Otolaryngology Surgical Patients: Study Reveals Low VTE Risk with Simplified Risk Assessment Models
USA: Recent research published in The Laryngoscope journal has shed light on venous thromboembolism (VTE) risk in patients undergoing otolaryngology surgeries. It reveals that this patient population generally faces a low risk of postoperative complications related to blood clots.
“Patients undergoing otolaryngology surgery have a low risk of postoperative VTE, with only two cases reported among 869 individuals studied. These findings support using shorter and simpler risk assessment models (RAMs) such as COBRA and Pannucci-NSQIP as effective alternatives to the more complex Caprini score for identifying ambulatory patients at risk,” the researchers reported.
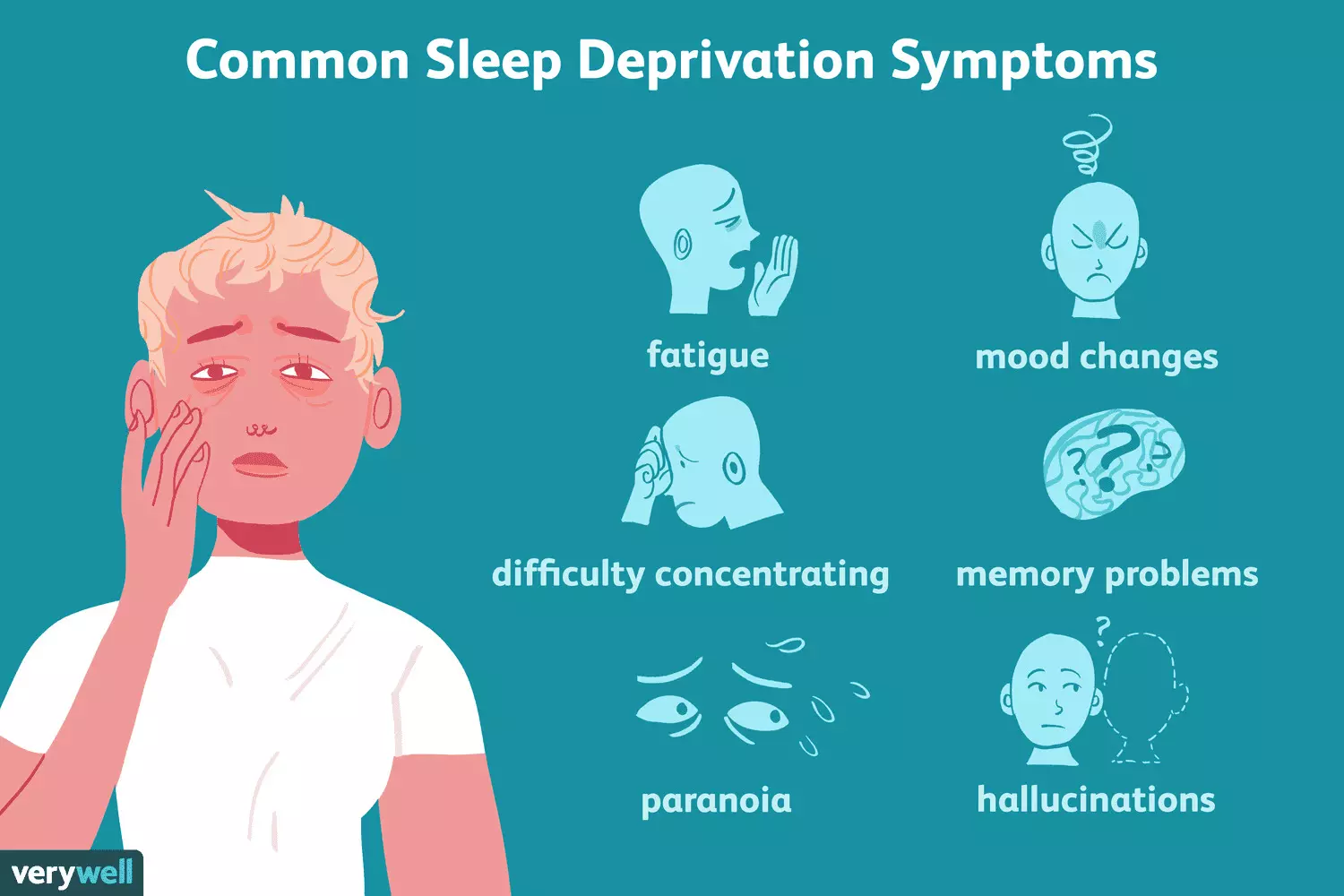
Venous thromboembolic events are a significant concern after surgery, contributing to complications, longer hospital stays, and higher healthcare costs. Current guidelines for prevention focus on the 2005 Caprini score, a tool designed to identify patients at risk for VTE. Although the Caprini RAM has been validated in various surgical specialties, most otolaryngology procedures are performed on an outpatient basis.
To address this, simpler RAMs like the COBRA scoring system and Pannucci-NSQIP have emerged. The study evaluates how well these three models—Caprini, COBRA, and Pannucci-NSQIP—stratify risk among patients undergoing otolaryngology surgeries. Rachel E. Weitzman, Department of Otolaryngology-Head and Neck Surgery, New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, New York, U.S.A., and colleagues aimed to determine the most effective approach to assess VTE risk in this patient population.
For this purpose, the researchers conducted a retrospective chart review of 869 patients who underwent surgery by Weill Cornell faculty otolaryngologists between June and December 2022. They collected data on patient demographics, VTE risk factors, admission status, types of surgeries, and postoperative events. Risk assessment model scores were calculated for each patient.
To evaluate differences in VTE risk scores, the researchers used Wilcoxon and Kruskal–Wallis rank-sum tests based on the type of procedure and admission status. They applied Spearman’s correlation to examine the agreement between the three scoring systems—Caprini, COBRA, and Pannucci-NSQIP. Additionally, multivariate linear regression analyses were conducted to identify which variables influenced the scores of the Caprini, COBRA, and NSQIP RAMs.
The following were the key findings of the study:
A total of two patients experienced postoperative venous thromboembolism.
There is a strong positive correlation between the Caprini and COBRA RAMs, even when analyzed by admission status; however, this correlation weakens in the inpatient group.
A moderate positive correlation exists between the Caprini and Pannucci-NSQIP RAMs across the entire patient cohort, but this correlation is not observed within the inpatient population.
“Patients undergoing otolaryngology surgery have a low risk of experiencing postoperative VTE. The Caprini, Pannucci-NSQIP, and COBRA risk assessment models effectively identify ambulatory patients at risk for postoperative VTE. Notably, simpler models like COBRA and Pannucci-NSQIP can serve as practical alternatives to the more complex Caprini RAM,” the researchers concluded.
Reference:
Weitzman, R. E., Zhao, K., Sclafani, M. S., Srinivasan, Y., Stein, E., Cole, A., & Sclafani, A. P. Venous Thromboembolism Risk Assessment in Inpatient and Ambulatory Otolaryngology Surgical Patients. The Laryngoscope. https://doi.org/10.1002/lary.31856
Powered by WPeMatico