Study Reveals Radiotherapy Benefits Persist for a Decade in Breast Cancer Patients

Powered by WPeMatico

Powered by WPeMatico

A new global analysis of the dietary habits of children and adolescents from 185 countries revealed that youth, on average, consumed nearly 23% more sugar-sweetened beverages in 2018 compared to 1990.
Overall, intakes were similar in boys and girls, but higher in teens, urban residents, and children of parents with lower levels of education. Researchers from the Friedman School of Nutrition Science and Policy at Tufts University published the findings Aug. 7 in The BMJ.
The study drew from the Global Dietary Database, a large comprehensive compilation of what people around the world eat or drink, to generate the first global estimates and trends of sugar-sweetened beverage intake in youth.
These were defined as soda, juice drinks, energy drinks, sports drinks, and home-sweetened fruit drinks such as aguas frescas with added sugars and containing more than 50 kcal per 1 cup serving. Incorporating data from over 1,200 surveys from 1990 through 2018 in a large model, the research team found that youth (defined as those ages 3 to 19 years) were drinking more and had nearly twice the overall intake of adults.
The research team’s definition of sugary drinks excluded 100% fruit juices, non-caloric artificially sweetened drinks, and sweetened milks.
Sugar-sweetened beverage intake among young people varied dramatically by world region, averaging 3.6 servings per week globally and ranging from 1.3 servings per week in South Asia to 9.1 in Latin America and the Caribbean. The researchers found that children and teens in 56 countries, representing 238 million young people or 10% of the global youth population, averaged 7 or more servings per week.
“Sugary beverages increase weight gain and risk of obesity, so even though kids don’t often develop diabetes or cardiovascular disease when they are young, there could be significant impacts later in life,” said first author Laura Lara-Castor, a recent graduate of the Friedman School and now a postdoctoral scholar at the University of Washington. “This study highlights the need for targeted education and policy interventions to change behavior early on and prevent the adverse outcomes associated with sugar-sweetened beverage intake in childhood.”
Among the world’s most populous nations, those with the highest sugary drink intakes by youth in 2018 included Mexico (10.1 servings per week), followed by Uganda (6.9), Pakistan (6.4), South Africa (6.2), and the United States (6.2). Looking at trends from 1990 to 2018, the region with the largest increase in consumption among youth was Sub-Saharan Africa, in which average weekly servings grew 106% to 2.17 servings per week, an acceleration that requires attention, say the researchers.
In recent years, many governments worldwide have been implementing measures such as soda taxes and restrictions on the sale of sugary drinks in schools to promote healthy dietary habits. These efforts are new and also face strong opposing forces such as aggressive industry marketing and the globalization of the food sector.
“Our findings should raise alarm bells in nearly every nation worldwide,” said senior author Dariush Mozaffarian, Jean Mayer Professor of Nutrition and director of the Food is Medicine Institute at the Friedman School. “The intakes and trends we’re seeing pose a significant threat to public health, one we can and must address for the future of a healthier population.”
Research reported in this article was supported by the Gates Foundation, the American Heart Association, and the National Council for Science and Technology in Mexico. Complete information on authors, methodology, limitations, and conflicts of interest is available in the published paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Powered by WPeMatico

There is growing concern regarding infertility and human
semen quality because 8–12% of couples of reproductive age, around the world,
have difficulties conceiving. It is estimated that male factors account for up
to 40–50% of this infertility burden. The remarkable decrease in semen quality
over the last decades, particularly in developed and industrialized countries,
highlights the potential roles of environmental and lifestyle factors in this
decline. Environmental pollution, illicit drug use, smoking, alcohol
consumption, dietary exposure to potential endocrine-disrupting chemicals,
psychological stress, and unhealthy diets have been hypothesized to be involved
in the etiology of poor semen quality. Given their modifiable nature,
decreasing exposure to these could be appropriate in infertility prevention.
Among lifestyle risk factors, dietary habits appear to have an important role
in semen quality.
Previous research has reported that adherence to healthy
dietary patterns rich in unprocessed or minimally processed food (fruits,
vegetables, legumes, or nuts) and low in red and processed meat or
sugar-sweetened beverages, such as the Mediterranean or Prudent diet is
positively associated with semen quality. In contrast, the Western diet, rich
in meat and processed meat, dairy products, and sugar-sweetened beverages, has
a high glycaemic index and seems to be negatively associated with different
semen quality parameters. Unfortunately, the Western dietary pattern, which is
associated with a higher consumption of ultra-processed food (UPF), has been
rising during recent decades. UPFs are industrial formulations typically of
poor nutritional quality and containing several added ingredients including
sugar, salt, fat, artificial colors, flavors and stabilizers, among other
additives. Thus, they are ready-to-eat, low-cost, hyper-palatable, convenience
products with a long shelf life. Additionally, most of them are low in
health-beneficial dietary components such as fiber, vitamins, minerals, and
phytochemicals. A significant body of scientific evidence has reported an
association between UPF consumption and several chronic diseases such as
obesity, diabetes, hypertension, cardiovascular disease (CVD), cancer, and
all-cause mortality.
