Late Gadolinium Enhancement Helps Predict Sudden Cardiac Death in Youth with Hypertrophic Cardiomyopathy: Study
A recent multicenter study has found that late gadolinium enhancement (LGE) on cardiovascular magnetic resonance (CMR) imaging can predict the risk of sudden cardiac death (SCD) in children and adolescents with hypertrophic cardiomyopathy (HCM). This can significantly improve risk stratification for younger patients and increases the ability to identify high-risk patients and potentially guide early interventions. The study results were published in the journal JAMA Cardiology.
Hypertrophic cardiomyopathy is a genetic heart condition and is one of the leading causes of sudden cardiac death in young people. It is marked by abnormal thickening of the heart muscle. Previous research shows that LGE has been associated with SCD events in adults with HCM, but its prognostic value in younger populations is uncertain. Hence, researchers conducted a study to examine the prognostic significance of LGE in patients with HCM who are younger than 21 years.
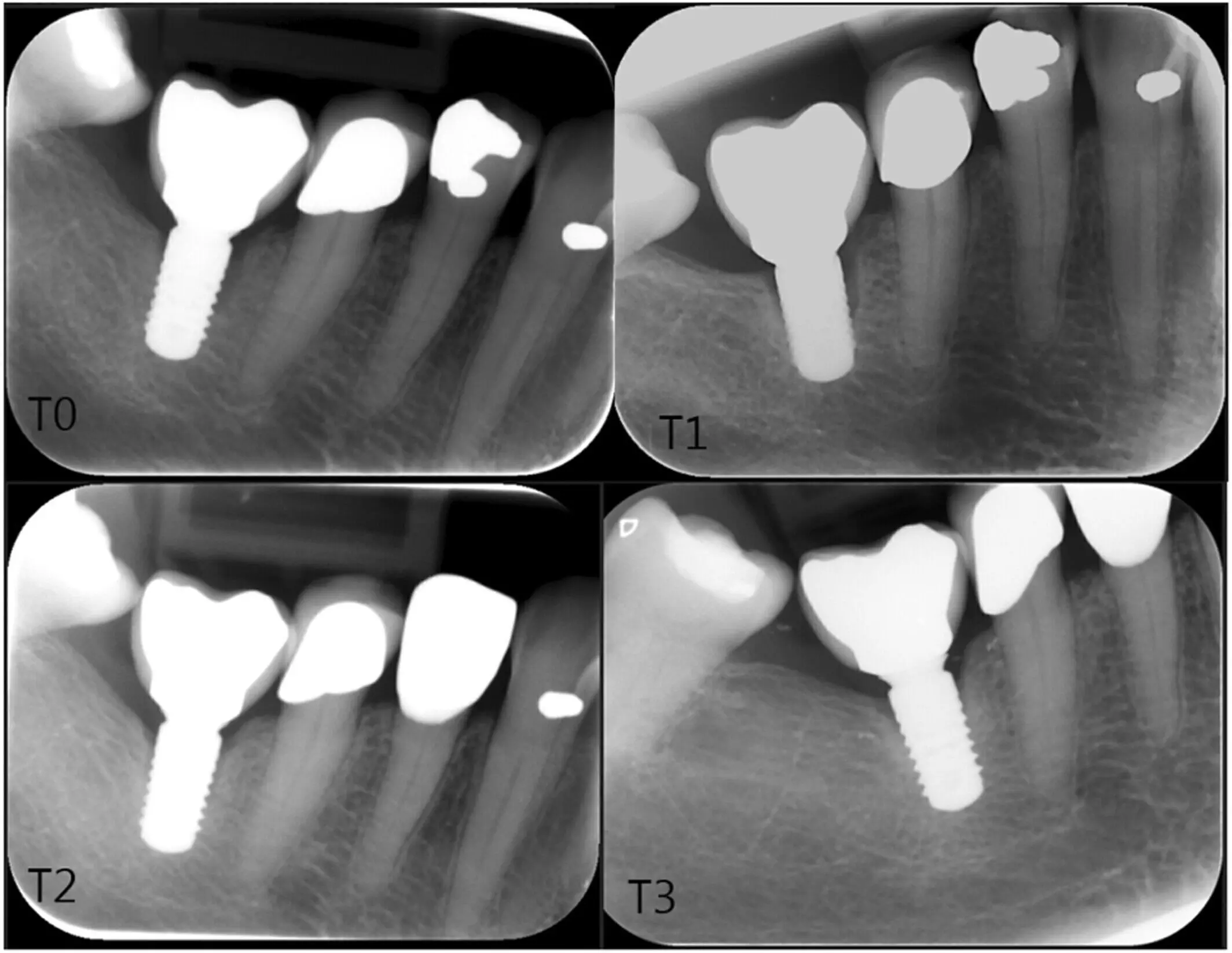
A multicenter, retrospective cohort study was conducted from April 2015 to September 2022 at 37 international sites in the US, Europe, and South America. The study included 700 patients less than 21 years of age diagnosed with HCM who underwent CMR imaging. The observers were masked from the outcomes and the demographic data for objective analysis. The primary outcome of measurement was to assess the prognostic significance of LGE in predicting SCD or equivalent events, such as resuscitated cardiac arrest or appropriate shocks from implantable defibrillators.
