Native American patients are sent to collections for debts the government owes
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Faridabad: The Atal Bihari Vajpayee Medical College and Hospital in Chhainsa village, is set to launch its Indoor Patient Department (IPD) services next month. The 400-bed hospital had faced delays in launching its IPD services due to a series of infrastructural and regulatory hurdles, including the absence of a No Objection Certificate (NOC) from the fire department and other required clearances.
The state government took over the medical college and hospital in 2021-22 after the closure of a private institution due to financial difficulties in 2015. The Emergency services of the hospital were launched in April 2023, the IPD remained on hold for months due to pending approvals and regulatory compliance. Despite these setbacks, the hospital started Outpatient Department (OPD) services in July 2022 but the admittance of patients into the hospital was delayed as certain conditions were yet to be met.
After conducting a visit, officials from the concerned departments identified several shortcomings and instructed the authorities to address the discrepancies. Reportedly, the department was also required to carry out certain tasks, including constructing staircases.
Speaking to Tribune India, an official stated, “With the infrastructure for starting the IPD services ready, day-care facilities are already being provided.” The official also added that up to 200 patients had been reporting at the OPD, and the number was expected to rise further due to the various facilities, including pathological tests at nominal charges.
The authorities have also reached out to the district administration and departments such as transport, requesting an increase in the frequency and number of buses on the route to assist patients and their attendants. This will make it easier for patients and their attendants to travel to the hospital from various parts of the district.
The hospital authorities have emphasized the need to establish a Critical Care Unit, modeled after the Trauma Centre, to treat patients in critical condition following accidents. The management has already raised this issue with the state government, stressing the importance of a dedicated trauma care unit to strengthen the region’s emergency healthcare services. Additionally, the hospital is grappling with a shortage of specialist doctors, which further hampers its ability to deliver comprehensive care.
Located approximately 20 km from the district headquarters, this is the second government institution in the area, following the ESIC Medical College and Hospital. The government has invested significant resources in restoring and upgrading the hospital’s infrastructure. Over the past four years, Rs 47.25 crore has been spent on the construction and repair work to make the hospital functional. This investment has played a crucial role in transforming what was once an abandoned private facility into a state-of-the-art government-run institution. The hospital was established after the state government took over the defunct private hospital in 2015.
Also Read: PM Modi inaugurates 960-bed AIIMS Kalyani, IPD services open for patients
The hospital also serves as a critical educational institution, with the first batch of 100 MBBS students admitted in 2022. This year, the third batch of medical students joined the college this year.
Dr BM Vashisht, the Director of the hospital, stated that the IPD services were expected to begin next month, as all necessary norms had been met.
Powered by WPeMatico

Researchers have discovered that long-term glycemic control does not affect the risk of bacterial infection in type 2 diabetes patients. A recent study was published in the journal PloS One by Edouard and colleagues. Diabetes mellitus affects a considerable part of the population worldwide, and its prevalence in France is estimated to be at 5.3% in 2020. Type 2 diabetes mellitus is the most common type and is linked to an increased risk of infection.
This study aimed to determine if glycemic control, determined by the levels of glycated hemoglobin, and severity of diabetes, as indicated by the number and type of antidiabetic drugs, are related to infectious risk. This was a cohort study based on data obtained from January 2012 to January 2022 from a French primary care database. Infectious risk was estimated using the mean number of antibiotic prescriptions per year, as an indicator of bacterial infections.
A retrospective cohort study looked at information from 59,020 patients, leading to analysis from 1,959 in the final instance. The glycemic control was classified on thresholds based on glycated hemoglobin and the severity of diabetes evaluated by the number and kind of antidiabetic treatments applied. The annual mean antibiotic prescriptions were taken as measurements of infectious risk. A sum of ANOVA tests was used in the statistics.
Main Results
• No relation between glycemic control and infection risk
• The mean count of antibiotic prescriptions per year was not significantly associated with glycated hemoglobin threshold level (p = 0.228).
Diabetes Severity and Infection Risk:
• Secondary analyses did not determine any association between the numbers of antidiabetic treatment and infection risk (p = 0.53). The type of antidiabetic treatment was also not significantly associated with antibiotic prescriptions (p = 0.018).