Currently, UPFs constitute a significant and growing
component of the global food supply, playing a crucial role in the average
consumer’s diet. However, their impact on semen quality has been scarcely
studied.
A cross-sectional analysis was conducted using data from 200
healthy men (mean age 28.4 ± 5.5 years) enrolled in the Led-Fertyl (Lifestyle
and Environmental Determinants of Seminogram and Other Male Fertility-Related
Parameters) study between February 2021 and April 2023. UPF consumption (% of
energy from UPF) was estimated according to the NOVA classification system
using a validated 143-item semi-quantitative food frequency questionnaire.
Total sperm count, sperm concentration, sperm vitality, total motility,
progressive motility, and normal sperm forms were set as the main outcomes.
Microscopic parameters were analyzed using a phase-contrast microscope and a
computer-assisted sperm analysis (CASA) system. Semen samples were collected
and tested according to World Health Organization 2010 standards. Multivariable
linear regression models were fitted to estimate the associations between UPF
tertile and semen quality parameters.
Sperm concentration (95% CI: −2.72 to −0.12) and motility (CI:
−15.16 to −0.51) were lower in participants in the highest tertile of UPF
compared to the lowest. A similar association was observed for sperm count when
UPF was analyzed per 10% increment of energy from UPF consumption (95% CI:
−2.83 to −0.17). Theoretically replacing 10% of energy from UPF consumption
with 10% of energy from unprocessed or minimally processed food consumption was
associated with a higher total sperm count, sperm concentration, total
motility, progressive motility, and normal sperm forms.
This is the first study using the NOVA classification system
to examine the association between UPF consumption and several semen quality
parameters. The findings of this cross-sectional analysis conducted in young
healthy men suggest that higher consumption of UPF is associated with lower
total sperm count, concentration and total motility. Moreover, replacing 10% of
energy from UPF consumption with unprocessed or minimally processed food was
associated with increases in total sperm count, sperm concentration, total
motility, progressive motility, and normal sperm forms.
High dietary UPF consumption was inversely associated with
certain semen quality parameters, including total sperm count, sperm
concentration, and total motility, in a population of young and healthy men.
Additionally, study results suggest that unprocessed and minimally processed
food consumption instead of UPF could have a beneficial effect on semen quality
parameters. Although the observed results could help to update or even develop
preventive and interventional male infertility programs, further studies are
required to replicate our observations, extend them to other populations, and
