Exercise and healthy eating behaviour together provide best protection against cardiovascular diseases: Study

Researchers at the University of Jyväskylä’s Faculty of Sport and Health Sciences have found that women who exhibit disturbed eating behaviours and engage in low physical activity tend to have more central body fat and a higher risk of metabolic low-grade inflammation. This condition increases the risk of cardiovascular diseases, which become more prevalent after menopause. However, the combined effect of exercise and healthy eating behaviour offers the most effective protection against inflammation and may also reduce it after menopause.
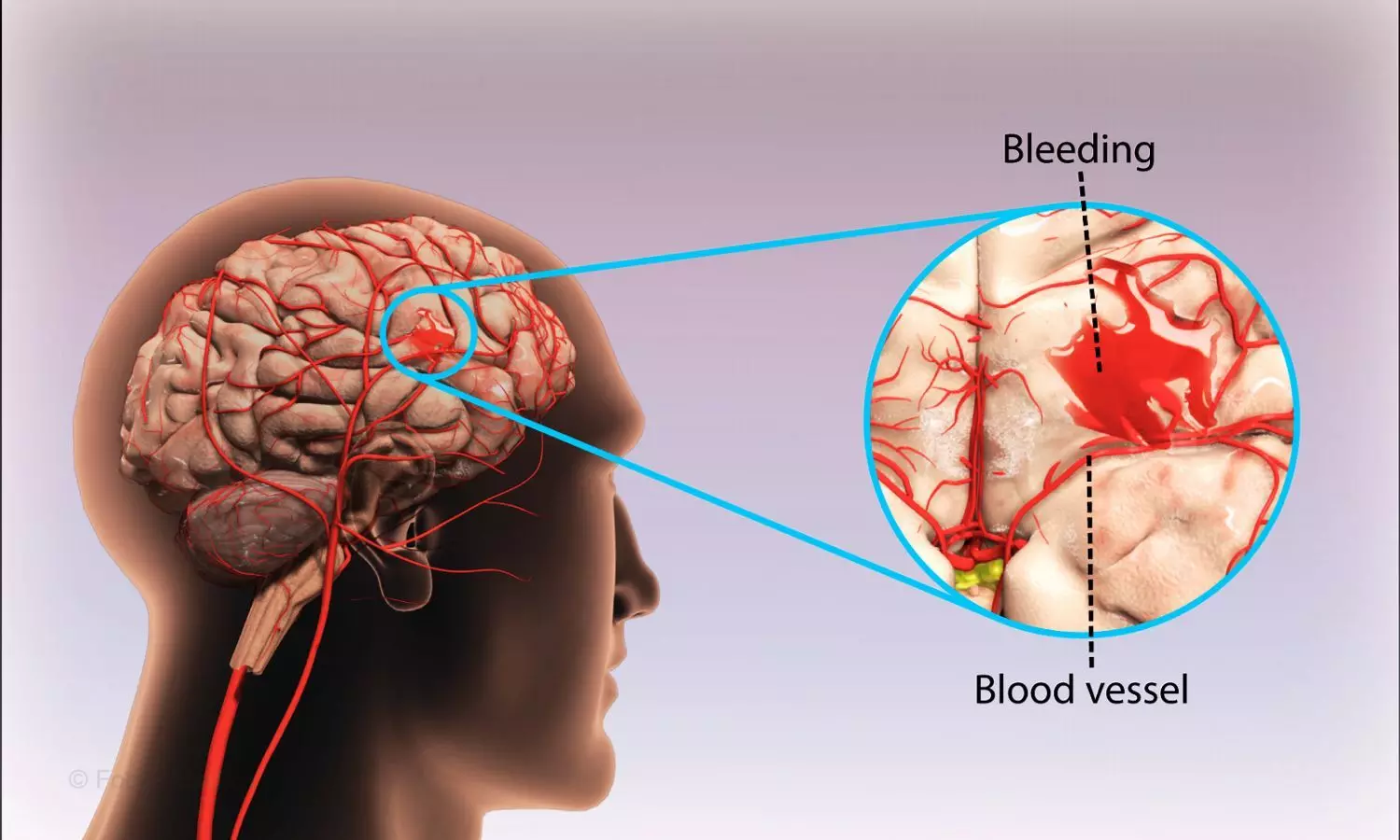
Body fat distribution changes as menopause progresses and estrogen levels decrease, causing the adipose tissue concentrated in the hips and thighs to gradually shift to the midsection as harmful visceral fat. This predisposes women to low-grade inflammation and cardiovascular diseases, which increase significantly after menopause.
A study by the University of Jyväskylä investigated the connection between health behaviours and low-grade inflammation. Health behaviours in this study include sleeping, eating and physical activity and related disorders. For example, disordered eating behaviour refers to a situation in which a person may restrict their eating to control their weight or body shape. They may also have a limited understanding of what they are allowed to eat or what their body should look like.
“In line with previous studies, a higher amount of visceral fat was, as expected, associated with low-grade inflammation,” says Hannamari Lankila, a doctoral researcher at the Faculty of Sport and Health Sciences. “Visceral fat accumulated in the midsection secretes cytokines that increase inflammation, and this can increase the risk of metabolic diseases.”
The results show that those individuals who exhibit more disordered eating behaviour, as well as those who were physically less active, had more visceral fat, and thus the risk of low-grade inflammation was also higher.
When eating and physical activity behaviours were examined together, higher physical activity was associated with lower visceral fat, especially in those women who did not display disordered eating behaviour.
“The connection was weaker, meaning that the protective effect of even a high amount of exercise was less if the individual had eating-related difficulties,” Lankila continues. “Surprisingly, sleep was not a significant factor in this equation.”
Previous research has shown that both exercise and various diets and foods are associated with low-grade inflammation to some extent, but the combined effects of health behaviours during menopause have not previously been studied. The menopause phase is significant, however, as women live more than a third of their lives after menopause on average. During this period, the risk of metabolic and cardiovascular diseases increases significantly.
The study highlighted the link between visceral fat and inflammation, especially in women with low physical activity. Both physical activity and flexible eating behaviour can help reduce visceral fat, but the effect is likely to be more effective when the two are combined.
“It’s good to remember that even after menopause, it is possible to reduce the accumulation of harmful visceral fat and thus prevent metabolic and cardiovascular diseases that may result from it,” Lankila concludes.
The study also assessed sleep duration and perceived sleep quality as well as physical activity with the help of self-report questionnaires. Eating behaviour was assessed with the Eating Disorder Examination Questionnaire (EDE-Q), which consisted of 28 questions. The questionnaire can be used to assess whether a person restricts their eating and whether they have specific concerns about their eating, weight or body shape. In addition, the participants’ age, income level and use of menopausal hormone therapy were considered.
Reference:
Lankila, H., Kekäläinen, T., Hietavala, EM. et al. A mediating role of visceral adipose tissue on the association of health behaviours and metabolic inflammation in menopause: a population-based cross-sectional study. Sci Rep 15, 1999 (2025). https://doi.org/10.1038/s41598-025-85134-8
Powered by WPeMatico