Clinical practice paper recommends alternatives to hysterectomy for uterine fibroids
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

New Delhi: The National Eligibility-Entrance Test Postgraduate (NEET-PG) 2024 counselling had to be kept on hold since the National Board of Examinations in Medical Sciences (NBEMS) had to issue state-specific ranks and both the State and Central counselling had to be conducted together, the secretary of the National Medical Commission (NMC) Dr. B Srinivas informed Education Times recently.
He further mentioned that the pending court case against NBEMS also resulted in the delay in setting the timelines for the entire counselling process for admission to postgraduate medical courses.
“By early November, the counselling for the All India Quota which was kept on hold, has been resumed. Since states have their own ranks, the NBEMS has to issue the state-specific ranks. Both the AIQ rounds at the central level and the state counselling have to be conducted in tandem. The MCC had to withhold the counselling since the NBEMS had to calculate the state-specific ranks over two sessions of NEET PG 2024 where scores at the All-India level were calculated using the normalisation process. This is unlike last year when the exam was conducted over a single session. Moreover, the NBEMS has had a pending court case. This led to the delay in setting the timelines for the whole counselling process,” Dr. Srinivas informed.
Clarifying that the issue of ranks has now been resolved, Dr. Srinivas further mentioned that the counselling will now start at both the Central and State levels.
Also Read: MCC NEET PG 2024 Counselling registrations open, Know how to apply
Meanwhile, due to the pending case before the Supreme Court seeking transparency in the NEET PG 2024 exam and due to the issue concerning the creation of state-specific ranks for PG medical admissions, the counselling has already been postponed and the academic session will now commence late- in November-end.
When asked about this, Dr. Srinivas told Education Times, “There are enough buffers in the system to make up for the academic loss with classes being held over weekends and summer breaks to cope with time constraints in completing the syllabus.”
However, experts have not agreed with this view as many of the doctors pointed out that the delay may create a manpower shortage, considering the fact that the final-year PG students are set to appear for their exams in December and January.
Commenting on this, Dr B Unnikrishnan, dean, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education told ET, “A delayed admission process can push back the start of academic programmes which could result in shortened academic terms or rushed instructional periods, affecting the overall quality of education.”
Some academicians have opined that the admission test for PG medical courses should have been conducted over a single session as only around 2.2 lakh students appeared for the exam that was held online.
“The exam-conducting authority should also bring more transparency in the examination to ensure that the process is fair and accountable. Allowing access to question papers, raw scores, and answer keys can increase candidates’ confidence in the integrity of the examination process. This can help mitigate allegations of malpractice or bias,” added Dr. Unnikrishnan.
After much await, the Medical Counselling Committee recently announced the counselling schedule for NEET PG 2024. As per the official notice, the Counselling will begin on November 7, 2024 when the Round 1 counselling will start. All the rounds of counselling including the Online Stray Vacancy Round will be completed on January 30, 2025.
Also Read: NEET PG Counseling Schedule Announced for 2024: Key Dates and Details
Powered by WPeMatico

Telangana- Through a notification, Kaloji Narayana Rao University of Health Sciences (KNRUHS) has notified regarding the conduct of the 2nd phase of web-based counselling under the Competent authority Quota for vacant seats in B.Sc. (Nursing) 4 YDC course for 2024-25 in affiliated Government, Private Nursing Colleges after 1st phase of counselling. Also, the conduct of the 2nd phase of web-based counselling under the Competent Authority Quota for vacant seats in the Post Basic B.Sc. (Nursing) 2 YDC course for 2024-25 in affiliated Government and Private Nursing Colleges after the 1st phase of counselling.
As per the notification, Candidates whose certificates were uploaded at the time of online registration and provisionally verified by the staff of concerned departments and whose names are notified as eligible candidates in the provisional final merit list for B.Sc. (Nursing) 4 YDC and P.B. B.Sc. (Nursing) 2YDC courses 2024-25 on the KNRUHS official website are eligible to exercise web – options online from the computer with internet connection.
All the eligible candidates whose names are displayed in the Provisional final merit list including PWD candidates on the KNRUHS website can exercise web options for admission into B.Sc (Nursing) 4 YDC and P.B. BSc (Nursing) 4 YDC course till 08th November 2024 upto 3.00 PM.
UNIVERSITY FEES
Allotted Candidates have to pay the University fee of Rs. 6000/- through a payment gateway by using an online payment method such as a Debit Card / Credit Card / Internet Banking and download the allotment letter. Candidates who have paid University fees in the first phase need not pay again. The University Fee and other fees once paid shall not be refunded under any circumstances.
