Elective Single-Embryo and Transfer Mechanisms leading to embryonic splitting and its risk factors, explains study
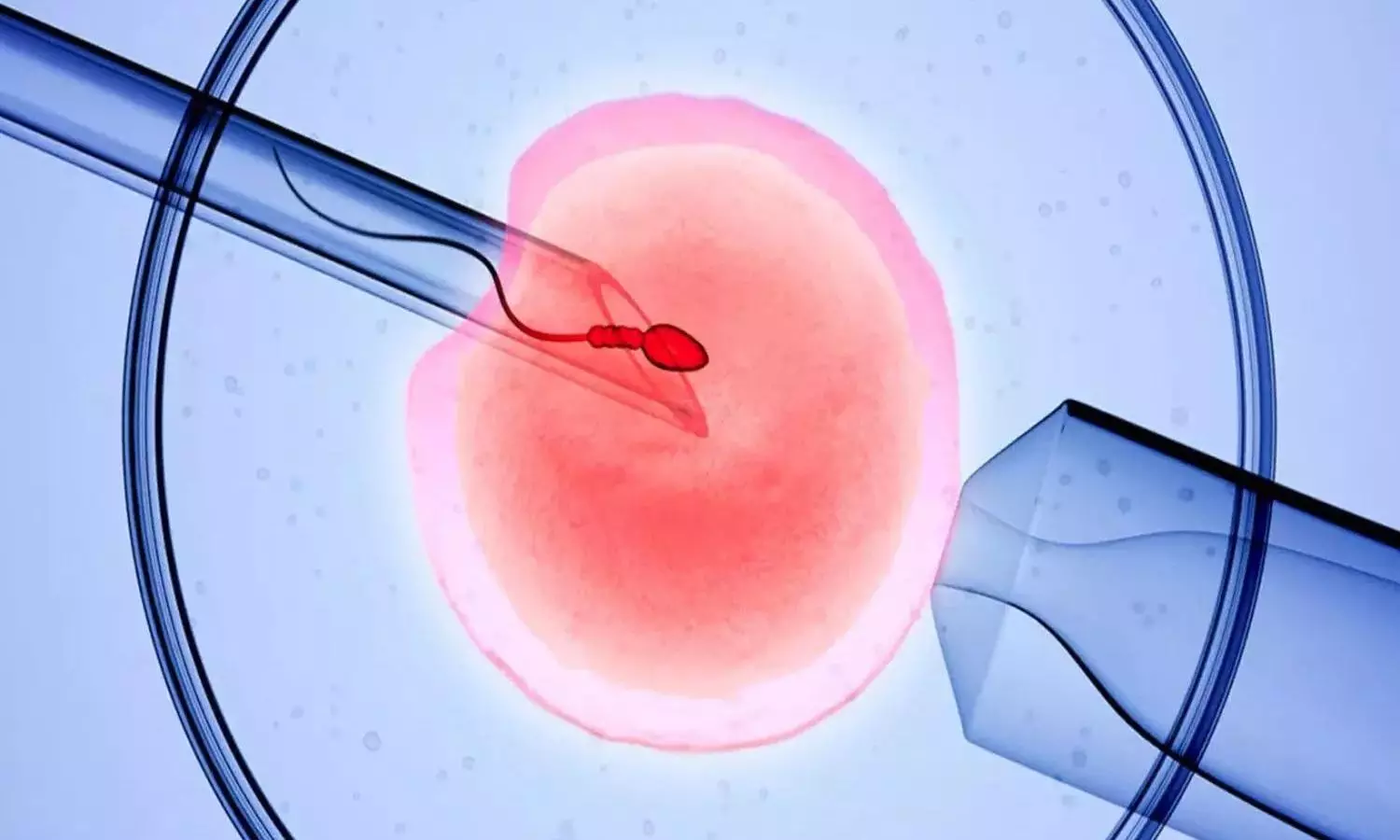
Multiple gestations are the most frequent complications
associated with assisted reproductive techniques (ART). To decrease the rate of
twin and higher order multiple gestations, the elective single-embryo transfer
(eSET) is currently encouraged. However, blastocyst stage SET was still found
to be associated with multiple gestations. The present data revealed that the
frequency of embryo splitting post-eSET is 1.36% with the rate of monozygotic
twin and triplet pregnancies being 0.9-3.1% and 0.048%, respectively. However,
dizygotic twin and triplet pregnancies can also be encountered post-eSET. Both
monozygotic and dizygotic pregnancies can occur in the setting of fresh embryo
transfers, in natural or modified natural frozen embryo transfers (FET), and
rarely in medicated FET cycles. Such events challenge the twinning dogma
proposed by Corner.
