Radial arterial access superior to femoral access in PCI: Study
USA: In a groundbreaking investigation into the comparative outcomes of radial versus femoral arterial access for percutaneous coronary intervention (PCI) in the United States, the study, published in the Journal of the Society for Cardiovascular Angiography & Interventions, has unveiled compelling insights into temporal trends and clinical implications. This pioneering research sheds new light on the evolving landscape of interventional cardiology and offers valuable guidance for healthcare practitioners and policymakers alike.
The study found a 2.8-fold increase in the use of radial access for PCI in the US over the past decade and represents the dominant form of access across all procedural indications. Based on instrumental variable analysis, a technique used to support causal inference, radial access was tied to lower in-hospital mortality, major access bleeding, and other major vascular complication rates than femoral access but with a slightly higher ischemic stroke risk.
New data presented at the Society for Cardiovascular Angiography & Interventions (SCAI) 2024 Scientific Sessions demonstrated the superiority of radial arterial access over femoral arterial access for coronary interventions.
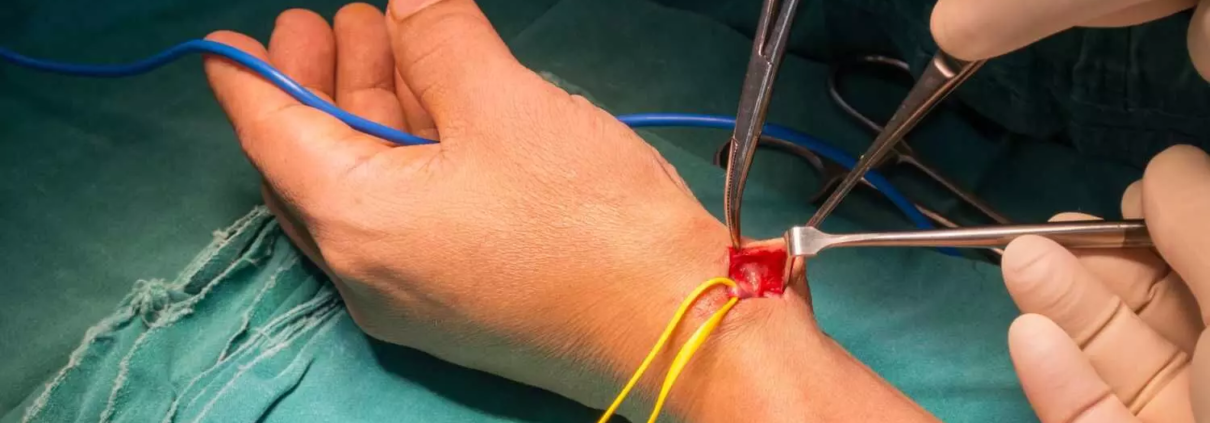
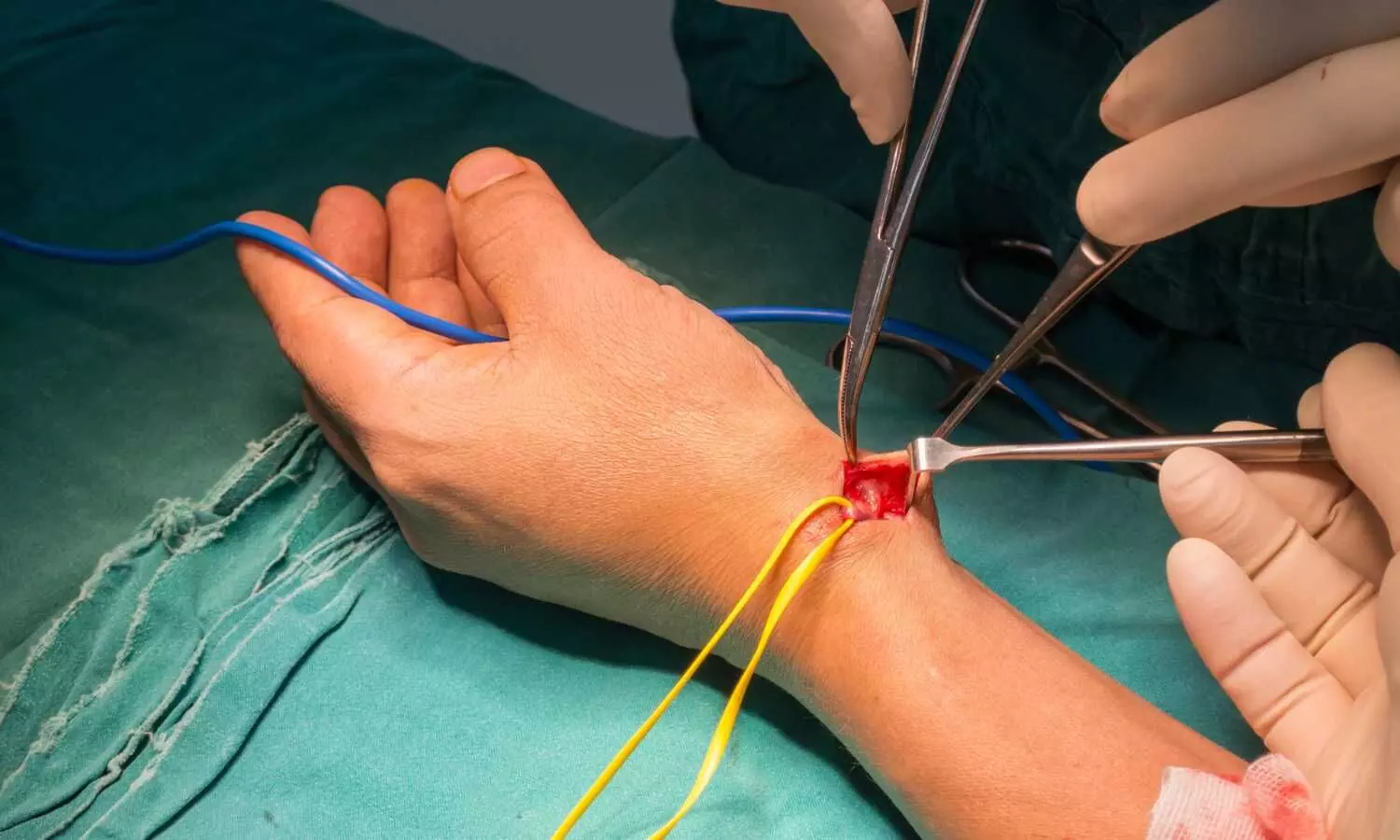
Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a minimally invasive procedure used to open blocked or narrowed coronary arteries, typically performed to treat coronary artery disease (CAD) and relieve symptoms of angina or prevent heart attacks. The choice of arterial access—radial (via the wrist) or femoral (via the groin)—has long been debatable among interventional cardiologists, with each approach carrying its own set of benefits and limitations.
Clinical practice guidelines recommend radial access for PCI because of superior outcomes compared with femoral access. Historically, the adoption of radial access in the United States has lagged behind much of the rest of the world, however, there is a lack of contemporary data on access site selection across the spectrum of clinical presentations and its association with outcomes.