Key Findings
- The study’s findings are significant.
- During a follow-up period of 1.9 years, 35 individuals experienced SCD or other similar events.
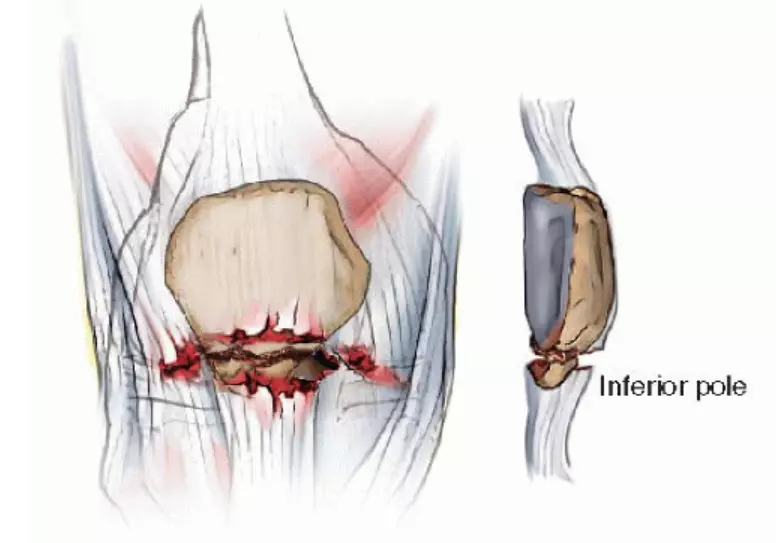
- Out of the 700 patients, 230 (32.9%) had evidence of LGE in the left ventricular myocardium, with an average burden of 5.9%.
- The presence and extent of LGE were more pronounced in older patients and those with greater left ventricular mass and wall thickness.
- Furthermore, patients with LGE showed signs of declining cardiac function, with lower left ventricular ejection fractions and larger left atrial diameters.
- The study demonstrated that patients with LGE had a higher likelihood of SCD, even when controlling for other existing risk factors.
- Notably, those with 10% or more LGE relative to total myocardium had more than double the risk of SCD (hazard ratio [HR] 2.19), suggesting a direct correlation between the extent of LGE and SCD risk.
- The addition of LGE burden to existing risk prediction models significantly improved their accuracy by improving the performance of the widely used HCM Risk-Kids score that increased from 0.66 to 0.73.
- The Precision Medicine in Cardiomyopathy score improved from 0.68 to 0.73 suggesting the importance of LGE as a valuable tool in refining current risk assessment methods for young HCM patients.
Thus, the study concluded that LGE is a critical marker for assessing SCD risk in children and adolescents with HCM. Quantitative LGE enhanced the predictive power of existing risk models and was a risk factor for SCD. This information could be pivotal in improving clinical management, leading to more personalized care for young HCM patients at high risk of sudden cardiac death.
Further reading: Chan RH, van der Wal L, Liberato G, et al. Myocardial Scarring and Sudden Cardiac Death in Young Patients With Hypertrophic Cardiomyopathy: A Multicenter Cohort Study. JAMA Cardiol. Published online September 25, 2024. doi:10.1001/jamacardio.2024.2824
Powered by WPeMatico