These findings can potentially change clinical strategies towards infection prevention among patients with type 2 diabetes, especially shifting the interest from glycaemic control to others such as immunity and comorbid conditions. In conclusion, long-term glycemic control and severity of diabetes were not correlated with the risk of bacterial infection in patients with type 2 diabetes. This research, for the first time, demonstrates how databases from primary care can contribute to advancing research and enhance our understanding of the complexities around managing diabetes and infectious risks.
Reference:
Lemoine, E., Dusenne, M., & Schuers, M. (2024). Glycemic control and bacterial infectious risk in type 2 diabetes: A retrospective cohort from a primary care database. PloS One, 19(12), e0314287. https://doi.org/10.1371/journal.pone.0314287
Powered by WPeMatico

A new study published in the JACC: Clinical Electrophysiology journal showed that when acute procedural success is attained in a subset of patients with ventricular tachycardia (VT) and a left ventricular ejection fraction (LVEF) higher than 35% following myocardial infarction, catheter ablation alone could be enough.
Post–myocardial infarction (MI) individuals with ventricular tachycardia are regarded at risk for VT recurrence and sudden cardiac death (SCD). For more than 20 years, implanted cardioverter-defibrillators (ICDs) have been advised for the prevention of SCD in patients with hemodynamically tolerated sustained monomorphic ventricular tachycardia (SMVT), irrespective of the left ventricular ejection fraction.
According to recent guidelines, catheter ablation should be explored as an alternative to an implanted cardioverter-defibrillator (ICD) in some individuals. This study was to examine the results of patients who were referred for VT ablation based on acute ablation outcome, left ventricular ejection fraction, and VT tolerance.
Post-MI patients without a history of ICD who had VT ablation at a single facility between 2009 and 2022 were included in this research. Catheter ablation was recommended as first-line treatment for patients with tolerable VT and an LVEF greater than 35%. All patients were given the option of ICD implantation, however the choice was made jointly based on the patient’s clinical presentation, LVEF, and ablation results.
VT ablation was performed on 86 patients (mean age 69 ± 9 years, 84% male, mean LVEF 41 ± 9%). 51 of the 66 patients with LVEF >35% have tolerated VT and 37 (73%) of these 51 individuals were made non-inducible.
An ICD was implanted in 11 out of 14 inducible patients and 5 out of 37 non-inducible patients. 10 out of 86 patients experienced VT recurrence after a median follow-up of 40 months (Q1-Q3: 24-70 months). One patient with ICD passed away unexpectedly, and the total mortality rate was 27%.
No SCD or VT recurrence happened among the 37 patients (none on antiarrhythmic medications) with LVEF >35%, tolerated VT, and non-inducibility. There was no SCD among the 14 patients with LVEF >35%, tolerated VT, and inducibility following ablation, yet, 29% of them experienced VT recurrence.
Overall, the prognosis for modern post-MI patients who have stable coronary disease, LVEF >35%, tolerated VT, no signs of hemodynamic compromise, and are noninducible following functional substrate ablation is favorable. In these particular patients, it appears to be safe to forego ICD installation.
Source:
Rademaker, R., de Riva, M., Piers, S. R. D., Wijnmaalen, A. P., & Zeppenfeld, K. (2024). Excellent Outcomes After First-Line Ablation in Post-MI Patients With Tolerated VT and LVEF >35%. In JACC: Clinical Electrophysiology (Vol. 10, Issue 11, pp. 2303–2311). Elsevier BV. https://doi.org/10.1016/j.jacep.2024.06.027
Powered by WPeMatico
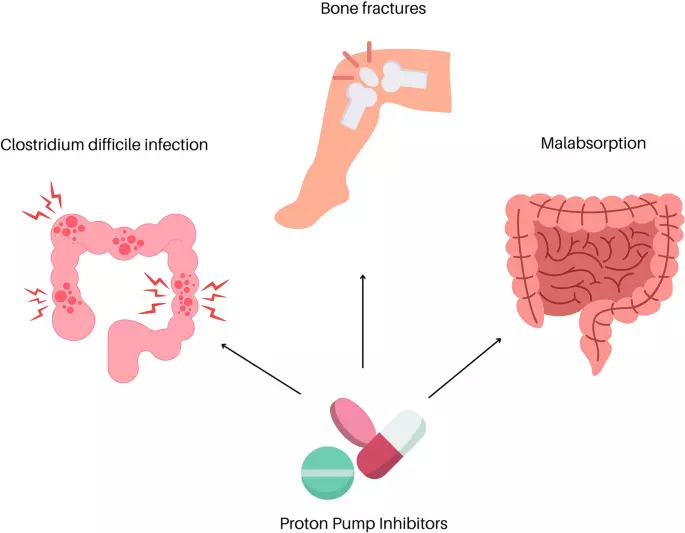
Proton pump inhibitors are tied to accelerated renal risk among CKD patients, suggests a study published in the BMC Nephrology.
