CVD Risk in Women After 40: Cardiovascular disease (CVD) is the leading cause of death in individuals with type 2 diabetes (T2D) and hypertension. (1) Women in the menopausal transition phase (aged 40–50) are particularly vulnerable yet often underrepresented in preventive care strategies. This transitional period is marked by significant hormonal fluctuations that amplify cardiovascular risk, making primary prevention critically important. (2)
In India, the National Family Health Survey (NFHS)-4 and 5 report that diabetes prevalence among women peaks at 7.8% in the 45–49 age group, with hypertension affecting 31.2% in the same group. Data show that women with diabetes face a 50% higher risk of fatal CVD events compared to men with diabetes (Relative Risk: 3.50 [2.0–4.53] vs. 2.06 [1.81–2.34]). Despite this heightened risk, they are frequently undertreated and inadequately targeted in cardiovascular prevention programs. (2)
Role of Aspirin in Primary Prevention of ASCVD in Diabetes and Hypertension: Diabetes promotes exaggerated platelet activation and aggregation, largely driven by hyperglycemia-induced oxidative stress and inflammation. This is compounded by insulin resistance, which increases intracellular calcium and further enhances platelet activity. As endothelial function deteriorates and lipid-rich plaques become vulnerable to rupture, the overall cardiovascular risk escalates. Aspirin offers cardioprotective benefits in this setting by irreversibly inhibiting COX-1, thereby reducing thromboxane A2 production and platelet aggregation. (3)
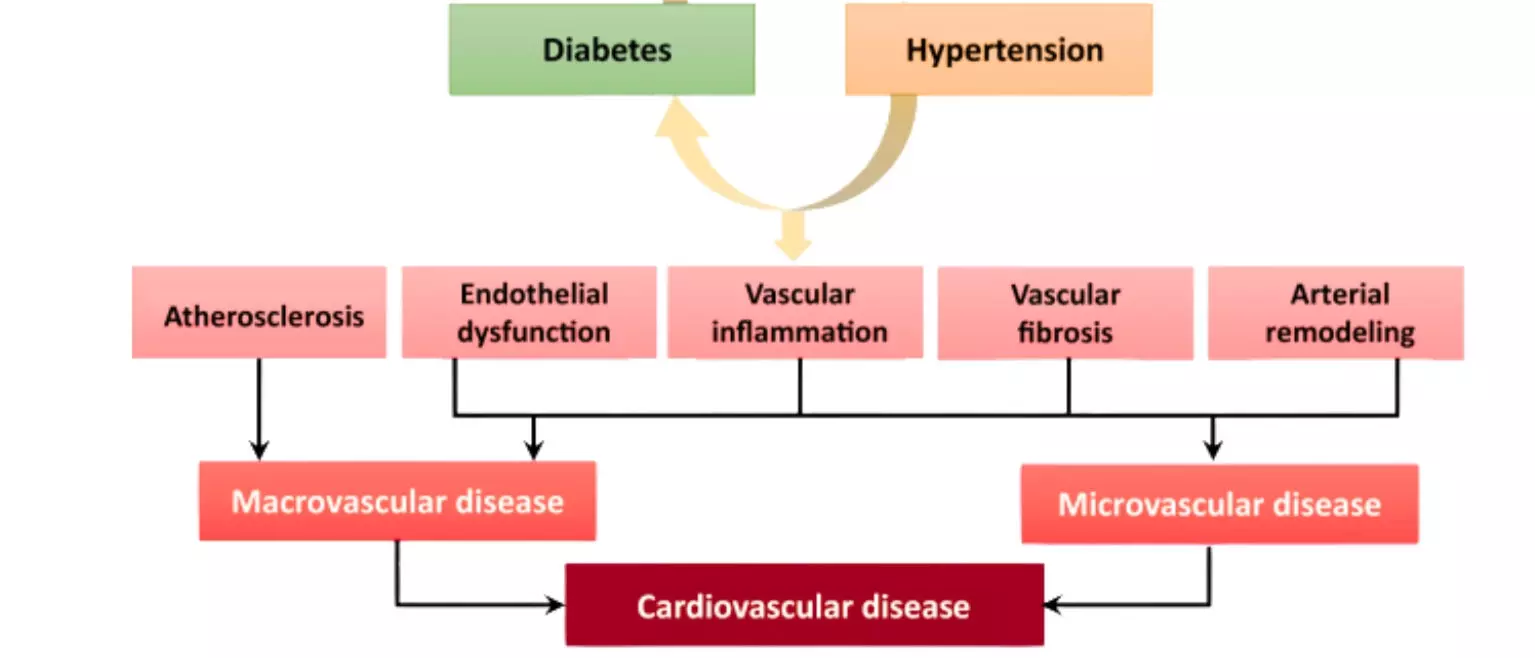
The following diagram illustrates shared risk pathways leading to cardiovascular disease in patients with diabetes and hypertension.
