Dexamethasone with Vitamin B12 reduces postoperative pain in lumbar disc herniation patients, reveals study

A recent study published in the Journal of Orthopaedic Surgery and Research found that combining dexamethasone and vitamin B12 (VB12) through epidural injection can significantly improve early postoperative outcomes for patients undergoing percutaneous endoscopic interlaminar discectomy (PEID).
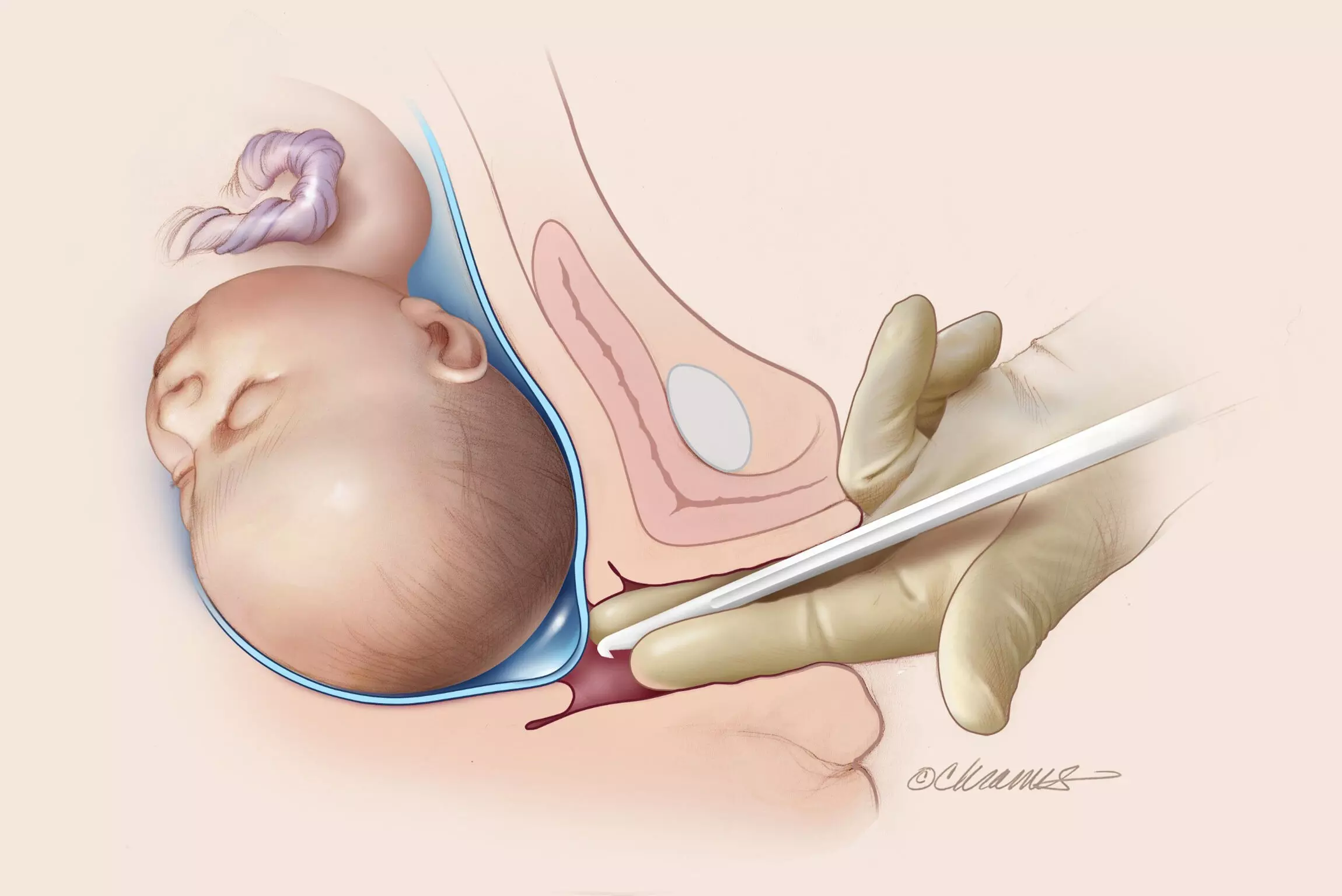
PEID is a minimally invasive procedure used to treat lumbar disc herniation (LDH). While it is generally effective, some patients experience residual pain post-surgery, impacting their recovery and overall quality of life. The study investigated whether supplementing PEID with epidural injections of dexamethasone and VB12 could reduce postoperative pain and improve recovery metrics.
This study enrolled patients who had undergone PEID for LDH and randomly divided them into 2 groups where one was the single surgery (SS) group, which only received PEID and the other was combined treatment (CT) group, which received both the surgery and an epidural injection of dexamethasone and VB12. The evaluation criteria included the Visual Analog Scale (VAS) for pain, the Japanese Orthopaedic Association (JOA) score for functional assessment, and the Oswestry Disability Index (ODI) for measuring disability. Other important metrics included the expression levels of serum inflammatory factors, adverse surgical events, postoperative hospitalization duration, and overall recovery according to the modified MacNab criteria.
The results indicated that patients in the CT group experienced significantly lower VAS scores for low back and leg pain at 1, 3, and 7 days post-surgery when compared to the SS group (P < 0.05). Also, 7 days after surgery, JOA and ODI scores reflected greater improvements in the CT group by underlining improved functional recovery and reduced disability (P < 0.05). Although there were no significant differences at other time points, early postoperative pain management was notably better in the CT group.
Serum analysis revealed that inflammatory markers were lower in the CT group 3 days after surgery by suggesting that the combined treatment played a role in moderating the inflammatory response (P < 0.05). This may contribute to the reported reductions in pain and shorter hospital stays for patients in the CT group (P < 0.05).Both groups had a high rate of positive outcomes, with 89.3% in the SS group and 92.2% in the CT group achieving favorable recovery (P = 0.945) which indicated the overall safety of the combined treatment. Overall, the addition of dexamethasone and VB12 via epidural injection can effectively reduce early postoperative pain, reduce inflammation, and improve initial recovery after PEID.
Reference:
He, C., Li, J., Hu, W., Xiao, B., Fan, T., Zhou, J., Shuang, F., & Li, H. (2024). Effects of dexamethasone combined with vitamin B12 on percutaneous endoscopic interlaminar discectomy early outcomes: a randomized controlled trial. In Journal of Orthopaedic Surgery and Research (Vol. 19, Issue 1). Springer Science and Business Media LLC. https://doi.org/10.1186/s13018-024-05210-z
Powered by WPeMatico