Meanwhile, candidates are hereby informed that final verification of original certificates will be conducted at the allotted college and in case of any discrepancy, the provisional allotment will be cancelled and action may be initiated as per University regulations. Therefore, original certificates will not be returned to candidates unless the candidate discontinues from the course.
To view the notifications, click the link below
Powered by WPeMatico

Researchers have been able to demonstrate that type 2 diabetic patients, when placed on a carbohydrate-restricted diet, are capable of experiencing short-term recovery of beta-cell function, which produces insulin. Researchers in the Journal of Clinical Endocrinology & Metabolism proposed that an eating regimen carbohydrate-restricted helps to rejuvenate the beta-cell function, and therefore one may utilize such an eating habit to potentially improve glycemic control, independent of weight reduction.
Beta-cell dysfunction is an important determinant in the mechanism of developing type 2 diabetes by losing first-phase insulin response. Led by Marian Yurchishin, MS, a PhD student at the University of Alabama at Birmingham, a new study aimed to determine if a carbohydrate-restricted diet could enhance beta-cell function over a short period of intervention. The researchers’ hypothesis was based on the belief that decreasing glucose exposure-to what is considered “glucose toxicity” for the beta cell-may allow for repair and restoration of cell function.
The study consisted of 57 patients with type 2 diabetes who were not on insulin therapy. Ninety-three participants were randomized to a carbohydrate-restricted diet (9% of energy from carbohydrates, 65% from fats) or a higher-carbohydrate diet (55% energy from carbohydrates, 20% from fats). The carbohydrate-restricted group included 5 men and 22 women; mean age 53 years, 17 Black and 10 white. The higher-carbohydrate group included 8 men and 22 women; mean age 55 years, 20 Black and 10 white.
At 12 weeks, the authors noted marked increases in beta-cell function in the carbohydrate-restricted diet group:
• The acute C-peptide response was twice as large in the carbohydrate-restricted group compared with the higher-carbohydrate group (p < 0.01).
• The maximal C-peptide response, an index of the beta-cell’s ability to produce insulin, was 22% larger in the carbohydrate-restricted group (p < 0.05).
• Disposition index, a marker of insulin sensitivity and secretion, was 32% higher in the carbohydrate-restricted group compared with the oral glucose tolerance test (p< 0.05).
• The study also noted race differences in beta-cell function. Maximum C-peptide response was 48% higher in white patients on the carbohydrate-restricted diet compared with those on the higher-carbohydrate diet (p< 0.01), but not in Black patients. This suggests that mechanisms that lead to beta-cell failure may vary by race.