Figure: Pathophysiological Link Between Common Risk Factors- T2D, HT & CVD. Adapted from Petrie JR et al. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34(5):575–584. doi:10.1016/j.cjca.2017.12.005
Aspirin in Primary Prevention- Women’s Health Study: Women’s Health Study which included 39,876 women aged ≥45 years without prior cardiovascular disease, demonstrated a 17% reduction in total stroke risk with alternate-day low-dose aspirin (100 mg) over 10 years. These findings support a selective approach to aspirin use in women aged ≥45 with elevated CVD risk. (4)
Aspirin in CV Prevention- Review of Guidelines: Accordingly, the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease also suggests considering low-dose aspirin (75–100 mg/day) for primary prevention in adults aged 40–70 years who are at high ASCVD risk but not at increased risk of bleeding. (5) Similarly, the DCRM 2.0 (Diabetes, Cardiorenal, and Metabolic Diseases Multispecialty Practice Recommendations) Multispecialty Task Force (2024) supports aspirin use (75–100 mg daily) for primary prevention in individuals with at least two major risk factors, such as elevated lipoprotein(a), T2D, hypertension, a family history of premature coronary artery disease, or a coronary artery calcium (CAC) score >100. (6)
Implementation to Clinical Practice–Brief Case Profile: To illustrate practical application, consider a 48-year-old Indian woman undergoing menopausal transition with a history of T2D and hypertension. Her lab values show elevated LDL-C (145 mg/dL), low HDL-C (38 mg/dL), and a high lipoprotein(a) level (55 mg/dL)—a recognized risk factor especially prevalent in South Asian populations.
Given her multiple major cardiovascular risk factors, she would be an appropriate candidate for low-dose aspirin therapy (75–100 mg/day) for primary prevention—provided a structured bleeding risk assessment is conducted. Tools like the Aspirin-Guide app can assist clinicians in individualized decision-making regarding aspirin initiation.
Conclusion: Women aged 40–50 years undergoing menopausal transition and living with type 2 diabetes and hypertension face a significantly heightened risk of cardiovascular disease, particularly in the Indian context where additional risk factors like elevated lipoprotein(a) and abnormal waist-hip ratio are common. Despite this, they remain underrepresented in preventive strategies. Low-dose aspirin therapy, when guided by current recommendations and individualized risk assessments, offers a valuable primary prevention tool to reduce cardiovascular events in this high-risk group.
References:
1. Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34(5):575-584. doi:10.1016/j.cjca.2017.12.005
2. Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006;332(7533):73-78. doi:10.1136/bmj.38678.389583.7C
3. Della Bona, Roberta et al. “Aspirin in Primary Prevention: Looking for Those Who Enjoy It.” Journal of clinical medicine vol. 13,14 4148. 16 Jul. 2024, doi:10.3390/jcm13144148
4. Pradhan AD, Cook NR, Manson JE, Ridker PM, Buring JE. A randomized trial of low-dose aspirin in the prevention of clinical type 2 diabetes in women. Diabetes Care. 2009;32(1):3-8. doi:10.2337/dc08-1206
5. Cho, Leslie et al. “Summary of Updated Recommendations for Primary Prevention of Cardiovascular Disease in Women: JACC State-of-the-Art Review.” Journal of the American College of Cardiology vol. 75,20 (2020): 2602-2618. doi:10.1016/j.jacc.2020.03.060
6. Handelsman, Yehuda et al. “DCRM 2.0: Multispecialty practice recommendations for the management of diabetes, cardiorenal, and metabolic diseases.” Metabolism: clinical and experimental vol. 159 (2024): 155931. doi:10.1016/j.metabol.2024.155931