Incidence of Zygotic Splitting after SET
Single-embryo transfer is becoming the most favored method
of ART conclusion in recent years as it decreased the complications associated
with multiple gestations. However, multiple gestations in the form of mono- or
dizygotic twinning are still encountered. The classic definition of when one
embryo undergoes fission into 2 or more genetically identical embryos is called
monozygotic splitting, while when 2 different embryos implant, a dizygotic
pregnancy ensures.
The findings of monochorionic and multiple chorionic
pregnancies in blastocyst eSET confirmed the fact that embryo splitting took
place after the transfer. However, not all pregnancies are monozygotic. As per
Osianlis et al., the calculated dizygotic rate in their paper was 0.5% with an
overall Di-Di birth rate of 1%. Based on these numbers, they concluded that 50%
of the multizygotic pregnancies are due to actual embryo splitting while the
other 50% could be explained by concomitant natural conception at the same time
of the ART conception. On another level, the Japanese ART national registry
database along with a survey done by Yamashita et al. documented 122 triplet
pregnancies, of which 46 were single gestational sac pregnancies, 18 were
double gestational sac pregnancies, and 59 were with 3 gestational sacs. It is
worth mentioning that the trichorionic pregnancies had zero fetuses in 9 cases,
1 fetus in 12 cases, 2 fetuses in 9 cases, and three fetuses in 29 cases. One
quadruplet case was also documented.
Chorionicity
Chorionicity refers to the placenta the origin of which can
be determined accurately. Zygosity on the other hand, which is the origin of
the fetus, can be predicted in half of the cases as multiple gestation
pregnancies can originate from one or multiple embryos especially when the sex
of the babies is discordant. Given this fact, same-sex twins or triplets could
be true monozygotic or dizygotic in origin. The only way to accurately diagnose
the zygosity is to do DNA fingerprinting which is expensive and thus not
performed in daily practice.
In contrast, monochorionic multiple gestations are always
monozygotic. Originally, it was thought that the earlier the embryonic
division, the more separate and independent the fetuses were. In other words,
cleavage stage divisions were believed to result in dichorionic diamniotic
pregnancies while blastocyst stage divisions resulted in monochorionic
monoamniotic pregnancies. According to Konno et al., dichorionic pregnancies
were found to be more common with ART. As such, authors can conclude that SET
can result in monozygotic (monochorionic and multichorionic) as well as
dizygotic pregnancies (multichorionic pregnancies).
Risk Factors
Naturally occurring twinning, especially the dizygotic form,
is believed to be linked to a genetic predisposition most commonly located on
chromosome 3. Some ethnicities were found to be more predisposed to dizygotic
twinning where the rate reached 50/1000 in Nigeria. This contrasts with the
naturally occurring monozygotic twinning which was found to be nonaffected by
the ethnicity or the genetic makeup of the couple.
ART on the other hand has increased the incidence of
monozygotic twining. It has been shown that the patient’s young age might
predispose to zygotic twinning while unexplained infertility was found to be
protective. It was proposed that ART associated embryo manipulations such as
FET per se, blastocyst culture, and assisted hatching could be risk factors for
zygotic splitting while the zona manipulation of the oocyte in the form of
intracytoplasmic sperm insemination (ICSI) was not. Interestingly, there was no
difference in the splitting rate neither between the cleavage stage and the
blastocyst stage transfers nor between fresh and frozen embryo transfer cycles.