Carbohydrate restriction ameliorates the function of white subjects’ beta cells, particularly of type 2 diabetic subjects. Such a dietary intervention may potentially enhance glycemic control and improve insulin secretions at least in the absence of weight loss. However, the racial differences in beta-cell recovery bode well for further research in the mechanisms that underlie such disparities.
Reference:
Swain, E. (2024, October 22). Effects of a Carbohydrate Restricted Diet on Beta-cell Response in Adults with Type 2 Diabetes, Journal of Clinical Endocrinology & Metabolism (2024). dx.doi.org/10.1210/clinem/dgae670
Powered by WPeMatico
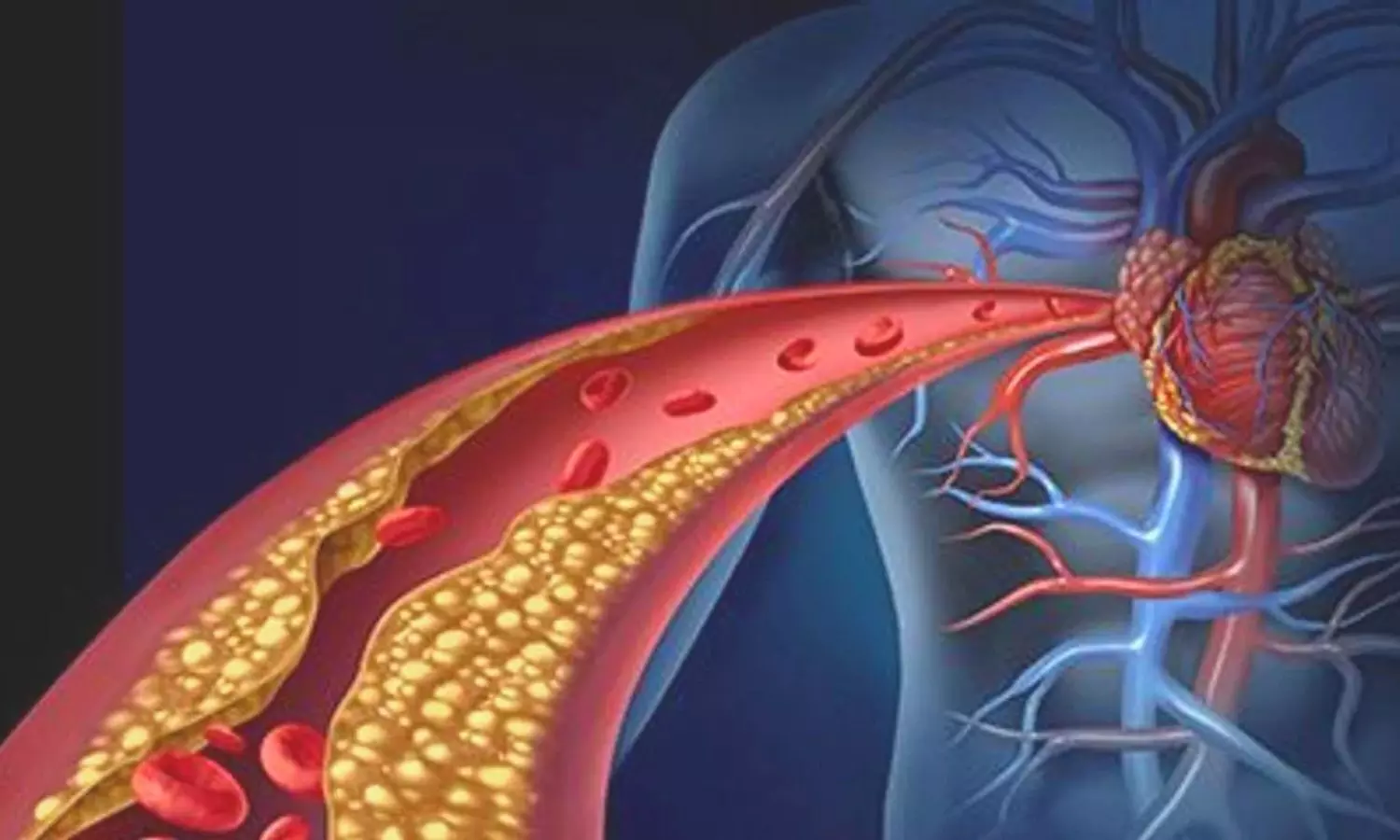
USA: A recent editorial comment in the Journal of the American College of Cardiology: Cardiovascular Imaging highlights the evolving role of coronary artery calcium (CAC) scoring as a critical tool for evaluating patients with stable chest pain. Traditionally, clinicians relied on the Diamond-Forrester model, which estimates the likelihood of obstructive coronary artery disease (CAD) based on age, sex, and angina characteristics. However, contemporary analyses suggest that this model may overestimate CAD probabilities and fail to incorporate newer testing methods.
The editorial references current guidelines, including the 2021 American Heart Association/American College of Cardiology Multisociety Chest Pain Guidelines, which advocate for integrating cardiovascular risk factors and CAC scores to refine the pretest probability (PTP) of CAD in patients with chest pain. According to the editorial authors David E. Winchester, and Mahmoud Al Rifai (both from USA), this is particularly relevant given that stable chest pain can indicate varying levels of underlying cardiovascular issues.
In the featured study by Rasmussen et al., which included 4,371 patients undergoing anatomical assessment for CAD, the researchers assessed the effectiveness of different PTP models. The findings indicated that both risk factor-weighted clinical likelihood (RF-CL) and CAC score-weighted clinical likelihood (CACS-CL) models provided significantly improved predictions for hemodynamically obstructive CAD compared to the basic PTP model. Notably, CAC scoring demonstrated a 98.9% negative predictive value for obstructive CAD, making it an effective tool for ruling out serious conditions.
The editorial emphasizes that while CAC scoring alone can serve as a valuable screening tool, it is crucial to consider individual clinical characteristics to minimize misclassification of CAD status. With nearly half of patients presenting with stable chest pain potentially having a CAC score of zero, the absence of coronary artery calcium suggests that further testing may be unnecessary.