examine the underlying biological mechanisms explaining the associations found,
specifically long-term and/or well-controlled clinical trials.
Source: Valle-Hita et al.; Human Reproduction Open, 2024,
2024(1), hoae001 https://doi.org/10.1093/hropen/hoae001
Powered by WPeMatico
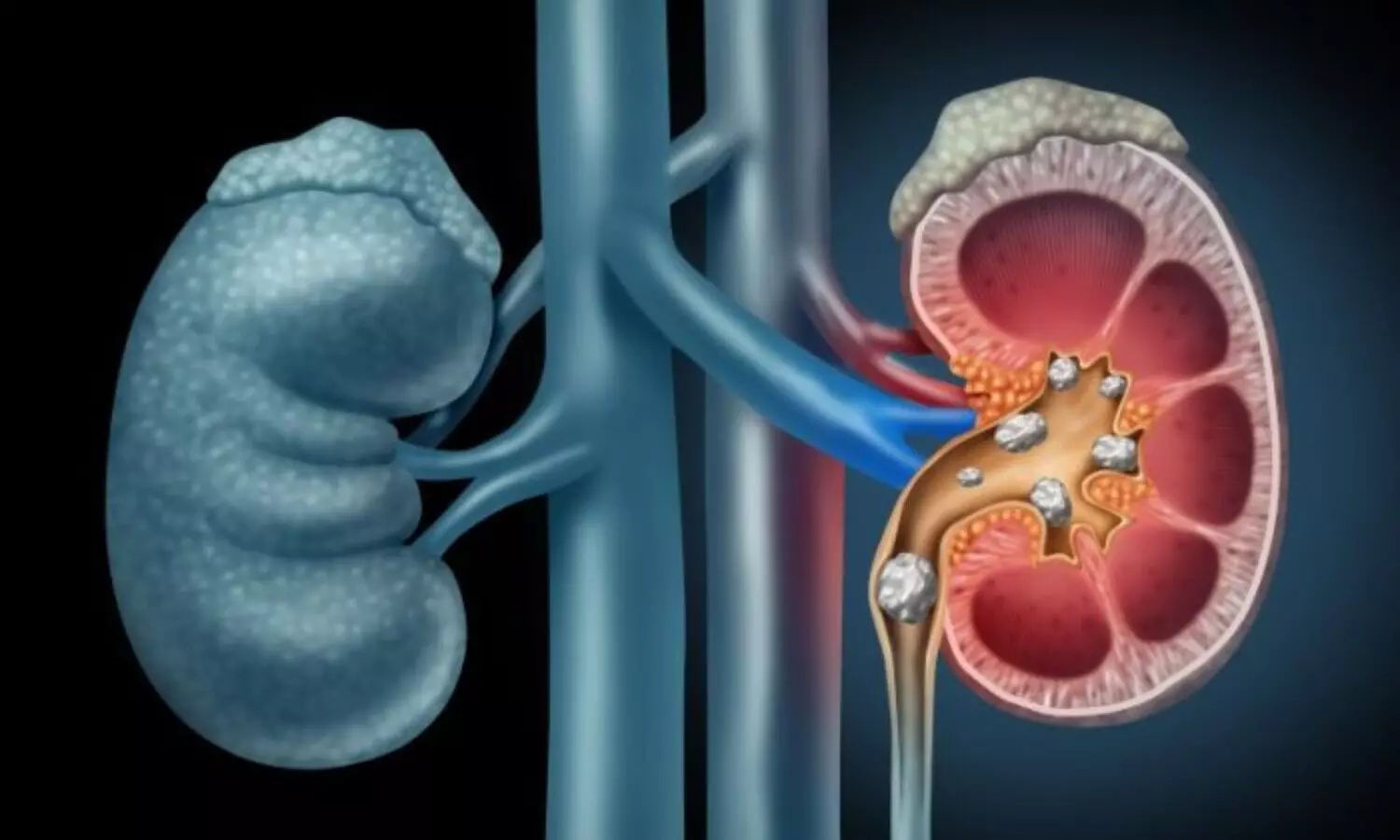
A novel artificial intelligence (AI) system was created by Jin kim and team to identify kidney stones in CT (computed tomography) scans with speed and accuracy, the findings of this work were published in the recent issue of European Urology Focus journal.
A prominent cause of acute renal colic is urolithiasis which has been more widespread in the recent years. The frequency of emergency department (ER) visits for renal colic caused by urolithiasis is correlated with this growing trend. It is crucial to diagnose urolithiasis as soon as possible to avoid major side effects including urosepsis and hydronephrotic kidney damage.
This study aimed to create an artificial intelligence system that would use sophisticated deep learning to detect urolithiasis in computed tomography pictures. This system would be able to calculate the properties of the stone like volume and density in real time, which is crucial for making treatment decisions. In ER circumstances, the system’s performance was compared to that of urologists.
The data set included axial CT scans for patients who had urolithiasis surgery between August 2022 and July 2023. The data set was split into three categories as training (70%), internal validation (10%) and testing (20%). Labelimg for ground-truth data was used to annotate stones by two urologists and an AI specialist. The RTX 4900 graphics processing unit (GPU) acceleration was applied to the YOLOv4 architecture during training. 100 individuals with probable urolithiasis had their CT pictures examined for external validation.
Overall, the AI interpretation system employs a sophisticated deep-learning algorithm to detect urolithiasis in CT images and compute critical stone properties, this assists in the real-time determination of suitable care strategies.
Source:
Kim, J., Kwak, C. W., Uhmn, S., Lee, J., Yoo, S., Cho, M. C., Son, H., Jeong, H., & Choo, M. S. (2024). A Novel Deep Learning–based Artificial Intelligence System for Interpreting Urolithiasis in Computed Tomography. In European Urology Focus. Elsevier BV. https://doi.org/10.1016/j.euf.2024.07.003
Powered by WPeMatico

Cannabis-related disorder linked to the development of head and neck cancer in adult patients suggests a study published in the JAMA.
This cohort study highlights an association between cannabis-related disorder and the development of head and neck cancer in adult patients. Given the limitations of the database, future research should examine the mechanism of this association and analyze dose response with strong controls to further support evidence of cannabis use as a risk factor for head and neck cancers.