To fill this knowledge gap, Reza Fazel, Beth Israel Deaconess Medical Center, Brookline, MA, and colleagues aimed to examine temporal trends in the utilization of radial versus femoral arterial access for PCI and to evaluate associated clinical outcomes.
For this purpose, the research team conducted a retrospective cohort study from the National Cardiovascular Data Registry’s CathPCI Registry, including PCIs performed between 2013 and 2022. They evaluated the comparative safety of radial versus femoral access for PCI using instrumental variable analysis exploiting operator variation in access preferences.
The following were the key findings of the study:
- During the study period, 2,244,115 PCI procedures were performed, of which 61.6% were performed via radial access, increasing from 23.9% in 2013 to 68.2% in 2022. This increase was seen in all geographic regions and across the full spectrum of presentations, with the largest relative increase seen in patients with ST-segment elevation myocardial infarction.
- In instrumental variable analyses, radial access was associated with lower in-hospital mortality (absolute risk difference [ARD] -0.15%), major access site bleeding (ARD -0.64%), and other major vascular complications (ARD -0.21%) but a higher risk of ischemic stroke (ARD 0.05%).
- There was no association with the falsification endpoint of gastrointestinal or genitourinary bleeding (ARD 0.00%).
As the field of interventional cardiology continues to evolve, studies like this play a pivotal role in informing best practices and shaping the future of cardiovascular care. By leveraging real-world data and rigorous analysis, researchers aim to drive innovation and improve outcomes for patients undergoing percutaneous coronary intervention.
“The study demonstrates a sea change in which PCI is performed in the US in response to trial data but also highlights the continued opportunity for practice improvement with dramatic interoperator variation,” said Dr. Fazel.
“It confirms that the benefit observed for radial access in RCTs has also been seen in real-world practice, including the largest benefits for the highest-risk patients. Finally, it shows a highly credible novel finding on the increased stroke risk.
Reference:
DOI: https://doi.org/10.1016/j.jscai.2024.101866