Future recommendations from the 2023 Appropriate Use Criteria for multimodality imaging in chronic coronary disease reinforce this perspective. These guidelines suggest that for patients with low to intermediate PTP for CAD, a negative CAC score could warrant deferring further testing. Conversely, the presence of CAC might indicate the need for additional assessments, such as coronary computed tomography angiography or myocardial perfusion imaging.
Despite its promise, challenges remain in determining which patients would benefit most from CAC scoring. The editorial underscores the need for ongoing research to evaluate various PTP strategies and refine how CAC can be used effectively in clinical practice. Ultimately, the integration of CAC scoring into routine assessments could lead to more accurate and safer management of patients with stable chest pain, improving overall cardiovascular care.
Reference:
Winchester DE, Al Rifai M. Coronary Artery Calcium as a Gatekeeper for Patients With Stable Chest Pain. JACC Cardiovasc Imaging. 2024 Oct;17(10):1211-1213. doi: 10.1016/j.jcmg.2024.05.025. Epub 2024 Aug 7. PMID: 39115500.
Powered by WPeMatico

Germany: A recent multicenter randomized clinical trial (Landi-SEP) has revealed promising results for the use of Landiolol, an ultra-short-acting beta-blocker, in managing heart rate in patients experiencing septic shock and persistent tachycardia. The findings suggest that landiolol can effectively reduce heart rate without increasing the need for vasopressors after 24 hours of treatment.
“Landiolol effectively lowers and sustains heart rate for 24 hours in patients with septic shock and persistent tachycardia, all while avoiding an increased requirement for vasopressors.,” the researchers wrote in Intensive Care Medicine.
Septic shock is a severe condition characterized by a significant drop in blood pressure due to infection, leading to organ dysfunction. Patients often present with persistent tachycardia, making heart rate management a crucial aspect of their treatment. Traditional therapies for controlling heart rate have had mixed results, highlighting the need for effective alternatives.
Against the above background, Sebastian Rehberg, University Hospital of Bielefeld, Bielefeld, Germany, and colleagues examined whether heart rate (HR) control could be achieved without raising the need for vasopressors by using the titratable, highly selective ultra-short-acting β1-blocker landiolol.
For this purpose, the researchers conducted a randomized, open-label, controlled trial across 20 sites in seven European countries from 2018 to 2022. They evaluated the efficacy and safety of landiolol in adult patients experiencing septic shock and persistent tachycardia. Participants were randomly assigned to receive either landiolol combined with standard treatment (n = 99) or standard treatment alone (n = 101).
The primary endpoint focused on achieving a heart rate within the range of 80 to 94 beats per minute and maintaining that rate without increasing the need for vasopressors during the first 24 hours following the start of treatment. Key secondary endpoints included 28-day mortality rates and the occurrence of adverse events.
The findings are summarized as follows:
The study revealed that the ultra-short-acting beta-blocker landiolol effectively reduced and maintained heart rate in patients with septic shock and persistent tachycardia without increasing the need for vasopressors after 24 hours. However, there were no significant differences in adverse events or clinical outcomes, including 28-day mortality, compared to standard care.
“These findings suggest that a strategy focused on strict heart rate reduction to below 95 beats per minute may not be appropriate for all patients with septic shock and persistent tachycardia. Further research is necessary to identify specific patient phenotypes within this population that may clinically benefit from heart rate control,” the researchers concluded.
Reference:
Rehberg, S., Frank, S., Černý, V. et al. Landiolol for heart rate control in patients with septic shock and persistent tachycardia. A multicenter randomized clinical trial (Landi-SEP). Intensive Care Med 50, 1622–1634 (2024). https://doi.org/10.1007/s00134-024-07587-1
Powered by WPeMatico
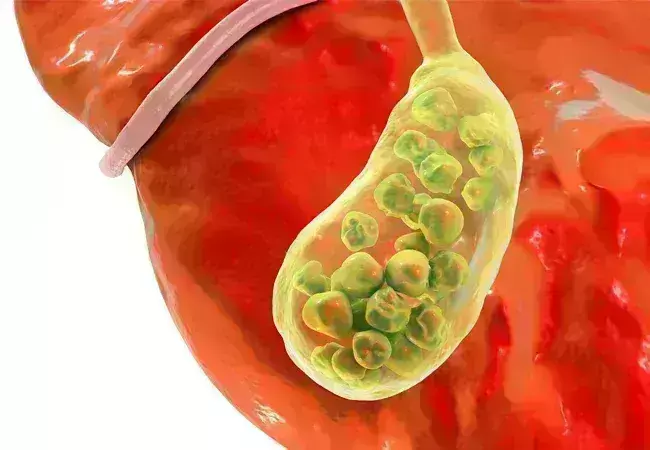
A recent study revealed that the neutrophil-to-high-density
lipoprotein cholesterol ratio (NHR) could be a useful tool to identify individuals
at risk of developing gallstone disease (GSD). NHR can be used as an easy and
cost-effective tool for the early detection of individuals at GSD as per a
study published in the journal Lipids in Health and Disease.