Although Proton pump inhibitors (PPIs) were widely prescribed for gastrointestinal (GI) diseases, there were numerous studies about PPIs and adverse renal outcomes. Most evidence was to evaluate the risk of PPIs in patients with normal renal function and the absence of moderate to advanced chronic kidney disease (CKD). This study focuses on the accelerated progression of renal function following proton pump inhibitors (PPIs) use, and the increased risks of acute kidney injury (AKI) among moderate to advanced CKD (pre-ESRD) patients. A retrospective cohort study was conducted by including adult patients with chronic kidney disease (CKD) stages 3b to 5 who initiated PPI or H2 blocker (H2B) therapy between 2011 and 2018. The risk of renal events was assessed using the Cox proportional hazard model to estimate the adjusted hazard ratio (HR) and 95% confidence interval (CI). Sensitivity analyses were performed, including propensity score matching, as-treated analysis, and subgroup analysis. Results: The cohort comprised 83,432 pre-ESRD patients, with 5,138 treated with H2B and 1,051 with PPIs. The progression to ESRD was significantly more likely in patients using PPIs compared to those using H2B (adjusted HR, 1.495; 95% CI: 1.198–1.867). Specifically, omeprazole (adjusted HR, 1.784; 95% CI: 1.079–2.951) and esomeprazole (adjusted HR, 1.847; 95% CI: 1.332–2.561) were associated with a notably higher risk of ESRD and AKI. The study highlights the significance of the accelerated renal risk, especially for moderate to advanced CKD patients, when prescribing PPIs and implicates the clinicians prescribed PPIs and H2B in pre-ESRD patients.
Reference:
Huang, CH., Tsai, CJ., Su, CC. et al. Accelerated risk of renal disease progression in pre-ESRD patients with proton pump inhibitors use: a nationwide population-based study. BMC Nephrol 25, 469 (2024). https://doi.org/10.1186/s12882-024-03867-6
Keywords:
Proton pump, inhibitors, use, accelerated, renal risk, among, CKD, patients, suggests, study, BMC Nephrology, Huang, CH., Tsai, CJ., Su, CC, Proton pump inhibitors, H2 blocker, pre-ESRD, Nephrotoxicity, Asia
Powered by WPeMatico
A new study published in the Graefe’s Archive for Clinical and Experimental Ophthalmology showed that all visual function measures recovered quickly and without any side effects with oral high-dose methylprednisolone optic neuritis (ON).
Serum aquaporin-4 autoantibodies are linked to neuromyelitis optica spectrum disease (NMOSD) is an inflammatory condition affecting the central nervous system. The most prevalent manifestations of this spectrum are myelitis and optic neuritis. Usually, it presents as subacute vision loss accompanied by discomfort that is frequently made worse by eye movement.
Multiple sclerosis (MS) and ON are closely related, and their pathophysiologies are typically comparable. About 50% of ON patients will go on to acquire MS. Despite no long-term effects on visual results, corticosteroids have been used extensively to treat optic neuritis and MS relapse. Their impact on the short-term recovery of visual function has been well documented. As of now, the only proven therapy for ocular neuritis is high doses of venous corticosteroids. To evaluate the changes in visual function parameters following oral high-dose methylprednisolone in ON patients, Elodie Boureaux and her colleagues carried out this study.
The patients with acute ON were analyzed retrospectively. For 3 to 5 days, the patients were given 1 g of oral methylprednisolone daily. Before treatment, 4 days, 2 weeks, 1 month, 3 months, and 6 months after treatment, visual function was assessed using the ETDRS test for visual acuity, the 30-second automated visual field test, the contrast sensitivity test, and the color vision test. At several time points, optical coherence tomography of the ganglion cells was carried out to evaluate anatomical alterations.
The research comprised a total of 29 participants in total between September 2014 and September 2016. After 3 and 6 months, approximately 80% of patients had returned to normal visual acuity. Although this recovery of all visual function measures was shown as early as 4 days following the start of therapy, it generally happened within 15 days. During the follow-up, this study saw weakening of the ganglion cell layer, which typically happens within a month.