Cannabis is the most commonly used illicit substance worldwide. Whether cannabis use is associated with head and neck cancer (HNC) is unclear. This large multicenter cohort study used clinical records from a database that included 20 years of data (through April 2024) from 64 health care organizations. A database was searched for medical records for US adults with and without cannabis-related disorder who had recorded outpatient hospital clinic visits and no prior history of HNC. Propensity score matching was performed for demographic characteristics, alcohol-related disorders, and tobacco use. Subsequently, relative risks (RRs) were calculated to explore risk of HNC, including HNC subsites. This analysis was repeated among those younger than 60 years and 60 years or older. Results The cannabis-related disorder cohort included 116 076 individuals (51 646 women [44.5%]) with a mean (SD) age of 46.4 (16.8) years. The non–cannabis-related disorder cohort included 3 985 286 individuals (2 173 684 women [54.5%]) with a mean (SD) age of 60.8 (20.6) years. The rate of new HNC diagnosis in all sites was higher in the cannabis-related disorder cohort. After matching (n = 115 865 per group), patients with cannabis-related disorder had a higher risk of any HNC (RR, 3.49; 95% CI, 2.78-4.39) than those without HNC. A site-specific analysis yielded that those with cannabis-related disorder had a higher risk of oral (RR, 2.51; 95% CI, 1.81-3.47), oropharyngeal (RR, 4.90; 95% CI, 2.99-8.02), and laryngeal (RR, 8.39; 95% CI, 4.72-14.90) cancer. Results were consistent when stratifying by older and younger age group. This cohort study highlights an association between cannabis-related disorder and the development of HNC in adult patients. Given the limitations of the database, future research should examine the mechanism of this association and analyze dose response with strong controls to further support evidence of cannabis use as a risk factor for HNCs.
Reference:
Gallagher TJ, Chung RS, Lin ME, Kim I, Kokot NC. Cannabis Use and Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg. Published online August 08, 2024. doi:10.1001/jamaoto.2024.2419
Keywords:
Cannabis-related, disorder, development, head, neck cancer, adult patients, JAMA, JAMA Otolaryngology–Head & Neck Surgery
Powered by WPeMatico

The U.S. Food and Drug Administration (FDA) has granted accelerated approval for the immunotherapy afamitresgene autoleuecel (Tecelra®, also known as afami-cel) for the treatment of adults with a rare soft tissue cancer called synovial sarcoma.
Afami-cel is the first engineered T cell therapy to receive FDA approval for a solid tumor cancer.
The clinical trial that resulted in the drug’s approval was led by Memorial Sloan Kettering Cancer Center (MSK) sarcoma specialist and immunotherapy expert Sandra D’Angelo, MD.
“This treatment offers an important new option for people with this rare cancer,” Dr. D’Angelo says. “It is also an important step forward in the development of T cell therapies for solid tumors, which has been a major challenge.”
Other cell therapies, such as chimeric antigen receptor (CAR) T cell therapy, involve targeting surface proteins to recognize and attack a cancer cell. Until now, these types of immunotherapies have been used only to treat blood cancers.
Synovial sarcoma is diagnosed in fewer than 1,000 people in the United States every year. A cancer that can develop in the extremities or in the soft tissue in the abdomen or lung, it most often occurs in young adults. It is slightly more common in men than in women.
“Sarcoma in general, and synovial sarcoma in particular, is a type of cancer where more treatments are desperately needed,” Dr. D’Angelo explains. “Once the disease spreads to other parts of the body, it is very difficult to control with the therapies we have now.”
Afami-cel is an engineered cell therapy, similar to the CAR T treatments that have been approved for treating certain blood cancers since 2017. With cell therapies, a patient’s own T cells are collected from the blood and engineered in a lab to recognize cancer cells. They are then infused back into the bloodstream, allowing them to travel throughout the body to detect and destroy tumor cells.
Engineered cell therapies are often called “living drugs,” and for many people with blood cancer, they have offered the hope of a cure.
Afami-cel is not a CAR T therapy but is in a related category called T cell receptor (TCR) therapy. The T cells are engineered to carry an extra tool that allows them to recognize proteins, or markers, that are hiding inside cancer cells. By contrast, CAR T therapies can only see these cancer markers when they are on the outside of tumor cells.
“With both CAR T and TCR therapies, you are giving the immune cells the ability to fight the cancer,” Dr. D’Angelo explains. The cancer-causing protein that afami-cel targets is called MAGE-A4.
Another therapy that uses patients’ own immune cells, known as TIL therapy, also recently received FDA approval for treating the solid tumor melanoma. TIL therapy requires that immune cells be extracted from tumors that are surgically removed and then expanded in the lab before being infused back into the patient.
