Esote group to set up Medical imaging manufacturing facility in Noida

Noida: Esaote Group, a leading Italian innovator in medical imaging, ultrasound technology, dedicated magnetic resonance imaging (MRI), and healthcare IT solutions, has strengthened its footprint in India with the opening of a new manufacturing facility in New Delhi (B-15, Sector 60, Noida, Uttar Pradesh). The facility, managed by Esaote Asia Pacific Diagnostic Private Limited, will focus on producing a full range of advanced ultrasound systems for the Indian market.
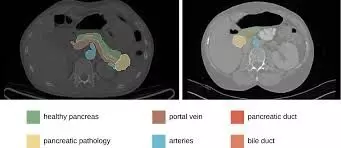
According to the PTI report, the new Esaote manufacturing site will produce – for the Indian market – a full range of advanced ultrasound series – My Lab A, My Lab E series and Compact Portable Ultrasounds – as “Made in India”, which will be marketed shortly after completion of regulatory and quality assurance processes by the relevant local bodies.
These ultrasound systems are the latest results of Esaote’s R&D efforts. They integrate the Augmented Insight functions and provide users with an innovative touchscreen control panel to significantly increase workflow. In addition, they also meet most demanding healthcare professionals’ needs with their compact footprint, battery-operated, lightweight and mobile design.
Also Read:SPMCIL donates Rs 65.77 Lakh Medical Equipment to Kakinada hospitals
The combination of AI-based features and advanced imaging technology will empower Indian healthcare professionals to make confident, informed decisions, ensuring accurate diagnostic outcomes.
For Esaote, the new production plant is a strategic choice to increase its presence in a market with strong growth prospects, where the Italian company has been operating for over 20 years. It also goes hand in hand with the care and empathy with which Esaote approaches its daily work worldwide to improve people’s well-being through technology, inclusion and the promotion of a sustainability culture.
“Consolidating our presence in key markets, where the Esaote brand has been known for many years, through on-site production and the creation of a local supply chain, is part of the international development strategy and reflects the principles of environmental and social sustainability that guide us in our daily actions, in line with the Global Compact,” said Franco Fontana, CEO of Esaote S.p.A.
“What gives us confidence is our innovative spirit, our customer focus, our growth mindset, the Esaote brand and a team that is not afraid to take on the challenges ahead and enjoys creating value for customers and partners. Nothing is more powerful than Esaote Group coming together and writing a new chapter in India with great ‘Italian innovation and Design’ combined with ‘Indian Skills and India Digitalization’,” said Dheeraj Nasa, Country Business Manager Sales APAC Region, news agency PTI reported.
Esaote Group is a leader in medical imaging (ultrasound, MRI and diagnostic process management software). At the end of 2023, the Group had 1,250 employees, half of which are based in Italy. With facilities in Genoa and Florence and its own production and research units in Italy and the Netherlands, Esaote is present in over 100 countries worldwide.
Also Read:AIIMS Delhi to establish Centralised Procurement System
Powered by WPeMatico