Gallstone disease (GSD) is one of the most frequent and expensive
gastrointestinal disorders caused by cholesterol, bile pigment, and mixed stones,
with cholesterol stones outranking the three. They are caused by the oversaturation
of calcium salts and cholesterol in bile, leading to cholesterol deposits. Gallstones
have an increased risk of cancer. The neutrophil to high-density lipoprotein
cholesterol ratio (NHR) is a novel comprehensive marker of inflammatory
responses and lipid metabolism that can detect cardiovascular disease,
depression, acute biliary pancreatitis, and hepatocellular carcinoma. Previous research
has shown that inflammatory reactions can promote gallstone formation by
altering protein and lipid metabolic pathways and increasing bile acid salt
concentrations by involving neutrophils and lipids. As there is ambiguity on
the association between NHR and gallstones, researchers from Zhejiang Chinese
Medical University, China conducted a study on the relationship between
gallstone disease (GSD) and the neutrophil-to-high-density lipoprotein
cholesterol ratio (NHR) in American patients with gallstones.
The study was conducted by collecting data from the National
Health and Nutrition Examination Survey (NHANES) between 2017–2020. Data was collected
through interviews, health exams, and lab tests. Out of 15,560 participants,
7,894 were included in the study. NHR calculation was done by dividing the neutrophil
count by HDL-C levels and the participants were divided into 3 NHR categories
based on the count. Gallstone data was reported by the participants based on
the physician’s diagnosis. Unadjusted and adjusted logistic regression models
were used to evaluate the association between NHR and GSD.
Key findings:
Thus, the study concluded that a higher NHR is associated
with a greater likelihood of having GSD and NHR can be used as a low-cost
method to screen patients at risk of GSD. NHR can also be used in early
diagnosis so that preventive measures can be taken to reduce the risk of gallstones.
Further reading: Ma
D, Ma H, Li Y, Yang L. Association between Neutrophil-to-high-density
lipoprotein-cholesterol ratio and gallstones: insights from the national health
and nutrition examination survey (2017-2020). Lipids Health Dis.
2024;23(1):355. Published 2024 Oct 31. doi:10.1186/s12944-024-02349-w.
Powered by WPeMatico

Assessing right ventricular diastolic function is crucial in cardiac surgery, as it significantly impacts long-term prognosis. Typically, RV diastolic dysfunction is evaluated using criteria from the American Society of Echocardiography (ASE) or the British Society of Echocardiography (BSE) via transthoracic echocardiography (TTE). Nevertheless, transesophageal echocardiography (TEE) is the primary method for perioperative evaluation during cardiac surgery. Recent study aimed to assess the agreement between transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) in grading right ventricular diastolic dysfunction (RVDD) using criteria from the American Society of Echocardiography (ASE) and the British Society of Echocardiography (BSE).
The study included 81 patients undergoing cardiac surgery. TTE and TEE measurements were taken within 10 minutes of each other, under similar hemodynamic, anesthetic, and ventilatory conditions. RVDD grading was performed separately using TTE, TEE mid-esophageal right ventricular inflow-outflow (MERVIO) view, and TEE deep transgastric right ventricular inflow-outflow (DTGRVIO) view, based on both ASE and BSE criteria. According to the ASE criteria, disagreement of ≥1 RVDD grade was seen in 53.1% of patients when comparing TTE and TEE-MERVIO, and in 39.5% when comparing TTE and TEE-DTGRVIO. The weighted kappa was 0.14 and 0.3, respectively, indicating poor to fair agreement. Using the BSE criteria, disagreement occurred in 11.1% and 14.8% of patients when comparing TTE with TEE-MERVIO and TEE-DTGRVIO, respectively, with unweighted kappa of 0.25 and 0.26, indicating fair agreement.
Limits of Agreement and Rater Consistency
The study found wide limits of agreement between individual 2D and Doppler parameters measured by TTE and TEE. There was almost perfect agreement between independent raters for RVDD grading using both TTE and TEE. In conclusion, the study revealed at best only fair agreement between TTE and TEE in grading RVDD. The authors recommend further research to develop a TEE-based algorithm for grading RVDD and to evaluate the prognostic effectiveness of perioperative TEE for predicting adverse clinical outcomes associated with RVDD.
