PCOS Management in India in 2024: Top 10 Insights from Gynecologists, Dermatologists and Endocrinologists Cross-Talk

Polycystic Ovary Syndrome (PCOS) remains one of the most challenging health concerns for women in India today, impacting both physical and emotional well-being. In a recent multi-specialty crosstalk on PCOS care, leading experts in endocrinology, gynecology, and dermatology shared insights that underscored the complexity of this condition and offered guidance on managing it effectively. The panel included Dr. Madhavi Latha, a Gynecologist practicing at Kalyan Hospital, Payakaraopet, Andhra Pradesh; Dr. Smita Ghate, Professor and Head of Department in Department of Dermatology, H.B.T. M. C. And R. N. C. G.H. Mumbai; and Dr. Tejal Lathia, an Endocrinologist at Cloud 9 Hospital, Mumbai.
Each specialist provided unique insights into PCOS management through their area of expertise. Here, we delve into the top 10 takeaways from this enlightening discussion.
1. Making a PCOS Diagnosis Prudently in Young Patients (Gynecology)
Diagnosing PCOS, particularly in adolescents, presents challenges due to its wide range of symptoms, from menstrual irregularities to metabolic issues like insulin resistance. To avoid premature labeling in young patients, it is recommended to adopt a “probable PCOS” status and revisit the diagnosis after a few years. This approach helps manage symptoms while reducing anxiety and social stigma.
2. Cost-effective and Focused Testing for PCOS Diagnosis – Practical Pearls (Endocrinology)
Efficient and economical testing is key in managing PCOS. Diagnostic criteria include irregular menstrual cycles lasting more than 35 days, signs of hyperandrogenism, and ultrasound findings of ovarian volume over 10 cc or more than 20 follicles. Adolescents should not be diagnosed based on ultrasound findings alone. Avoiding unnecessary follow-up ultrasounds or tests reduces costs and keeps care accessible, especially for young patients, and is relevant in Indian socio-economic settings
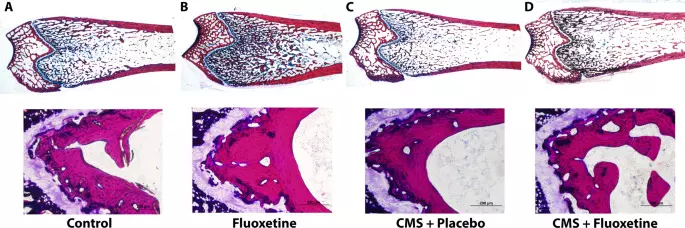
3. Addressing Mental Health as an Essential Component of PCOS Care (Dermatology)
PCOS brings significant psychological burdens, with high rates of anxiety, depression, and body image concerns among patients. Visible symptoms like acne and hirsutism can exacerbate these issues. Positive and supportive communication is essential in reducing stigma, while incorporating mental health support, such as professional therapy, can foster better coping strategies, enhancing overall care quality in these patients.
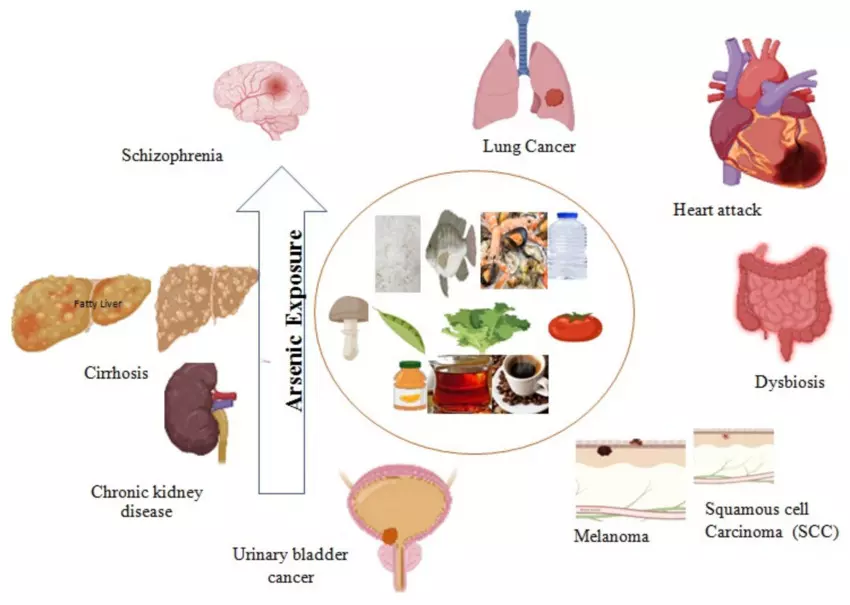
4. Awareness of Dietary Adjustments & Environmental Factors (Dermatology)
Lifestyle and environmental factors play significant roles in PCOS management. A dietary approach emphasizing whole foods, fiber, and probiotics helps maintain gut health and support hormonal balance. Additionally, reducing exposure to endocrine disruptors found in plastics and processed foods contributes to long-term health and may help alleviate PCOS symptoms.
