoop K, Naidoo K, Nair G, Gela A, Nemes E, Scriba TJ, Cinar A, Frahm N, Mogg R, Kaufman D, Dunne MW, Hatherill M; BCG REVAX Study Team. BCG Revaccination for the Prevention of Mycobacterium tuberculosis Infection. N Engl J Med. 2025 May 8;392(18):1789-1800. doi: 10.1056/NEJMoa2412381. PMID: 40334156; PMCID: PMC12061034.
Powered by WPeMatico
