Lyophilized Amniotic Membrane Patch Primary Procedure in Myopic Traction Maculopathy with Macular Detachment, finds study
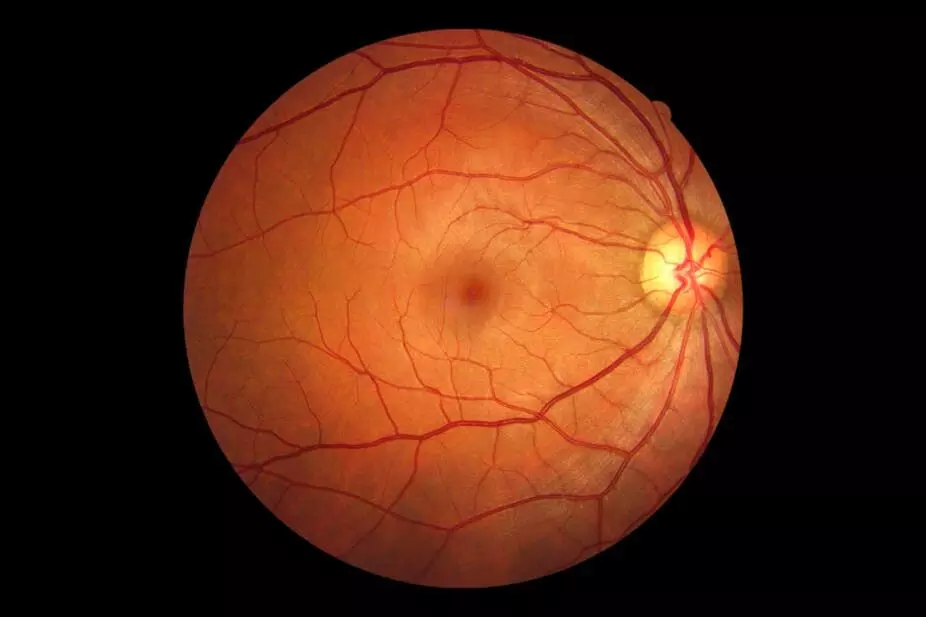
Maculopathy secondary to pathologic myopia (PM) is
increasingly causing visual impairment and blindness worldwide. PM is an ocular
disorder characterized by a spherical equivalent (SE) of more than – 6.0
diopters (D) or by an axial length (AL) of more than 26.5 millimeters (mm). PM
is associated with myopic maculopathy (MM) or myopic tractional maculopathy
(MTM), a disorder that encompasses a spectrum of retinal abnormalities in
patients with high myopia, including macular foveoschisis and macular hole.
Myopic foveoschisis consists of the progressive separation of the layers of the
retina, which are connected by Müller cells. However, when foveoschisis
progresses, it can lead to a macular hole.
Maculopathy secondary to pathologic myopia (PM) is
increasingly causing visual impairment and blindness worldwide. PM is
associated with tractional maculopathy that ranges from macular foveoschisis to
macular hole. These disorders are treated with different options that offer
variable results, reflecting the need for new techniques that address myopic
maculopathy with consistent outcomes.
This diversity of treatments with variable results reflects
the need for new techniques that address myopic maculopathy with consistent
results. In addition, good preoperative visual acuity and the absence of
preoperative foveal detachment are significant predictors of good visual
prognosis, which is why surgical intervention before the development of macular
complications may improve visual outcomes. However, this is not the reality in
the clinical setting, where patients present with advanced cases, foveal
detachment, and poor visual acuity. It has been reported that the human
amniotic membrane (HAM) is safe for intraocular use and to promote retinal
healing; other authors proposed the use of a thin layer of lyophilized amniotic
membrane (LAM) as a patch (LAMPatch) to temporarily block retinal breaks,
reporting good tolerance on the retinal surface. Based on this, Ramirez-Estudillo
et al presented a novel technique using the lyophilized amniotic membrane as an
adjuvant in pars plana vitrectomy in patients with FD, MH, and MHRD.
Since human amniotic membrane (HAM) has been reported to be
safe for intraocular use and to promote retinal healing, it was incorporated as
an adjuvant in pars plana vitrectomy in patients with different tractional
disorders related to myopia. This work presents a prospective, consecutive case
series of seven patients with high myopia who underwent a 25-gauge vitrectomy
with ILM peeling and HAM transplantation.
Tractional myopic degeneration with foveoschisis and
concurrent tangential traction represents a significant challenge since the
standard of care, PPV plus limitorhexis, fails to maintain the retina attached
to the posterior pole. For this purpose, several scleral buckling options have
been developed, as previously mentioned, but at least in our country, these
options are not readily accessible. For example, amniotic membrane can be found
in three presentations: fresh, cryopreserved and freeze-dried. The fresh
variety is difficult to obtain, and as a human-derived tissue, entails
infectious risks and its regulatory and logistics management are complex. These
disadvantages gave rise to the cryopreserved membrane, which is widely
available and is the one that has been broadly used in ophthalmology, including
as a plug transplanted into the subretinal space. Due to the above, LAMPatch is
a valuable option. It reduces tangential traction by using an amniotic membrane
graft approved and used for other types of ocular surgeries, especially of the
anterior segment. The utility of this graft is that it works as a patch that
maintains the adherence of the posterior pole to the choroid and sclera;
specifically, it serves as a scaffold to increase the adhesion surface without
which tangential traction would again pull the retina, causing retinal
detachment.
It is relevant to mention that in addition to this
advantage, this technique is not more complicated than conventional vitrectomy
plus limitorhexis since it only adds one step: the amniotic membrane placement.
However, amniotic membrane handling requires a learning curve since it is essential
to keep the media dry to avoid folding. Specifically, the vitreous cavity must
be completely free of fluid to insert the amniotic membrane so that it does not
fold, and the surgeon can unfold it over the desired anatomical location.
Finally, although the anatomical results in our case series are like those
observed after PPV plus limitorhexis, the great differentiator of this
technique is that the permanence of tissue at six months is very stable, unlike
the recurrence of traction with conventional surgery. This functional success
translates into a gain and maintenance of visual acuity superior to vitrectomy
plus limitorhexis; up to now, the results authors report from the 6-month
follow-up are excellent both anatomically and functionally.
Lyophilized amniotic membrane as an additional step after
vitrectomy with limitorhexis, provides structural and clinical stabilization by
OCT at the 6-month follow-up in a series of cases with FD, MH, and MHRD.
Although longer-term structural and functional follow-up is required, study
results laid the groundwork for a prospective, randomized, controlled clinical
study
Source: Ramirez-Estudillo et al; Clinical Ophthalmology
2024:18 2473–2480
Powered by WPeMatico