Angioplasty with sirolimus-coated balloon Comparable to Thin-Struts DES among in-stent restenosis Patients at 2 Years: Study
Italy: Findings from contemporary registry data have revealed encouraging data for interventionists hoping that a new generation of coronary balloons may improve the treatment of in-stent restenosis (ISR).
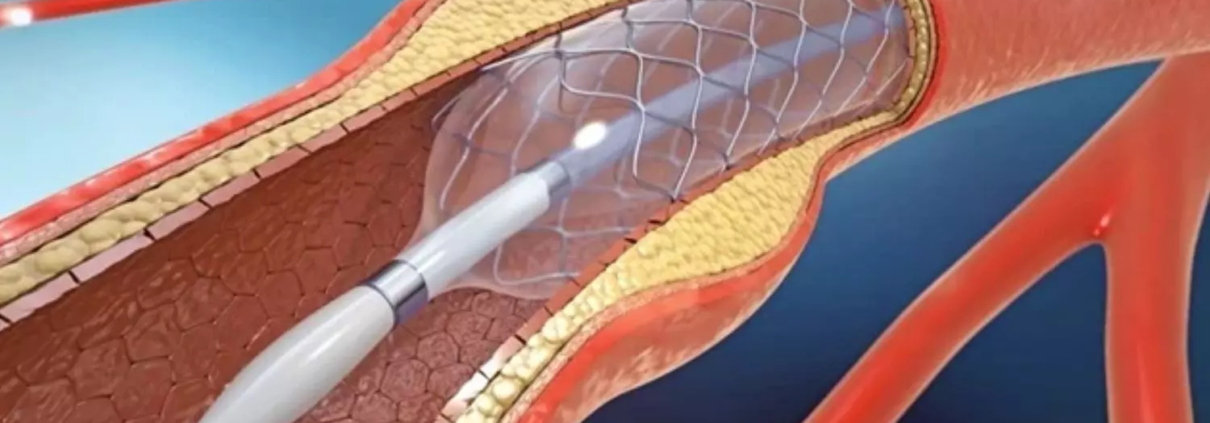
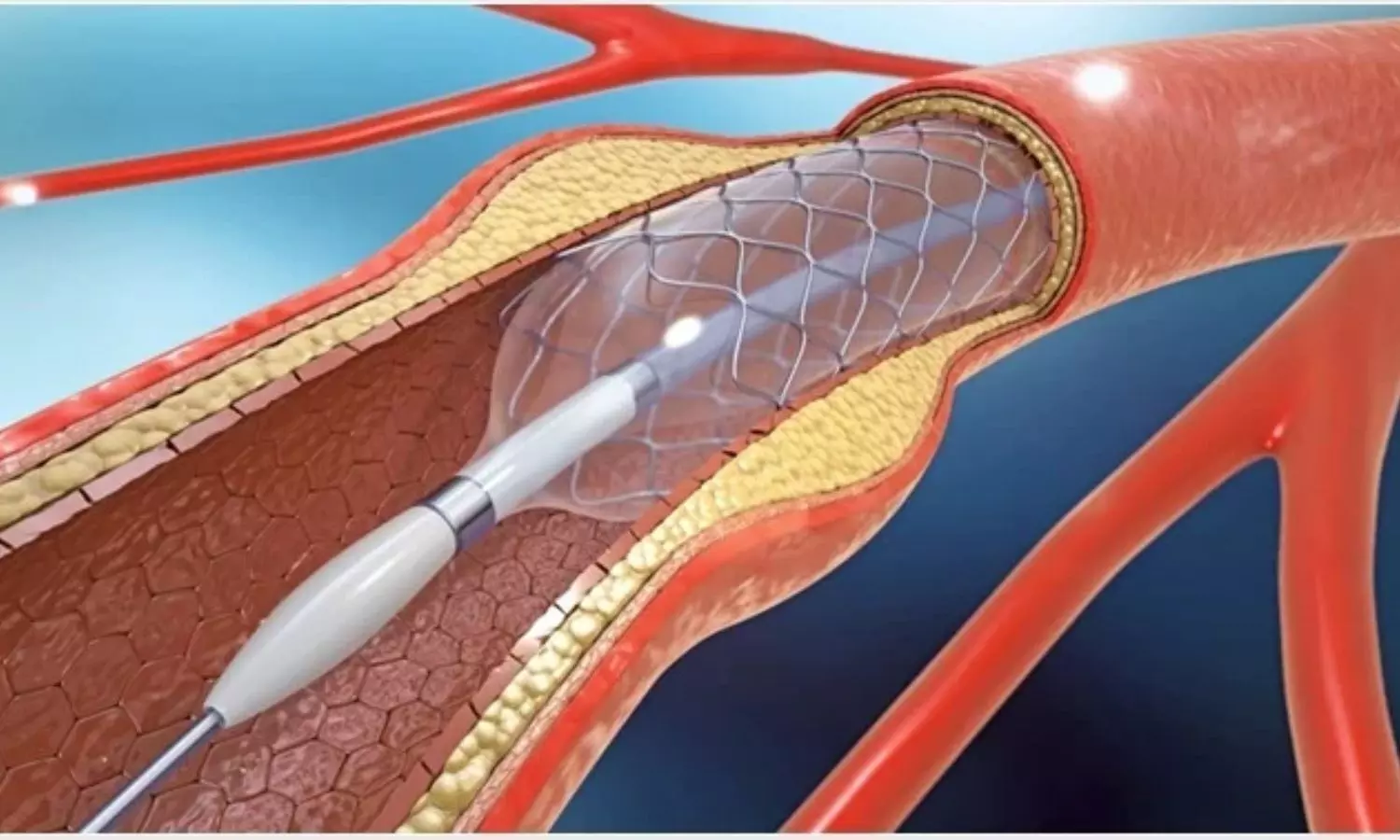
In a propensity score-matched analysis of 335 pairs of patients with ISR lesions, the researchers found that angioplasty with a new-generation sirolimus-coated balloon (SCB) yielded comparable rates of target vessel revascularization, target lesion revascularization, all-cause death, myocardial infarction, and major adverse cardiovascular events at two years as compared to thin-struts drug-eluting stents (DESs).
The findings provide some information about the long-term safety and efficacy of sirolimus DCBs versus DES in real-world patients with DES-ISR, the researchers wrote in Circulation: Cardiovascular Interventions.
DCBs that release sirolimus are a relatively new invention that requires researchers to engineer an effective release of this antiproliferative drug, owing to its limited lipophilicity inherently blocking effective vessel wall penetration.
Evidence indicates that drug-coated balloons may be beneficial in treating in-stent restenosis (ISR). However, in this setting, the efficacy of new-generation SCB compared with the latest-generation drug-eluting stents has not been studied. Considering this, Bernardo Cortese from Milan, Italy, and colleagues aimed to evaluate the safety and efficacy of SCB versus thin-struts DES in ISR at long-term follow-up.