Key Points
1. The study aimed to assess the agreement between transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) in grading right ventricular diastolic dysfunction (RVDD) using criteria from the American Society of Echocardiography (ASE) and the British Society of Echocardiography (BSE).
2. The study included 81 patients undergoing cardiac surgery, with TTE and TEE measurements taken within 10 minutes of each other under similar hemodynamic, anesthetic, and ventilatory conditions. RVDD grading was performed separately using TTE, TEE mid-esophageal right ventricular inflow-outflow (MERVIO) view, and TEE deep transgastric right ventricular inflow-outflow (DTGRVIO) view, based on both ASE and BSE criteria.
3. Using the ASE criteria, there was a disagreement of ≥1 RVDD grade in 53.1% of patients when comparing TTE and TEE-MERVIO, and in 39.5% when comparing TTE and TEE-DTGRVIO, with poor to fair agreement as indicated by the weighted kappa values.
4. Using the BSE criteria, disagreement occurred in 11.1% and 14.8% of patients when comparing TTE with TEE-MERVIO and TEE-DTGRVIO, respectively, with fair agreement as indicated by the unweighted kappa values.
5. The study found wide limits of agreement between individual 2D and Doppler parameters measured by TTE and TEE, but almost perfect agreement between independent raters for RVDD grading using both TTE and TEE.
6. The authors conclude that the study revealed at best only fair agreement between TTE and TEE in grading RVDD, and they recommend further research to develop a TEE-based algorithm for grading RVDD and to evaluate the prognostic effectiveness of perioperative TEE for predicting adverse clinical outcomes associated with RVDD.
Reference –
Singh N C, Biswas I, Kumar B, et al. (October 07, 2024) The Agreement Between Transthoracic and Transesophageal Echocardiography in the Assessment of Right Ventricular Diastolic Dysfunction Grades in Adult Patients Undergoing Cardiac Surgery: A Prospective Observational Study.
Cureus 16(10): e70976. DOI 10.7759/cureus.70976
Powered by WPeMatico

A new study published in the Clinical and Experimental Dermatology journal showed that estradiol with minoxidil (EMX) may raise the risk of irregular menstruation in individuals with female pattern hair loss (FPHL) which is also known as female androgenetic alopecia (AGA). The variables that influence miniature follicle development and the pathophysiology of FPHL are yet unknown. There is proof that genetic, hormonal, and environmental factors also play a part in male AGA, in addition to the most obvious impact of androgens. Women who have thick, healthy hair are more likely to feel secure, confident, and capable of change. They are also more likely to engage with others.
The prevalence of female pattern hair loss is high and has a detrimental effect on one’s quality of life. The most effective treatment for FPHL is minoxidil, however it is more difficult to treat than male pattern hair loss. Several trials treated FPHL with 17α-estradiol solution, either by alone or in combination with minoxidil, with varying degrees of success. Thus, this study evaluated the safety and effectiveness of topical 17α-estradiol 0.01% with minoxidil 2% against minoxidil 2% in the treatment of FPHL, by Nermeen Ibrahim Bedair and colleagues.
For this study, 43 women with FPHL were instructed to apply a spray-on solution comprising either 17α-estradiol 0.01% plus minoxidil 2% (EMX group) or minoxidil 2% alone (MX group) blindfolded twice a day. The course of treatment lasted six months. After baseline and after the conclusion of the therapy, trichoscopic and clinical evaluations were conducted.
Both groups displayed indicators of improvement at the conclusion of the therapy session. The EMX group outperformed the MX group in terms of improvement metrics, however, this difference was not statistically significant. Menstrual abnormalities were more common among the patients of EMX group. Overall, the findings of this study suggest that a 0.01% 17α-estradiol and 2% minoxidil solution does not appear to provide a statistically significant benefit over minoxidil alone, and there may be a greater chance of related menstrual abnormalities in the treatment of FPHL.
Reference:
Bedair, N. I., EL-Komy, M. H. M., Mohamed, R. E., Shamma, R. N., & Amer, M. A. (2024). Efficacy and safety of combined topical ethinylestradiol with minoxidil versus topical minoxidil in female pattern hair loss. A trichoscopic randomized controlled clinical study. In Clinical and Experimental Dermatology. Oxford University Press (OUP). https://doi.org/10.1093/ced/llae436
Powered by WPeMatico