The phase 2 clinical trial that resulted in the drug’s approval was published in The Lancet in April 2024. Dr. D’Angelo was lead author of the paper, which reported that afami-celsignificantly shrank sarcoma tumors in more than one-third of patients.
“Some patients in the trial had their tumors completely disappear and have not had the cancer come back for several years,” Dr. D’Angelo says.
The clinical trial was an international study that treated a total of 52 people who had been diagnosed with synovial sarcoma and myxoid/round cell liposarcoma (MRCLS), another type of soft tissue sarcoma. These patients had not responded to other therapies.
“These findings are significant for a group of patients who have largely exhausted other treatment options,” Dr. D’Angelo says.
Before receiving the cell therapy afami-cel, patients were first treated with chemotherapy. The most frequent side effect of that treatment was low blood counts.
About 71% of patients in the trial also experienced cytokine release syndrome (CRS) , a common reaction after cell therapies. This occurs when the immune system temporarily goes into overdrive to fight the cancer. For most patients in the afami-cel trial, this syndrome was not severe.
Dr. D’Angelo hopes that eventually afami-cel may work against any type of solid tumor that carries the mutated MAGE-A4 protein.
Afami-cel and other TCR therapies are also being studied in pediatric sarcomas.
Powered by WPeMatico

India: A study published in the Indian Journal of Gastroenterology revealed that utilizing a portable ultrasound machine and a dynamometer for bedside assessment of sarcopenia effectively identifies liver cirrhosis patients who are at a high risk of complications and mortality.
Sarcopenia is linked to numerous negative outcomes in cirrhosis patients. The current tools for assessing sarcopenia have various shortcomings. The researchers investigated the effectiveness of using portable ultrasonography and a dynamometer for bedside assessment of sarcopenia and its implications in hospitalized cirrhosis patients.
Sabbu Surya Prakash, Department of Gastroenterology, All India Institute of Medical Sciences et. al. conducted a study to evaluate the bedside assessment of sarcopenia in hospitalized patients with liver cirrhosis, focusing on its magnitude and clinical implications.
In this study, a dynamometer was utilized to assess hand-grip strength (HGS), while an ultrasound was employed to measure the thickness of the forearm and quadriceps muscles. According to the European Working Group on Sarcopenia in Older People (EWGSOP2) criteria, HGS values less than 27 kg for men and less than 16 kg for women were considered significant. The lower normal limit of muscle mass (5th percentile) was established based on measurements from 100 matched healthy controls.
The key findings of the research were as follows:
According to EWGSOP2 criteria and HGS values, 56% of 300 cirrhosis patients had sarcopenia, and 62.3% had probable sarcopenia.
HGS alone identified sarcopenia in 88.9% of patients but overestimated it in 6.3% of cases.
Sarcopenic patients had more cirrhosis complications, such as ascites, variceal bleeding, hepatic encephalopathy, spontaneous bacterial peritonitis, sepsis, hepatorenal syndrome, and refractory ascites, compared to those without sarcopenia.
In-hospital mortality, three-month mortality, and six-month mortality rates were all higher among sarcopenic patients.
Cox regression survival analysis showed that six-month mortality was significantly higher in sarcopenic patients than in those without sarcopenia.
The researchers concluded that bedside assessment of sarcopenia using a portable ultrasound machine and a dynamometer detects liver cirrhosis patients with a high risk of complications and mortality.
