Vitamin D supplementation may lower BP in overweight elderly: Study

Vitamin D supplementation may lower BP in overweight elderly suggests a study published in the Journal of the Endocrine Society.
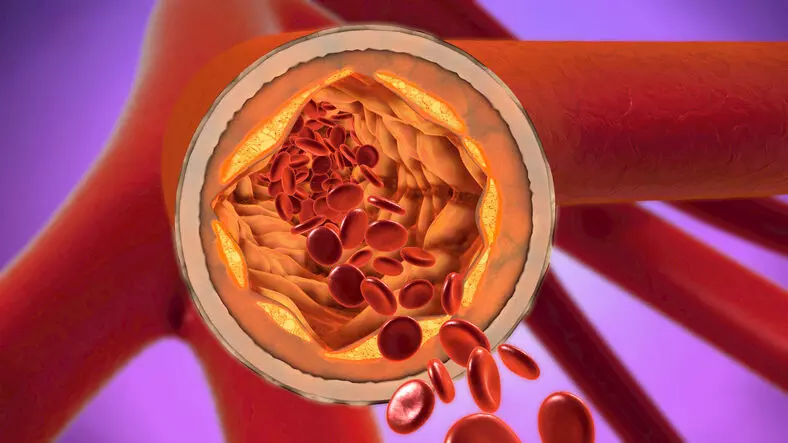
Supplementation with vitamin D and calcium can reduce systolic and diastolic blood pressure in older individuals with overweight, particularly in those with a body mass index (BMI) > 30 and those diagnosed with hypertension. Large cohort data have provided epidemiologic evidence linking vitamin D deficiency to a higher risk for cardiovascular disorders, including hypertension; however, evidence on the beneficial effects of vitamin D supplementation on blood pressure outcomes remains inconclusive. A post hoc analysis of a randomized controlled trial was conducted to investigate the effect of two doses of cholecalciferol (vitamin D3) on blood pressure in individuals aged 65 years or older with a BMI > 25 and serum vitamin D levels of 10-30 ng/mL. A total of 221 participants were recruited through outpatient departments, clinics, and advertisements in the greater Beirut area and received calcium supplementation in combination with either a low dose (600 IU/d, as recommended by the Institute of Medicine [IOM]) or a high dose (3750 IU/d) of vitamin D3. Blood pressure measurements were taken at baseline, 6 months, and 12 months using a SureSigns VS3 monitor. Participants were also stratified by BMI and hypertension status to assess the effects of vitamin D and calcium on blood pressure. Systolic and diastolic blood pressures were significantly reduced with vitamin D supplementation in the overall cohort (mean difference, 3.5 and 2.8 mm Hg, respectively; P = .005 and P = .002, respectively), with the effect more prominent in those in the high-dose vitamin D group. Participants with a BMI > 30 experienced reductions in both systolic and diastolic blood pressures in the overall cohort (P < .0001 and P = .01, respectively); although the systolic blood pressure was significantly reduced with both high- and low-dose vitamin D, the diastolic blood pressure decreased in the high-dose group only. Patients with hypertension benefited from all doses of vitamin D, regardless of the BMI. Systolic blood pressure at 6 and 12 months was significantly predicted by BMI and baseline systolic blood pressure measurements, although not by the dose of vitamin D received.
“The study found vitamin D supplementation may decrease blood pressure in specific subgroups such as older people, people with obesity, and possibly those with low vitamin D levels,” said study author, Ghada El-Hajj Fuleihan, MD, MPH, of the American University of Beirut Medical Center in Beirut, Lebanon, in a news release. “High vitamin D doses compared to the IOM’s recommended daily dose did not provide additional health benefits.”
Reference:
Maya Rahme, Laila Al-Shaar, Hani Tamim, Ghada El-Hajj Fuleihan, Blood Pressure Decreases in Overweight Elderly Individuals on Vitamin D: A Randomized Trial, Journal of the Endocrine Society, Volume 8, Issue 12, December 2024, bvae168, https://doi.org/10.1210/jendso/bvae168
Keywords:
Vitamin D, supplementation, lower BP, overweight, elderly, study, Journal of the Endocrine Society, Maya Rahme, Laila Al-Shaar, Hani Tamim, Ghada El-Hajj Fuleihan, Blood Pressure
Powered by WPeMatico