At 6 months, the P100 wave of visually evoked potentials was seen in every patient. 2 individuals suffered a recurrence of ON during the six-year follow-up period. Also, no significant negative impacts were noted. Overall, for individuals with ON, oral high-dose methylprednisolone may be a safe and effective therapy for visual recovery.
Source:
Boureaux, E., Laurent, C., Rodriguez, T., Le Page, E., & Mouriaux, F. (2024). Visual recovery after oral high-dose methylprednisolone in acute inflammatory optic neuropathy. In Graefe’s Archive for Clinical and Experimental Ophthalmology (Vol. 262, Issue 12, pp. 3979–3985). Springer Science and Business Media LLC. https://doi.org/10.1007/s00417-024-06568-w
Powered by WPeMatico

Researchers have established that consanguineous marriages greatly elevate the risk of congenital hearing loss among children in Saudi Arabia. A recent study was conducted by Shawq F. A. and colleagues which was published in the International Journal of Pediatric Otorhinolaryngology. The prevalence of hereditary hearing loss in Saudi Arabia is mainly due to first-cousin marriages, which are a widely practiced cultural norm.
A search was performed in September 2023 on the databases of PubMed, CENTRAL, MEDLINE, and EMBASE. Two reviewers conducted independent screening and data extraction. The review focused on Saudi Arabian studies regarding hereditary hearing loss. The review ensured ethical practice in dissemination because it utilized only research articles that were public and excluded any study that involved humans or animals. Due to heterogeneity in study designs and outcomes, a meta-analysis was not possible.Due to the heterogeneity of study designs and outcomes, a meta-analysis was deemed not feasible.
Results
Prevalence of Consanguinity: Rates of consanguineous marriages varied between 21.1% and 80.8%, where first-cousin marriages were the most prevalent.
Risk of Hearing Loss: Children born from consanguineous marriages had a highly significant risk of CHL than those born from non-consanguineous unions.
Increased Risk: The risk of CHL in children born to consanguineous parents was 3.5 times higher.
Genetic Factors: Genetic and hereditary influences were constantly reported across the studies with varying prevalence and contributing risk factors.
Consanguinity has serious consequences on the childhood hearing health of Saudi Arabia, and targeted interventions are therefore necessary. Some of the suggested measures include:
Educational Programs: To increase awareness about the genetic risks associated with consanguineous marriages.
Genetic Counseling: Providing couples with comprehensive genetic information and support to make informed decisions.
Premarital Screening: Expanding mandatory screening programs to include hereditary hearing loss markers and counseling.
This systematic review uncovers a significant correlation between consanguineous marriages and the increased predisposition of Saudi Arabian children to congenital hearing loss. This calls for sound public health policies, such as education, genetic counseling, and premarital screening programs, which would significantly alleviate the hereditary burden of hearing loss and lead to better outcomes in this regard.
Reference:
Powered by WPeMatico
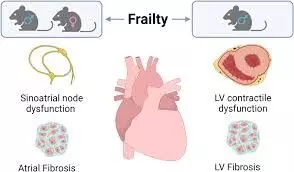
Frailty significantly elevates the risk of adverse outcomes among patients undergoing CABG, reveals a study published in the BMC Surgery.
Coronary artery bypass grafting (CABG) remains the preferred treatment for complex multi-vessel coronary artery disease, offering substantial long-term benefits. Non-cardiac comorbidities such as frailty may significantly affect the outcomes of this procedure. However, the exact impact of frailty on CABG outcomes remains unclear, particularly given its exclusion from many pivotal revascularization trials. This systematic review and meta-analysis aimed to consolidate existing data to evaluate the impact of frailty on short- and long-term outcomes following CABG. Searches across PubMed, Cochrane Library, Embase, and Scopus were done to identify studies that were published up to March 31, 2024, had detailed preoperative frailty assessments and compared frail versus non-frail adult patients undergoing CABG. Primary outcomes were all-cause mortality and major adverse cardiac events within one year. Secondary outcomes included hospital readmission rates and length of stay. A random-effects model was used to account for heterogeneity. Results were reported as odds ratios (OR) or mean differences (MD) with 95% confidence intervals (CI). Results: The meta-analysis, involving data from 14 studies, revealed a significant increase in both 30-day (OR 2.52; 95% CI: 2.07 to 3.07) and 1-year mortality (OR 2.58; 95% CI: 1.49 to 4.45) among frail patients. The risk of acute cardiac and cerebrovascular complications was comparable in all patients (OR 1.03; 95% CI: 0.89 to 1.19). However, frailty was associated with a significant increase in the risk of acute kidney injury (OR 2.31; 95% CI: 1.26 to 4.23). Frail patients were more likely to have longer hospital stays and higher readmission rates compared to their non-frail counterparts. The study confirms the critical impact of frailty on mortality and morbidity in CABG patients and advocates for the integration of frailty assessments into the preoperative evaluation process. Addressing frailty can lead to more individualized patient care and better outcomes, urging a paradigm shift towards comprehensive, patient-centric management in cardiac surgery.