Reference:
Prakash, S.S., Priyadarshi, R.N., Surya, H. et al. Bedside assessment of sarcopenia in hospitalized patients with liver cirrhosis: Magnitude and clinical implications. Indian J Gastroenterol (2024). https://doi.org/10.1007/s12664-024-01642-x
Powered by WPeMatico
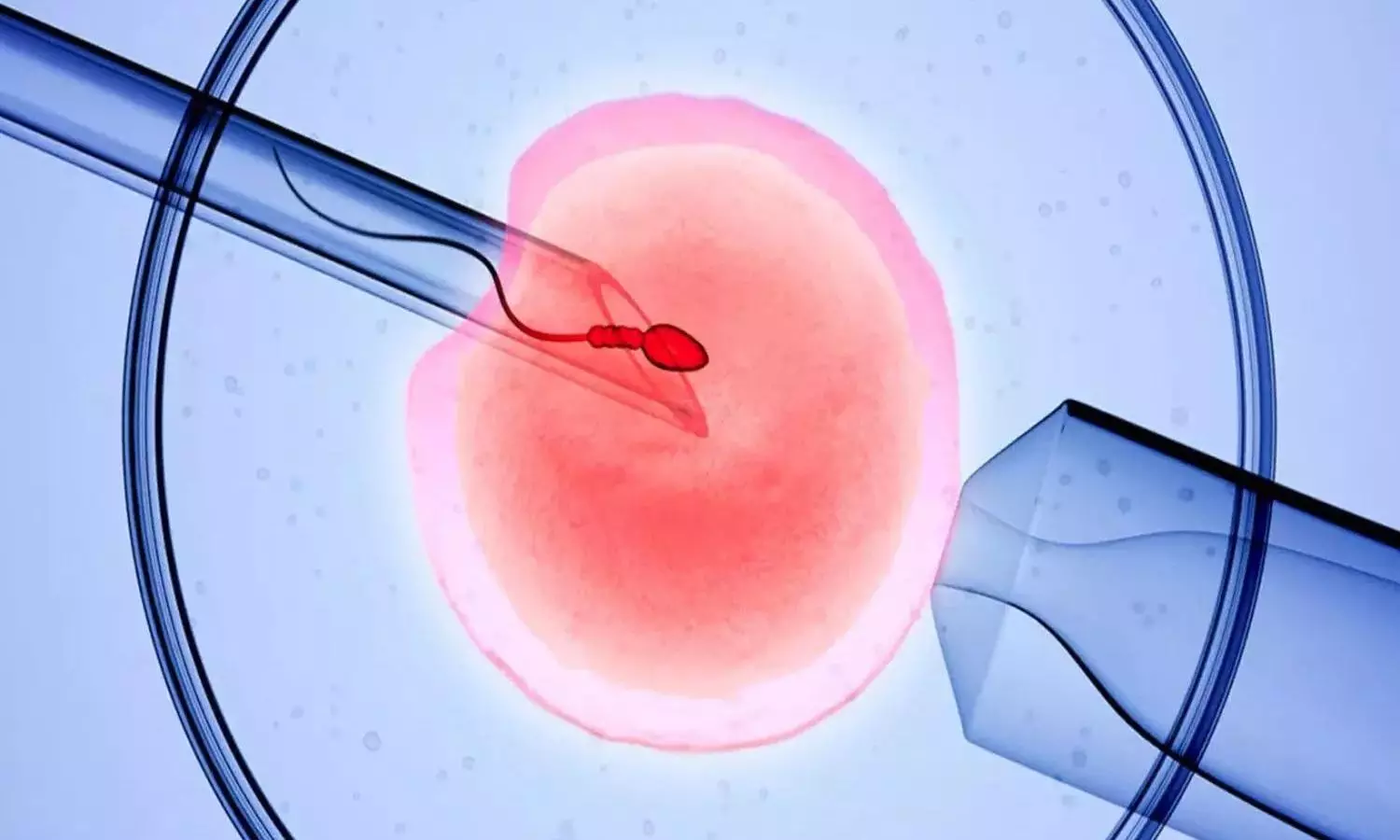
There is no difference in live birth rates between time-lapse imaging and other standard approaches used in in-vitro fertilisation (IVF) for embryo incubation and selection prior to implantation, according to the results of the largest trial of its kind.
The randomised controlled trial looked at IVF outcomes in the UK and Hong Kong. The results, published in The Lancet, provide much-needed evidence that using time-lapse imaging (TLI) does not improve treatment outcomes for someone undergoing fertility treatment.
Time-lapse imaging is a technique used in IVF that takes thousands of time-lapse images of embryos as they grow, creating a continuous view of each embryo as it develops. Some fertility practitioners offer TLI as a pre-implantation screening technique and believe that information that TLI provides – such as rate of development or the number and appearance of cells-can help to select the best embryos for implantation.
In TLI, the embryos are not removed from their incubators, thereby minimising the fluctuations in temperature, humidity, pH, and gas concentrations that might affect development. Standard techniques to assess and select the embryos with the best implantation potential require the embryo to be removed from incubators.
The double-blind trial, led by Dr Priya Bhide from the Women’s Health Research Unit at Queen Mary University of London and funded by Barts Charity and others, recruited over 1,500 participants undergoing IVF at seven centres in the United Kingdom and Hong Kong.
The participants were randomly assigned to one of three trial arms: one group of participants received TLI-based embryo selection, one group received the standard static assessment using undisturbed culture, and the third received conventional assessment using light microscope and standard embryo culture in standard incubators. Baseline demographic and clinical characteristics of participants were similar in the three arms.
Live birth rates for embryos from each arm of the study were 33.7% in the TLI arm, 36.6% in the undisturbed culture arm and 33.0% in the control arm. The clinical pregnancy rates were 42.2% in the TLI arm, 43.4% in the undisturbed culture arm, and 40.9% in the control arm. None of the other secondary outcomes for clinical effectiveness and safety demonstrated significant differences between the arms.
