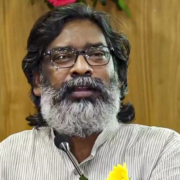
Jharkhand CM Proposes Health Circuit connecting Medical Colleges, Hospitals, District Health Facilities
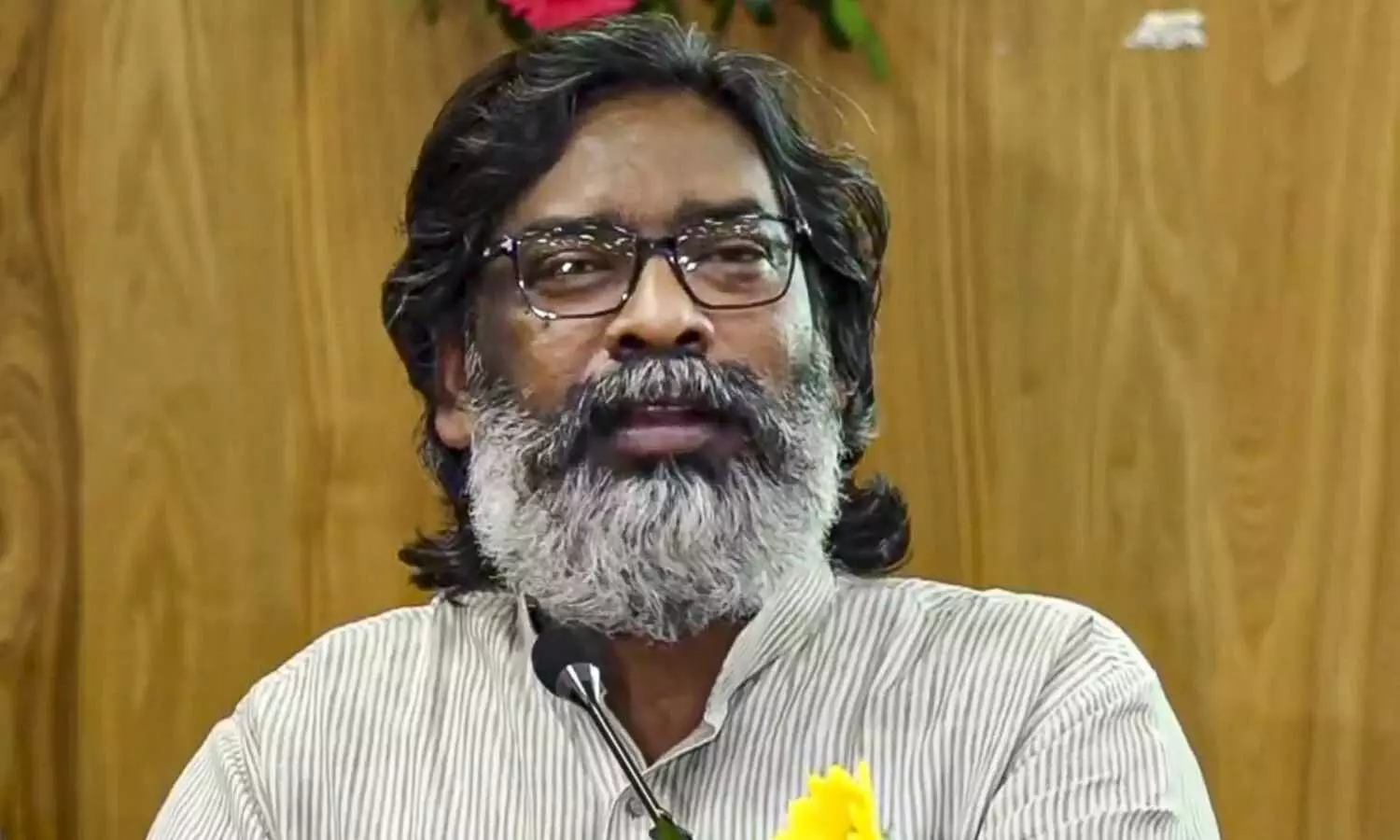
Ranchi: Jharkhand Chief Minister Hemant Soren on Thursday emphasized the need to create an integrated health circuit connecting all medical colleges, hospitals, and district health facilities across the state to enhance healthcare services.
According to the PTI report, the proposed circuit would help shift patients from one hospital to another as per the need and it would reduce the pressure of patients in one health facility, he said.
The chief minister, in a review meeting with health department officials, said that providing the best facilities to the people of the state was his government’s commitment.
Soren directed the officials that all government hospitals in the state should be functional 24×7 and take the initiative to ensure that better and modern facilities are provided at community health centres and district hospitals.
Also Read:Jharkhand CM lays foundation stone for 310-bed Apollo multi-speciality hospital in Ranchi
“Complaints of mismanagement in hospitals are often received through various mediums. Patients coming to hospitals for treatment face many problems. Some of them are not able to get beds in hospitals, while others face inconvenience in getting tests done. There is a crowd of patients in the OPD,” the CM said.
He also asked hospital authorities to strengthen capacity and infrastructure so that patients can easily access all information related to treatment, news agency PTI reported.
Expressing concern over the rising number of cancer patients, Soren asked officials to prepare a complete database of such people in the state so that his government can move forward to provide better treatment.
Medical Dialogues had earlier reported that Jharkhand Chief Minister Hemant Soren laid the foundation for a 310-bed multi-speciality hospital in the Smart City area of Ranchi. The facility, set to be developed by Apollo Hospitals Enterprises Limited, will occupy 2.75 acres of land provided free of charge by the Ranchi Municipal Corporation (RMC).
Also Read:Govt to bring Medical protection bill soon, says Jharkhand Health Minister Banna Gupta
Powered by WPeMatico