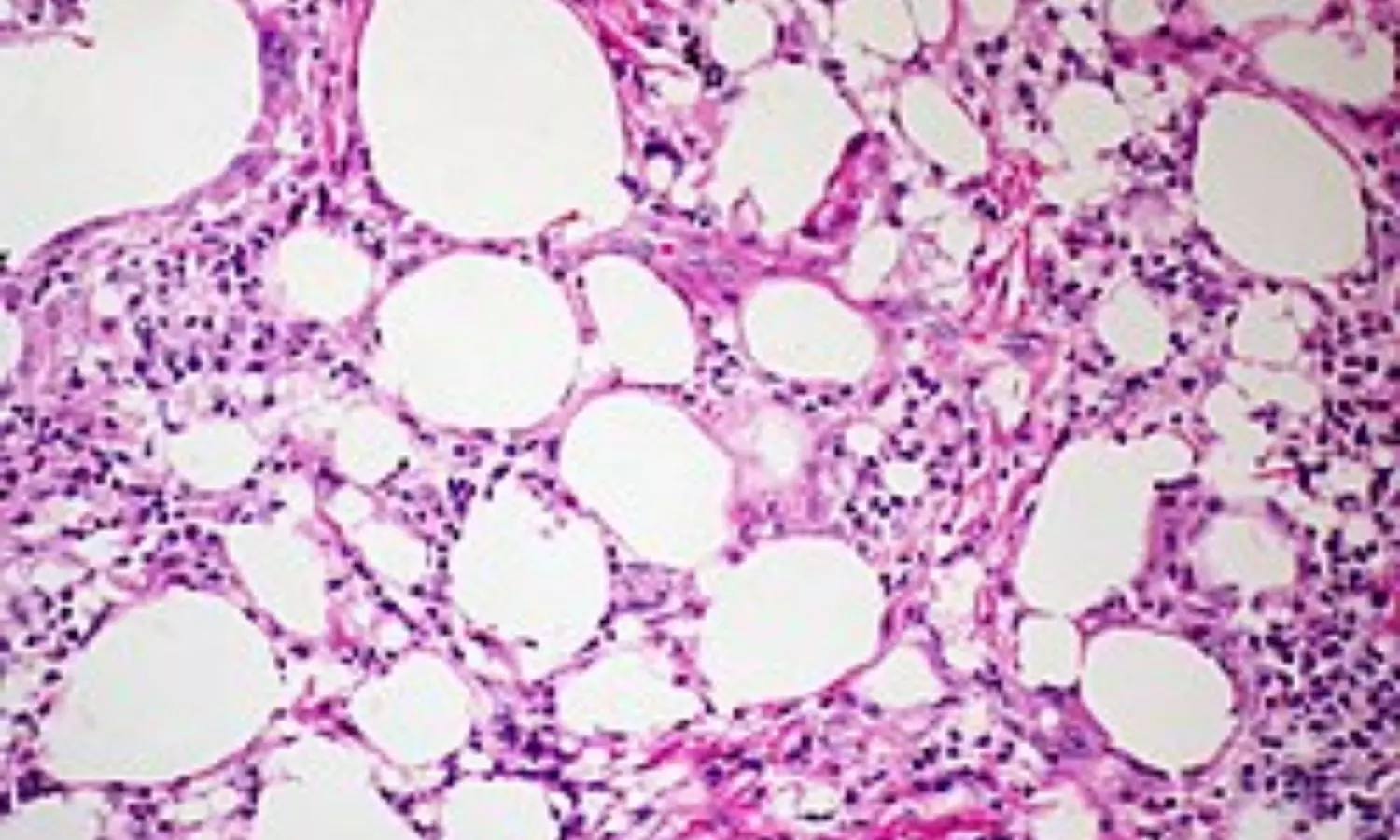
Another risk factor for splitting is a lower inner cell mass
(ICM) grading of B or C. It is thought that loose intercellular connections may
induce the ICM fission. This has been documented through the time-lapse imaging.
The quality of the culture media is also thought to stimulate zygotic
splitting. An increase in the free radicals’ concentration due to increased
glucose concentration in the culture media used for prolonged culture could
lead to ICM splitting at the site of glucose-induced apoptosis of certain
regions of the ICM.
The new sequential culture systems with antioxidant activity
might explain the lack of increase of the rate of embryo splitting despite the
major increase in the number of IVF cycles and embryo transfers worldwide. When
coupled with the improvement in the embryologists training and experience, the
rate of splitting associated with a blastocyst transfer has been found to
decrease. The OR for embryo splitting decreased from 2.2 to 1.7 when comparing
the periods of 2007 to 2010 and 2010 to 2014. Embryo biopsy on the other hand
was not found to increase the risk of embryo splitting contrary to what was
believed before.
Suggested Mechanisms of Division
It has been shown that blastomeres from a 4-cell stage
embryo can develop into an ICM and trophectoderm; hence, any division after
this stage could give rise to 2 or more embryos with an implantation potential.