The study included all patients in the EASTBORNE (The All-Comers Sirolimus-Coated Balloon European Registry) and DEB-DRAGON (DEB vs Thin-DES in DES-ISR: Long Term Outcomes) registries undergoing percutaneous coronary intervention for DES-ISR.
The primary study endpoint was target lesion revascularization at 24 months. Secondary endpoints included all-cause death, major adverse cardiovascular events, myocardial infarction, and target vessel revascularization at 24 months.
The study led to the following findings:
- The pooled analysis included 1545 patients with 1679 ISR lesions, of whom 40.2% of patients with 621 lesions were treated with thin-strut DES, and 59.8% of patients with 1045 lesions were treated with SCB.
- The unmatched cohort showed no differences in the incidence of target lesion revascularization (10.8% versus 11.8%); however, there was a trend toward lower rates of myocardial infarction (7.4% versus 5.0%) and major adverse cardiovascular events (20.8% versus 17.1%) in the SCB group.
- After propensity score matching (n=335 patients per group), there were no significant differences in the rates of target lesion revascularization (11.6% versus 11.8%), target vessel revascularization (14.0% versus 13.1%), myocardial infarction (7.2% versus 4.5%), all-cause death (5.7% versus 4.2%), and major adverse cardiovascular event (21.5% versus 17.6%) between DES and SCB treatment.
The researchers, however, acknowledged the inherent limitations of a non-randomized analysis. Additionally, the two registries came from different centers that did not follow a uniform protocol for lesion preparation.
Reference:
Wańha W, et al “Long-term outcomes following sirolimus-coated balloon or drug-eluting stents for treatment of in-stent restenosis” Circ Cardiovasc Interv 2024; DOI: 10.1161/CIRCINTERVENTIONS.124.014064.