Dr Priya Bhide, Clinical Reader at the Women’s Health Research Unit, Centre for Public Health and Policy in the Wolfson Institute of Population Health, said: “Our trial suggests that TLI does not improve the odds of live birth in women having IVF and ICSI treatments. This shows that the theoretical benefits of advanced technology do not always translate into improved clinical outcomes. This is important information for all stakeholders; patients, healthcare professionals, funders and policymakers.”
Dr David Chan, lab director at the Prince of Wales Hospital, The Chinese University of Hong Kong, said: “Our trial provides evidence to support that TLI machines may not be essential equipment in the IVF lab, especially for IVF laboratories with limited resources. Laboratories may use the findings from this study to re-evaluate how they allocate their budget for equipment. Instead of investing heavily in the TLI machine, they could focus more on lab equipment that has a direct, measurable impact on live birth rates. This approach could help strike a better balance between the overall cost of IVF treatments and patient affordability in resource-limited settings”.
One in six adults are affected by subfertility worldwide. Statistics from the Human Fertilisation and Embryology Authority (HFEA) show over 100,000 IVF treatments took place in the UK during 2022-23.
Reference:
Priya Bhide, David Y L Chan, Doris Lanz, Odai Alqawasmeh, Eleanor Barry, Dominic Baxter, Clinical effectiveness and safety of time-lapse imaging systems for embryo incubation and selection in in-vitro fertilisation treatment (TILT): a multicentre, three-parallel-group, double-blind, randomised controlled trial, The Lancet, https://doi.org/10.1016/S0140-6736(24)00816-X.
Powered by WPeMatico

Switzerland: Chronic pruritus, or persistent itching, is a distressing condition that significantly impacts the quality of life for many individuals. A recent narrative review has shed light on the evolving role of device-based physical therapies in managing this challenging symptom. The review underscores how technological advancements are providing new avenues for effective treatment.
In the review, published in the Journal of the American Academy of Dermatology, Jie Zhu, Department of Dermatology, University Hospital Basel, Basel, Switzerland, and colleagues provided an overview of physical modalities and their role in itch management.
Chronic pruritus can be a standalone issue or a symptom of underlying conditions such as eczema, psoriasis, or chronic kidney disease. Traditional treatments have often focused on topical agents, antihistamines, and systemic medications. However, these approaches may not always provide sufficient relief or have undesirable side effects. This has led researchers to explore alternative strategies, including device-based physical therapies.
Chronic pruritus is a highly prevalent disease associated with high economic and psychosocial burdens. The researchers note that alongside pharmacological treatments, device-based physical therapies are also emerging as effective antipruritic options. Technologies such as phototherapy, laser treatments, electrical neurostimulation, acupuncture, cryotherapy, and cold atmospheric plasma are being explored as potential treatments. While some of these methods remain experimental, they are expanding the arsenal for managing chronic pruritus.
In the review, the research team discussed data regarding these physical therapy modalities for managing patients with chronic pruritus.
“The promising modalities include pulsed-dye laser, phototherapy, acupuncture, cryotherapy, electrical neurostimulation, cold atmospheric plasma, and counter stimuli treatments,” the team wrote.
In patients with difficult-to-treat conditions with chronic pruritus, clinicians should consider the use of physical therapy modalities as a part of a multimodal approach to itch, the review stated.
In conclusion, device-based physical therapies represent an exciting frontier in treating chronic pruritus. As technology continues to advance, these therapies could become integral components of personalized treatment plans, offering new hope for those struggling with persistent itching.
Reference:
Zhu J, Zhao X, Navarini AA, Mueller SM. Device-based physical therapies in chronic pruritus: A narrative review. J Am Acad Dermatol. 2024 Jun 29:S0190-9622(24)00975-7. doi: 10.1016/j.jaad.2024.06.045. Epub ahead of print. PMID: 38950710.
