Lung ultrasound score easy and effective bedside tool for assessing lung parameters in mechanically ventilated patients: Study
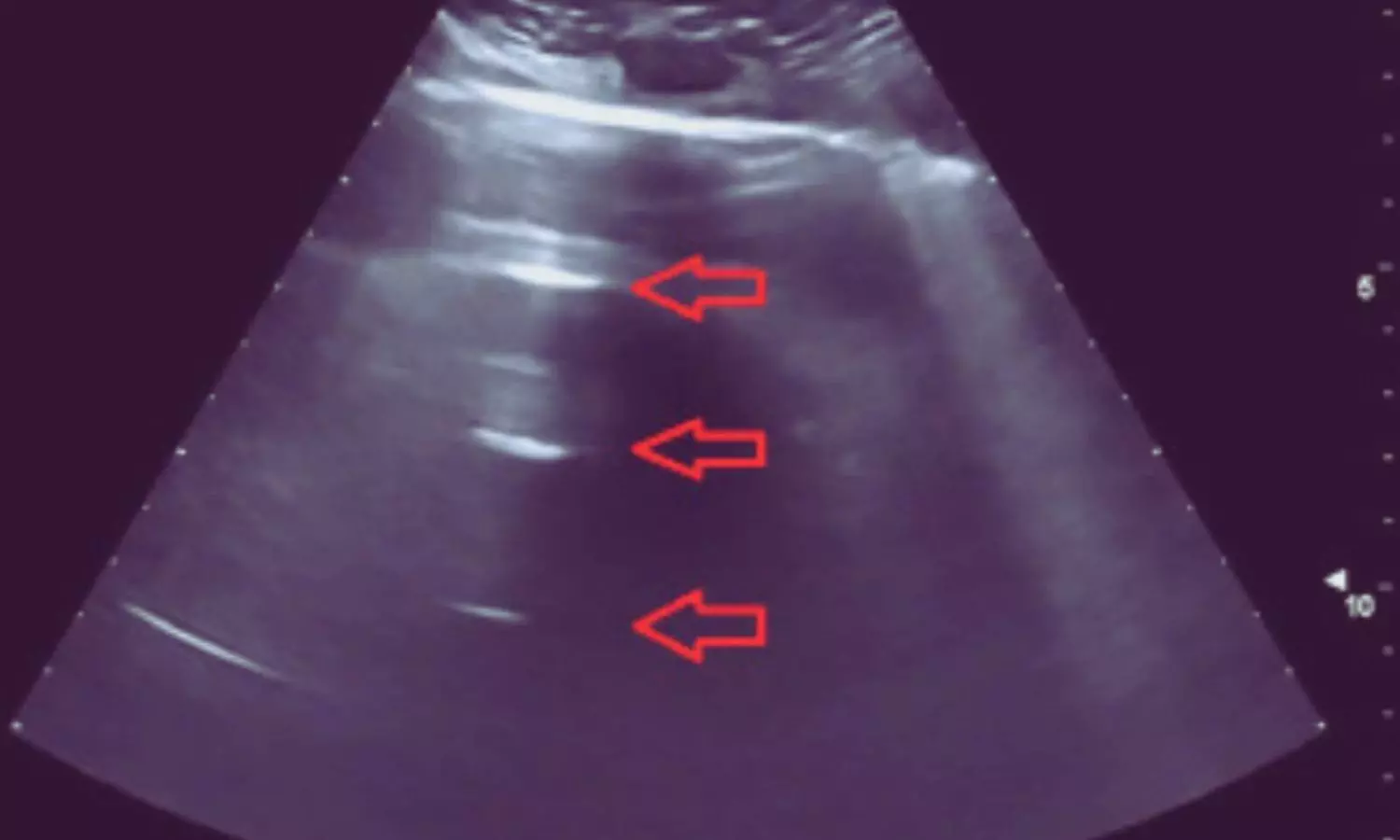
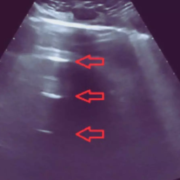
Lung ultrasound is a developing and beneficial method for identifying compromised alveolar air and the presence of interstitial and alveolar fluid. It assesses lung aeration beyond the pleura and can reveal underlying lung issues. Recent study aimed to investigate the relationship between lung ultrasound score (LUSS) and oxygenation, as well as respiratory mechanics, in mechanically ventilated patients. The researchers performed 101 lung ultrasounds in 50 patients aged 18-60 years requiring at least 24 hours of mechanical ventilation. The key findings of the study are: 1. LUSS showed a strong negative correlation with the ratio of arterial oxygen partial pressure (PaO2) to fractional inspired oxygen (FiO2) (ρ = -0.827, p<0.001), indicating that higher LUSS values are associated with worse oxygenation. 2. LUSS also had a moderate negative correlation with lung compliance (ρ = -0.634, p<0.001), suggesting that higher LUSS is associated with decreased lung compliance. 3. Conversely, LUSS had a strong positive correlation with lung resistance (ρ = 0.735, p<0.001), meaning higher LUSS values correspond to increased lung resistance. 4. Using receiver operating characteristic (ROC) curve analysis, the researchers determined that a LUSS greater than 12 can predict a PaO2/FiO2 ratio less than 200 with 97.37% sensitivity and 85.7% specificity.
Conclusion
The authors concluded that LUSS is an easy and effective bedside tool for assessing lung parameters in mechanically ventilated patients. It correlates significantly with oxygenation, lung compliance, and lung resistance, providing valuable information about the underlying lung pathology. LUSS may be useful for monitoring disease progression and guiding treatment in these critically ill patients.
Key Points
1. Lung ultrasound score (LUSS) showed a strong negative correlation with the ratio of arterial oxygen partial pressure (PaO2) to fractional inspired oxygen (FiO2), indicating that higher LUSS values are associated with worse oxygenation.
2. LUSS had a moderate negative correlation with lung compliance, suggesting that higher LUSS is associated with decreased lung compliance.
3. LUSS had a strong positive correlation with lung resistance, meaning higher LUSS values correspond to increased lung resistance.
4. Using receiver operating characteristic (ROC) curve analysis, the researchers determined that a LUSS greater than 12 can predict a PaO2/FiO2 ratio less than 200 with 97.37% sensitivity and 85.7% specificity.
5. The authors concluded that LUSS is an easy and effective bedside tool for assessing lung parameters in mechanically ventilated patients.
6. LUSS correlates significantly with oxygenation, lung compliance, and lung resistance, providing valuable information about the underlying lung pathology, and may be useful for monitoring disease progression and guiding treatment in these critically ill patients.
Reference –
Nishant Kumar et al. (2024). Relationship Of Lung Ultrasound Score With Oxygenation And Pulmonary Mechanics In Mechanically Ventilated Patients: An Observational Study. *Indian Journal Of Anaesthesia*. https://doi.org/10.4103/ija.ija_771_24.
Powered by WPeMatico