Autotransplantation of third molars with fully formed roots promising solution for replacing missing teeth, finds study
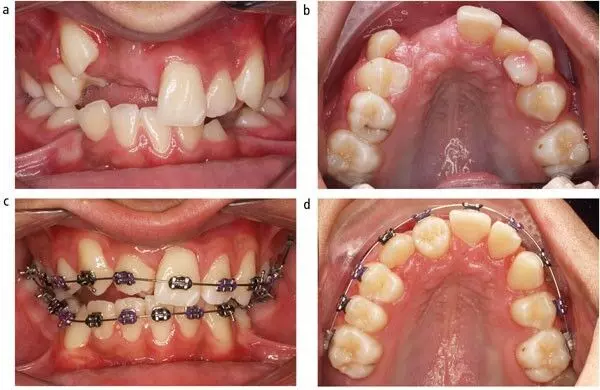
A study published in the Journal of the American Dental Association suggests that autotransplantation of third molars with fully formed roots is a promising solution for replacing missing teeth.
The autotransplant of third molars to replace missing teeth is gaining attention. This study aimed to analyze factors influencing the success, survival, and inflammatory root resorption (IRR) of autotransplanted third molars with completely formed roots. A total of 160 patients who underwent autotransplant of third molars with completely formed roots were evaluated retrospectively, involving 168 teeth. Preoperative, intraoperative, and postoperative variables were assessed to identify prognostic factors for success, survival, and IRR. Results: The average (SD) follow-up was 5.21 (1.99) years. The success, survival, and IRR rates were 75.0%, 91.1%, and 17.3%, respectively. Cox proportional hazards regression analysis revealed that both apical resection and retrofilling (ARR) (P < .001) and donor tooth replicas (P < .001 for success and IRR; P = .013 for survival) were associated significantly with success, survival, and IRR. Furthermore, root canal treatment timing and patient age significantly affected success and survival, respectively (P = .006 and P = .036). The use of donor tooth replicas significantly reduced both the surgical time (P < .001) and extraoral time of the donor tooth (P < .001), whereas ARR increased the extraoral time of the donor tooth (P = .002). The use of a single root donor tooth was associated with a reduced surgical time (P = .003). Using donor tooth replicas and avoiding ARR contributed to increased success and survival rates and prevented IRR. Third molars with completely formed roots are suitable donors for replacing missing teeth, provided that appropriate preoperative, intraoperative, and postoperative indications are considered.
Reference:
Xia J, Ge Z, Zhang Y, Shi J, Xie Z. Prognostic factors for autotransplanted third molars with completely formed roots: A retrospective cohort study. J Am Dent Assoc. 2024 Nov 23:S0002-8177(24)00588-9. doi: 10.1016/j.adaj.2024.10.004. Epub ahead of print. PMID: 39580736.
Keywords:
Autotransplantation, third, molars, fully, formed, roots, promising, solution, replacing, missing, teeth, finds, study, Journal of the American Dental Association, Autotransplantation; inflammatory root resorption; success rate; survival analysis; survival rate; third molar, Xia J, Ge Z, Zhang Y, Shi J, Xie Z
Powered by WPeMatico