Lucknow: Granting relief to a doctor who was first accused of medical negligence resulting in malignancy and then hitting the patient with a motorcycle, the Allahabad High Court recently quashed the criminal proceedings against him.
Apart from Dr. Srivastava, the HC bench comprising Justice Shree Prakash Singh also quashed the criminal proceedings against Advocate Ramesh Kumar Srivastava, as it held that the prosecution was instituted with mala fide and malicious intent.
“…the facts and circumstances of the present matter is indicative that the first information report has been lodged with a malafide and malicious intention,” observed the HC bench in its order dated April 10, 2025.
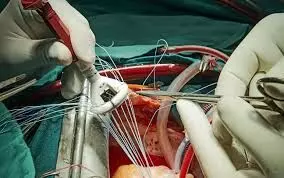
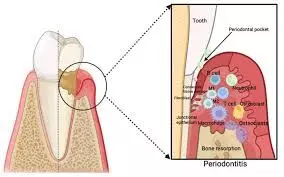
The case stems from a First Information Report (FIR) lodged on 8 February 2007 by a complainant who alleged that Dr. Srivastava had performed a negligent surgery at the Prathmik Swasthya Kendra, Malihabad, resulting in malignancy. Following this, when she was sitting on a dharna, both the doctor and the advocate had allegedly hit her with a motorcycle and threatened her with dire consequences. This led to a fracture in her left elbow, alleged the complainant. Ultimately, the complainant/patient died of cancer in 2009.
Based on the complaint, charges under Sections 325 and 506 IPC were framed based on the chargesheet dated 18 December 2007 and consequently, the Chief Judicial Magistrate, Lucknow, issued summoning orders on 19 December 2007 and 22 July 2013.
Also Read: HC quashes SC, ST Act, Negligence charges against MBBS doctor in gallbladder surgery death case
Challenging these proceedings, the doctor and the advocate approached the HC bench, and their counsel, Sanjay Kumar Srivastav, argued that the FIR was lodged after an unexplained delay of nearly two months. He also argued that the charge sheet was filed hurriedly without proper investigation and emphasized that the protection witnesses, including the complainant’s husband, were not eyewitnesses and relied solely on hearsay.
The applicants claimed that Dr. Srivastava was on emergency and Pulse Polio duty at P.H.C. Malihabad on the date of the alleged incident, and Ramesh Kumar Srivastava (another accused) was present at the High Court, where several of his cases were listed, supported by affidavits of four advocates.
It was further submitted that no evidence of medical negligence was found against Dr. Srivastava in an earlier departmental inquiry by Dr. M.K. Gupta, Deputy CMO, on 29.08.2006.
The doctor and the advocate, who were accused in the matter, further argued that the complaint was filed after the complainant failed to obtain compensation. They claimed that consequently, the complainant tried to falsely implicate them due to a personal grudge and failed extortion attempts.
On the other hand, the Additional Government Advocate submitted that the applicants were named in the FIR, and two rounds of investigations had been conducted. The initial investigation was done by the original Investigating Officer and then a second officer was appointed after the applicants applied for further investigation. The AGA submitted that the charge sheet and summoning orders were based on available evidence.
While considering the matter, the HC bench observed that Dr. Srivastava had been exonerated in the departmental inquiry, which had concluded that any medical negligence pertained to a private hospital, not the government facility.
“In so far as the present case is concerned, it is
prima-facie apparent that there being without any
cogent reason or evidence, the opposite party no.2
moved an application to the Chief Medical Officer with
the allegation that because of the operation conducted
by the applicant no. 2 (the doctor), she had suffered with
malignancy, though there is no medical report submitted in support of her complaint and when an
enquiry was conducted, it was found that the complaint
is false against the applicant no. 2 and thereafter, the
first information report has been lodged, while hatching
the applicants in a criminal conspiracy for personal
grudge.”
Further, the Court noted that when the complainant lodged the FIR on the incident dated 08.02.2007 while alleging the incident of 15.01.2007 even though “there is no explanation of the delay”.
Referring to the allegation that the applicants had hit the complainant with a motorcycle, leading to her fracture, the HC bench observed, “…having at glance the whole scenario, this is not understandable that for what reason and motive, the applicants would be intended to commit such offence.”
“It is also evident that the place where the incident is said to have occurred, is a public place, but there is no public eye witness of the incident, whereas, one of the witness namely, ****, who supported the version of the prosecution, is also not an ocular witness of the incident and he on the basis of receiving the information from the husband of the opposite party no. 2, has deposed before the police,” the bench further noted.
Regarding the claim by the applicants that Dr. Srivastava was on an emergency duty, from 14.01.2007 to 15.01.2007 and thereafter he was on Pulse Polio Duty, the Court noted that this fact had been certified by the Superintendent of P.H.C. Malihabad and “…this fact has not been denied anywhere in the Counter Affidavit filed on behalf of the State-respondent.”
At this outset, the Court also observed that the presence of Advocate Srivastava in the High Court on 15.01.2007 was supported by four other witnesses, “but, this fact seems to be ignored by the Investigating Officer as well as the learned trial court while issuing the summons. Further this fact has also not been denied by the State in it’s Counter Affidavit.”
The High Court bench referred to the Supreme Court’s order in the case State of Haryana vs. Bhajan Lal, and concluded that this case squarely fell under category (7) of mala fide prosecution.
“…the facts and circumstances of the present matter is indicative that the first information report has been lodged with a malafide and malicious intention, which is squarely covered with the ratio of the Judgment of the Hon’ble Apex Court in the case of Bhajan Lal(Supra),” observed the Court.
“It is trite law that it would not only be sufficient for the court to look into the averments made in the first information report/complaint alone to find out whether the necessary ingredients to constitute the alleged offence are disclosed, but, the court owes a duty to look into the other attending circumstances emerging from the record of the case over and above the averments and if it is required, the court with due care and caution, would try to read in between the lines. So far as the present case is concerned, the background of the circumstances indicates that the allegations levelled in the first information report, seem to be with a motive to wreaking vengeance and malafide,” it noted.
Accordingly, the Court quashed the criminal proceedings against the doctor and the advocate while noting that “the trial would result in a gross abuse of process of the law and would not serve the ends of justice.”
To view the order, click on the link below:
https://medicaldialogues.in/pdf_upload/allahabad-hc-quashes-criminal-proceedings-282636.pdf
Also Read: SC quashes Culpable Homicide Charges against Doctor for prescribing injection over phone