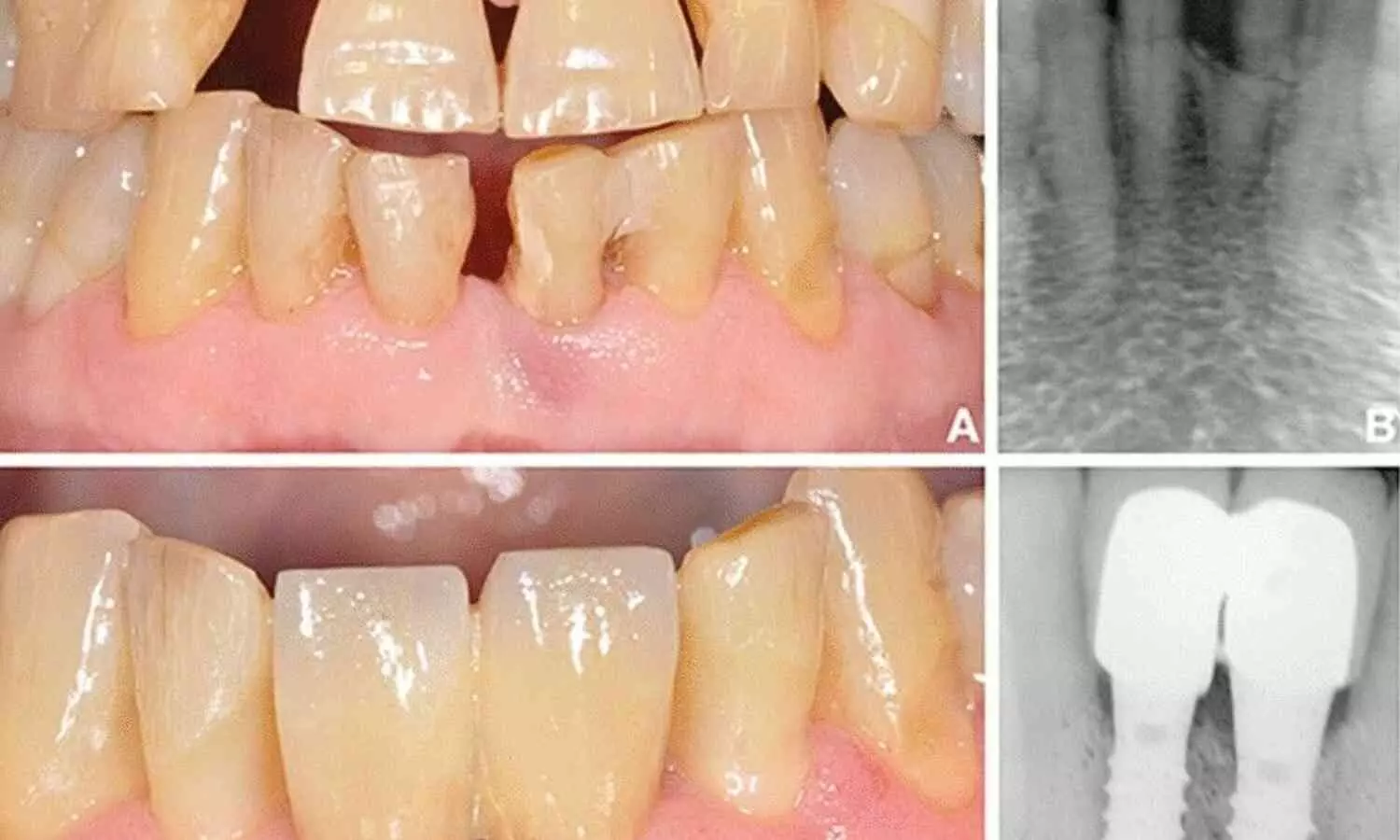
5. Dermatological Symptoms: Recognizing Hyperandrogenic Indicators (Dermatology)
PCOS frequently manifests through dermatological issues, such as resistant acne, hirsutism, and pigmentation around the knuckles and neck (acanthosis nigricans). Recognizing these symptoms early can guide diagnosis and treatment with a combination of metformin, lifestyle modifications, and skin-specific therapies like topical treatments like salicylic acid peels. Managing these symptoms can boost patient confidence and overall quality of life.
6. Dealing with PCOS & Pregnancy (Gynecology)
PCOS can complicate pregnancy, increasing risks of gestational diabetes, hypertension, and miscarriage. Pre-pregnancy counseling and annual screenings for blood glucose and blood pressure are recommended to identify risks early. In pregnancy, careful monitoring through continuous glucose monitoring and metformin under professional guidance & physician discretion can help mitigate risks, improving outcomes for both mother and child.
7. Insulin Resistance: Addressing the Core Metabolic Challenge (Endocrinology)
Insulin resistance is a central issue in PCOS, making the management of insulin sensitivity essential for alleviating symptoms. Metformin, commonly used to reduce androgen levels, helps regulate menstrual cycles and can lessen acne. A balanced diet, reduced in processed carbohydrates and higher in protein, alongside regular exercise, supports effective insulin resistance management in PCOS.
8. Lifestyle Modifications as the Foundation of PCOS Management (Gynecology)
Lifestyle interventions remain a foundational approach to PCOS management. For women with PCOS, maintaining a healthy weight through balanced nutrition and regular physical activity can significantly improve metabolic parameters and fertility outcomes. Weight reduction of even 5-10% positively impacts menstrual regularity and general health, while lean PCOS patients benefit from waist circumference monitoring and stress reduction techniques.
9. Metformin as a Treatment Option in Adolescents and Adults (Endocrinology)
Metformin is often recommended, especially for adolescent patients dealing with insulin resistance and weight management challenges. Beyond metabolic benefits, metformin can aid in regulating menstrual cycles without introducing hormonal pills, which are often avoided in younger patients due to potential impacts on bone health. Initiation of metformin at doses of 500 mg, gradually increased, supports both weight loss and balance androgenic hormones effectively.
10. Compassionate Communication and Simplified Patient Education (Gynecology)
Effective communication is essential in PCOS management. Using positive, empathetic language and avoiding words that may shame or blame patients can significantly improve their mental well-being. Educating patients in a supportive manner empowers them and instills confidence to manage their condition effectively, fostering trust and adherence to treatment plans.
Powered by WPeMatico