Reference:
Chen, S., Zhang, S., Cai, S. et al. Impact of frailty on outcomes following coronary artery bypass grafting: a systematic review and meta-analysis. BMC Surg 24, 419 (2024). https://doi.org/10.1186/s12893-024-02728-1
Keywords:
Frailty, significantly, elevates, risk, adverse, outcomes, among, patients, undergoing, CABG, reveals, study, BMC Surgery, Chen, S., Zhang, S., Cai, S, Frailty, CABG, Mortality, Cardiac surgery, Elderly, Systematic review, Meta-analysis
Powered by WPeMatico

Bone fractures often require arthroplasty, which carries the risk of surgical site infections (SSIs) and prosthetic joint infections (PJIs). Antibiotic-loaded bone cement (ALBC) is commonly used to reduce these risks. Dual antibiotic-loaded cement (DALC) has been proposed as a more effective option compared to single antibiotic-loaded cement (SALC).
Ahmed E A et al conducted a systematic review and meta-analysis aimed to compare the efficacy and safety of DALC and SALC in preventing infections and related outcomes in arthroplasty.
The authors conducted a systematic review and meta-analysis comparing DALC and SALC in patients undergoing hip or knee arthroplasty for fractures. The primary outcome was infection rate (SSI and PJI), with secondary outcomes including re-revision rates and mortality. Databases searched included PubMed, Cochrane Library, Scopus, and Google Scholar. Data synthesis was performed using Review Manager Software (RevMan 5.4, Cochrane Methods, London, UK), and odds ratios (OR) with 95% confidence intervals (CI) were calculated.
Key findings of the study were:
• Nine studies comprising 55,672 patients were included. Eight studies focused on hip arthroplasty, and four included knee surgeries.
• In hip arthroplasty, DALC significantly reduced infection rates compared to SALC (OR, 0.64; 95% CI, 0.49 to 0.83; P = 0.001), with moderate heterogeneity (I² = 52%). However, no significant difference was found in knee arthroplasty (OR, 1.21; 95% CI, 0.87 to 1.70; P = 0.26).
• Overall, DALC showed a significant reduction in infection rates (OR, 0.81; 95% CI, 0.66 to 1.00; P = 0.05). DALC also significantly reduced deep surgical site infections in hip surgeries (OR, 0.46; 95% CI, 0.33 to 0.66; P < 0.001).
• No significant differences were observed in re-revision rates for either hip or knee arthroplasty. Mortality rates were also not significantly different between DALC and SALC.
The authors concluded that – “The study reveals that dual antibiotic-loaded cement (DALC) is more effective in reducing infection rates, especially in hip surgeries, than single antibiotic-loaded cement (SALC). DALC reduces deep surgical site infections and prosthetic joint infections in hip replacement patients. However, it did not significantly improve knee surgeries, suggesting the need for further research on this subgroup. Also, we found no significant difference in re-revision rates or mortality between DALC and SALC. Hence, the clinical advantage of DALC may be limited to reducing infections and no other long-term outcomes, such as reoperations or patient survival. We recommend future large-scale randomized controlled trials focusing on the efficacy, cost-benefit analyses, and long-term effects of dual antibiotic therapies.”
Further reading:
Ahmed E A, Muharib R. Alruwaili K, Abdulhamid F. Alanazi A, et al. (December 06, 2024) Efficacy and Safety of Dual vs Single Antibiotic-Loaded Cement in Bone Fracture Management: A Systematic Review and Meta-Analysis. Cureus 16(12): e75208. DOI 10.7759/cureus.75208
Powered by WPeMatico
