Abdominal vs. Perineal Surgery for Recurrent Rectal Prolapse: Research Highlights Higher Recurrence with Perineal Approach
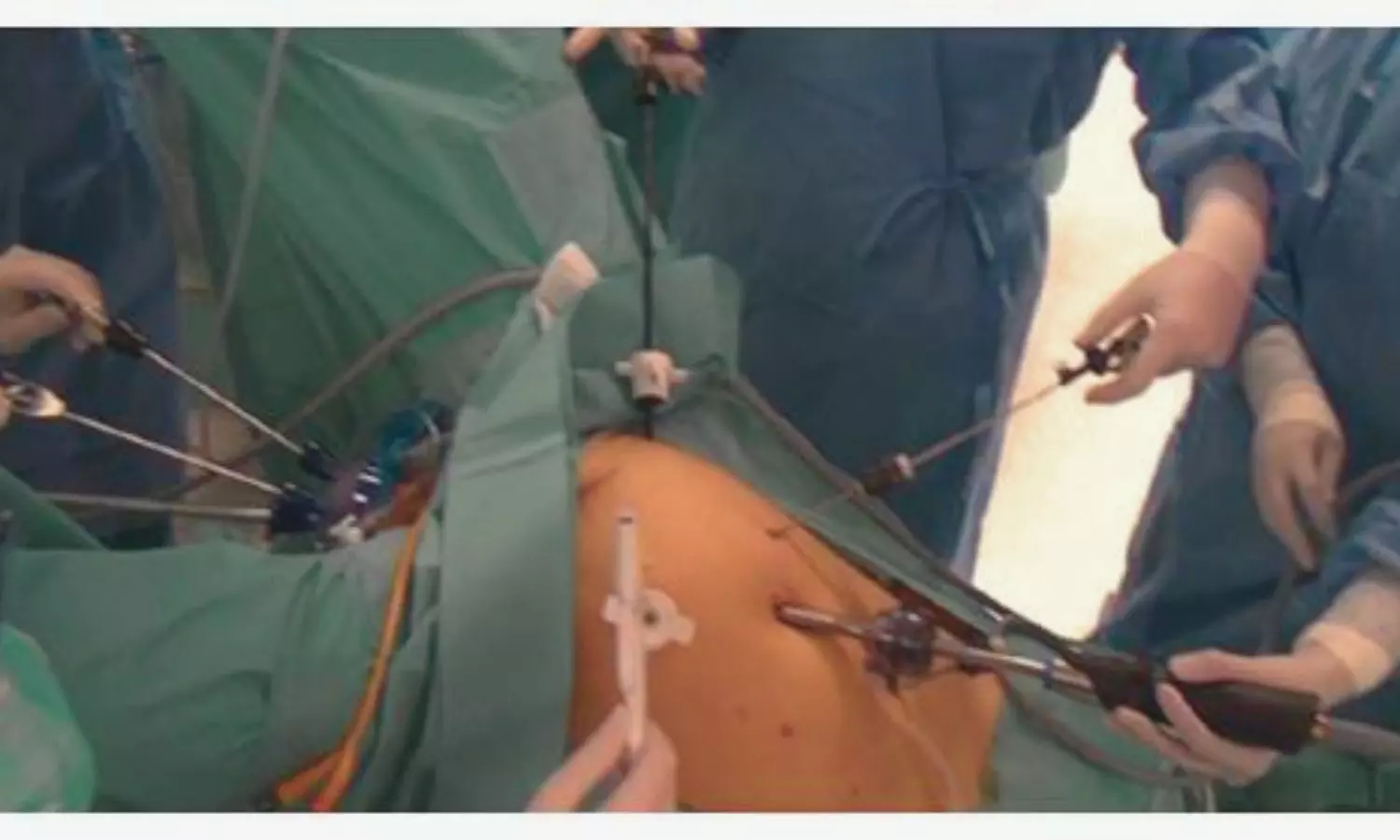
Italy: A recent systematic review and meta-analysis have provided valuable insights into the effectiveness of perineal and abdominal surgical approaches for treating recurrent external rectal prolapse. The analysis revealed that the recurrence rate for the abdominal approach in treating recurrent external rectal prolapse was 15.6%, notably lower than the 27.9% observed with the perineal approach.
“Although both surgical techniques had comparable complication rates and hospital stays, the findings indicate that abdominal surgery may provide better patient outcomes,” the researchers wrote in the International Journal of Colorectal Disease.
External rectal prolapse, characterized by the protrusion of the rectum through the anal opening, often necessitates surgical intervention, especially in recurrent cases. At the same time, surgery remains the most effective treatment, recurrence rates reported in the literature range from 6% to 27%. Surgeons typically select between perineal and abdominal approaches based on patient characteristics and clinical considerations. The perineal approach, including procedures like the Altemeier and Delorme techniques, is often favored for elderly or high-risk patients due to its lower perioperative morbidity and suitability for regional anesthesia. In contrast, the abdominal approach, encompassing laparoscopic and open rectopexy techniques, offers better anatomical support and durability, potentially reducing recurrence rates.
Against the above background, Giacomo Fuschillo, Colorectal Surgery, Department of Advanced Medical and Surgical Sciences, Università Degli Studi Della Campania “Luigi Vanvitelli”, Naples, Italy, and colleagues aimed to compare the effectiveness of abdominal and perineal approaches in the surgical management of recurrent external rectal prolapse.
For this purpose, the researchers conducted a systematic search of PubMed and Embase the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. They reviewed studies published between January 2000 and May 2024 that reported surgical outcomes for recurrent external rectal prolapse.
The primary focus was on recurrence rates at the last available follow-up, while secondary outcomes included surgical complications and the length of postoperative hospitalization.
The study led to the following findings:
- The analysis included nine studies with a total of 531 patients.
- The recurrence rate was 26.3% at a mean follow-up of 30.5 months.
- Recurrence after perineal surgery was 27.9%.
- Recurrence after abdominal surgery was 15.6%.
- The odds ratio (OR) for recurrence between the two approaches was 0.66.
- The OR for surgical complications was 1.44.
- The standardized mean difference (SMD) for hospital stay length was 0.49.
This meta-analysis found that the recurrence rate after the perineal approach was nearly twice that of the abdominal approach in the surgical treatment of recurrent external rectal prolapse. However, the comparison between the two techniques did not reveal a statistically significant difference.
“While the perineal approach offers the benefits of a shorter hospital stay and lower morbidity, further randomized trials are necessary to establish the most effective surgical strategy for these patients,” the researchers concluded.
Reference:
Fuschillo, G., Selvaggi, L., Cuellar-Gomez, H. et al. Comparison between perineal and abdominal approaches for the surgical treatment of recurrent external rectal prolapse: a systematic review and meta-analysis. Int J Colorectal Dis 40, 26 (2025). https://doi.org/10.1007/s00384-024-04771-z
Powered by WPeMatico