Of the suggested mechanisms, abnormal cellular axis formation and cytoplasm
folding in the secondary oocyte prior to fertilization or during the actual
fertilization lead to duplication. It is speculated that gonadotropin
stimulation might disrupt the fine balance and gradients of signalling
molecules affecting the polarity of the oocyte. This is thought to lead to the
formation of 2 cells referred to as daughter cells or tertiary oocytes that
could be fertilized. This is speculated to be caused by the displacement of the
meiotic spindle due to oocyte aging postovulation. This disruption might lead
to the duplication of the axes and formation of 2 embryos upon fertilization or
the fission of the ICM into 2 at the blastocyst stage. This theory would be
replaced later on by the formation of 2 zygotes postfertilization of the
secondary oocyte and not 2 blastomeres.
Other studies advocated the fission to happen closer to the
cleavage stage, and thus, the sequence of events happening during hatching
would then explain the type of the twin gestation. If both blastocysts were
released at the same time, then the resultant pregnancy would be a dichorionic
diamniotic twin gestation.
If on the other hand the blastocysts fused with the
conservation of 2 separate ICMs prior to hatching, then monochorionic
diamniotic twins would appear. If complete fusion of the trophectoderm and the
ICM happened, then monochorionic monoamniotic twins would be created.
Another suggestion was that the ICM would split due to
mechanical compression during hatching through the manipulated zona pellucida
of the embryo which is also referred to as atypical hatching. This atypical
hatching is referred to as 8-shaped hatching, which usually takes place when
the embryo is squeezing out through the hatch of the hardened zona pellucida
due to prolonged culture to blastocyst stage and in cryopreserved-thawed
blastocysts especially with the application of the day 3 prehatching protocol.
It is speculated that this phenomenon might also be the culprit for the
monozygotic triplet gestations that have been documented post-SET.
Another possible explanation to dual or even more ICM is the
nature of human blastomere plasticity. Studies have shown that isolated
trophectoderm cells when cultivated could give rise to a whole new embryo with
an implantation potential. As such, if a blastomere gets separated from the
trophectoderm into the blastocele due to low-grade compaction of the
trophectoderm, this blastomere could give rise to an ICM. Theoretically, each
ICM should give rise to a separate fetus with the surrounding amnion while the
chorion develops during the implantation. The mechanism of chorionic
differentiation between mono and higher order chorionicity in monozygotic
pregnancies is still unknown.
Triplets: Possible Explanation
The explanation of embryo splitting into three is
challenging since triplets after SET is a very rare event. What is known so far
is that to have implantation, an embryo with an intact ICM should be present.
The number of the ICM that the embryo has will define the number of fetuses
that will be seen on the pregnancy ultrasound.
The chorionicity of the pregnancy will depend on the number
of zygotes present at the time of implantation. In theory, the chorion should
rise from trophectoderm cells; thus, it would be logical to consider that the
higher the order of the chorionicity, the higher the number of separate embryos
available for implantation.
In the setting of monochorionic triplets, it is believed
that the blastocyst harbors three distinct ICMs. The mechanism of their
creation might be similar to the ones suggested for the monochorionic twin
gestation. The trigger factor for the splitting into 3 and not into 2 is still
unknown. In the setting of the multichorionic triplets, a suggested explanation
might be the complete division of the hatching embryos resulting in 3 and not
only 1 fully hatched embryo.
Another possible explanation for this is if the origin of
the sister ICMs is a trophectoderm blastomere. Since the implantation potential
of reconstructed embryos cannot be tested at this point due to ethical reasons,
one can only postulate that such cellular plasticity might confer to the newly
formed ICM the whole genetic makeup necessary for a successful implantation and
healthy fetal development. The question that arises here is that whether the
embryo initially had multiple ICM followed by trophectoderm splitting upon
hatching or the splitting of the ICM took place during hatching due to the
mechanical pressure exerted by the hardened zona pellucida. The latter might
explain the high incidence of blighted ova in triplet pregnancies. Due to the
abnormal cell division in the embryo(s) as well as increased cellular stress,
the ICM fails to continue itsdivision resulting in a blighted ovum.
Zygotic splitting is a well-described event in ART, yet the
complete mechanism of these events is not completely elucidated. The hypotheses
that authors have so far remain unproven due to the rarity of zygotic splitting
as well as the ethicolegal considerations of human embryo research. The
presence of such incidents necessitates extensive counselling of couples
undergoing SET.
Source: Mokhamad Zhaffal,1 Rania Al Jafari,2 and Anastasia Salame;Hindawi Journal of Pregnancy Volume 2024, Article ID 2686128, 4 pages https://doi.
Powered by WPeMatico