Lupin Announces Positive Results from Global Phase 3 Trial of Lucentis Biosimilar
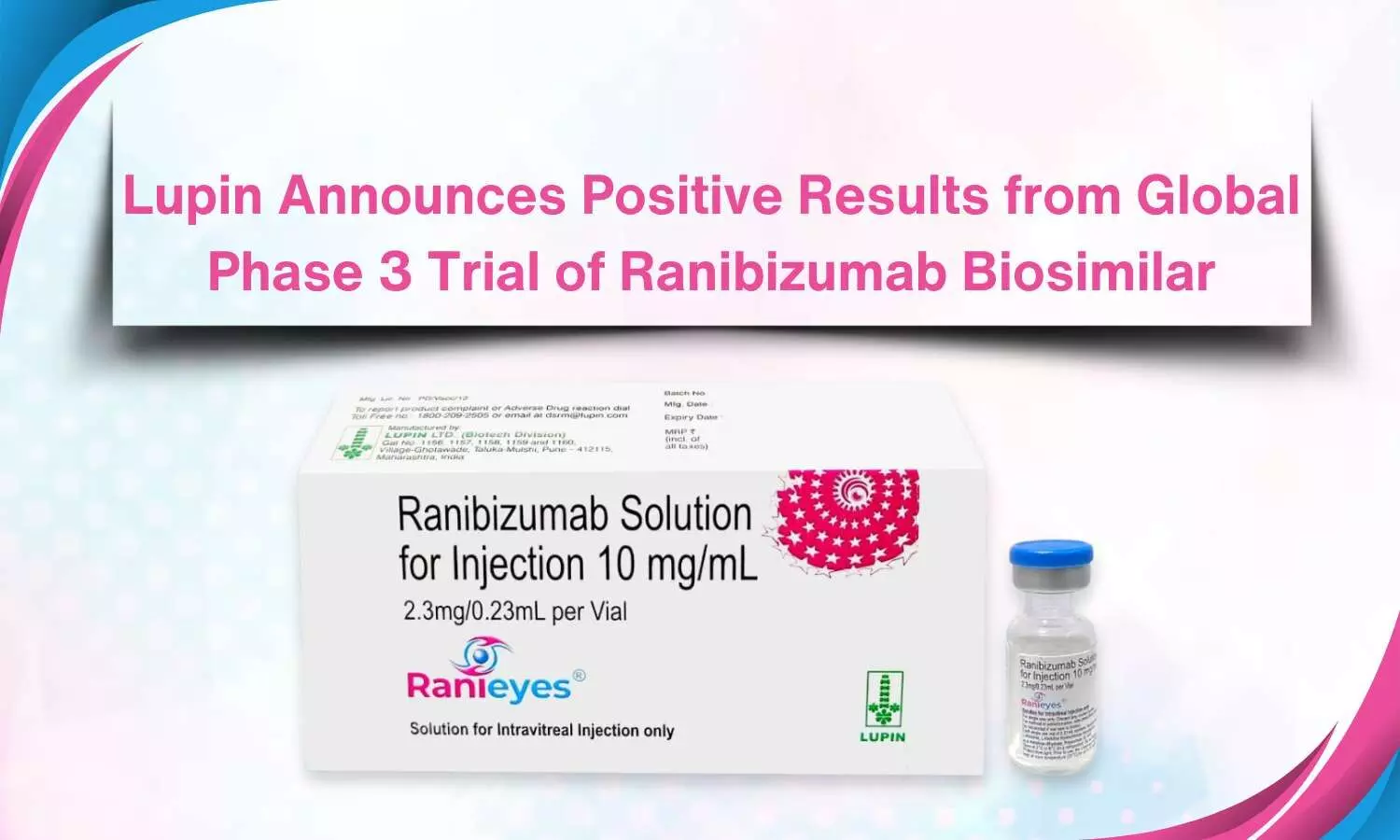
Lupin recently announced positive results from global phase 3 clinical trials evaluating the immunogenicity, safety, and efficacy of LUBT010—Lupin’s biosimilar for Luncentis versus Lucentis (0.5 mg ranibizumab) in patients with neovascular age-related macular degeneration.
Results from the 12-month-long global phase 3 trial demonstrated that it achieved the primary endpoint of therapeutic equivalence in visual acuity improvement for wet age-related macular degeneration patients, showcasing comparable safety and immunogenicity between LUBT010 and Lucentis. The trial enrolled about 600 patients from India, the US, the European Union and Russia who were randomised to receive either Lupin’s candidate LUBT010 or Lucentis 0.5 mg, as an injection once a month. Patients were followed for efficacy, safety and immunogenicity assessment. The data from this study would be part of Lupin’s application for marketing approval with the US Food and Drug Administration and the European Medicines Agency (EMA).
Approximately 600 patients from Russia, the US, India, and the European Union were included in the trial and randomly assigned to receive injections of either Lucentis 0.5 mg or Lupin’s biosimilar, LUBT010, once a month. Patients were monitored for safety, effectiveness, and immunogenicity evaluation. The 12-month phase 3 trial’s results showed that LUBT010 and Lucentis were similarly safe and immunogenic, and they also met the primary endpoint of therapeutic equivalency in terms of improving visual acuity for patients with wet age-related macular degeneration.
The findings from this study will be included in Lupin’s application to the US Food and Drug Administration and the European Medicines Agency (EMA) for marketing clearance. In addition, Lupin stated that the global phase 3 trial complied with the US Food and Drug Administration’s and the European Medicines Agency’s recommendations to compare the immunogenicity, safety, and effectiveness of LUBT010 with Lucentis in patients with neovascular age-related macular degeneration.
The global Phase 3 study marks another significant developmental milestone for Lupin’s Lucentis biosimilar, said Cyrus Karkaria, President, of Lupin Biotech. “We will be filing marketing applications for LUBT010 in all major global markets this year,” he added.
“This achievement of our biosimilars team demonstrates our capability to develop cutting-edge, cost-effective products. We have already commercialised four products to date and there are several more at various stages of clinical trials. We now look forward to bringing our high-quality Ranibizumab biosimilar into the global ophthalmic market, making a positive difference in the lives of our patients”, said Nilesh Gupta, Lupin’s Managing Director.
Since 2022, Lupin has been selling the biosimilar of ranibizumab in India under the name RaniEyes. Ranibizumab is a recombinant humanized IgG1 kappa isotype monoclonal antibody fragment used in the treatment of neovascular age-related macular degeneration, macular edema following retinal vein occlusion (RVO), diabetic macular edema (DME), diabetic retinopathy (DR) and myopic choroidal neovascularization (mCNV).
Powered by WPeMatico