Powered by WPeMatico
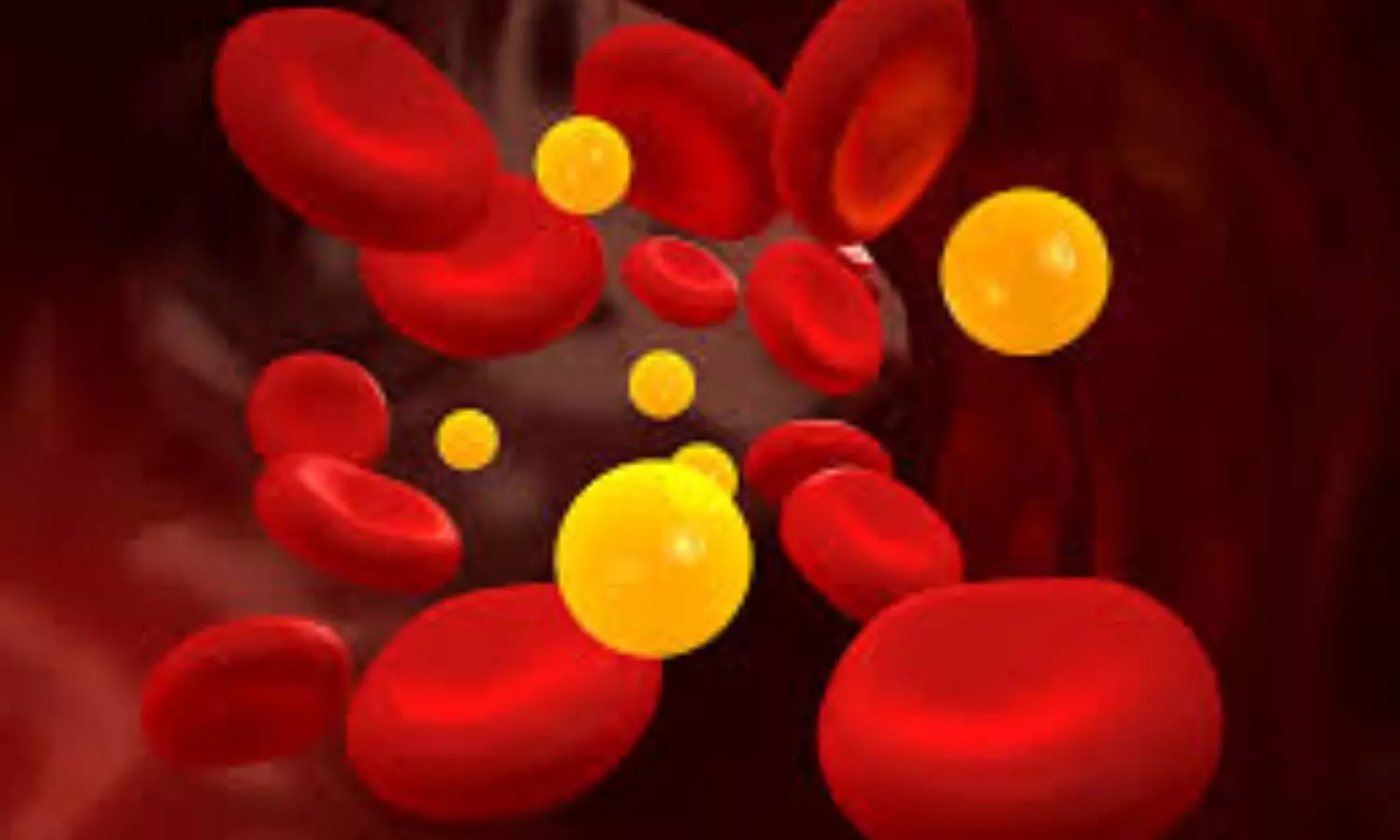
In a study, researchers found that elevated serum lipoprotein(a) (Lp(a)) was associated with an increased risk of atherosclerotic cardiovascular disease in Chinese maintenance hemodialysis patients. A study on this was published recently in BMC Nephrology by Qiaojing Liang and colleagues. The study at Beijing Tongren Hospital brings into light serum Lp(a) as a clinical biomarker for assessing atherosclerotic cardiovascular disease (ASCVD) risk in this population.
Serum Lp(a) is an established independent risk factor for ASCVD in the general population, but its role in ASCVD incidence among Chinese MHD patients was less clear. The present study aimed to clarify the relationship of Lp(a) levels with ASCVD events in a cohort of MHD patients from Beijing, China.
This was a retrospective observational cohort study of MHD patients treated in Beijing Tongren Hospital between January 1, 2013, and December 1, 2020, with follow-up until December 1, 2023. Primary outcome: the occurrence of ASCVD events. We used Kaplan-Meier survival analysis to evaluate ASCVD-free survival rates according to Lp(a) level strata. Cox regression analyses assessed the relationship of Lp(a) level with ASCVD incidence.
Results
There were a total of 265 patients, and the median follow-up period was 71 months.
There were 78 (29.4%) ASCVD events and 118 (47%) deaths; 58 (49.1%) were attributed due to ASCVD.
Spearman rank correlation tests have found correlations positively for serum Lp(a) and LDL-c levels whereas negative ones with hemoglobin, triglyceride, serum iron, serum creatinine, and albumin levels.
Conclusion: Using the multivariate Cox regression analysis, it was evidenced that Lp(a) level ≥30 mg/L, advanced age, low serum albumin, and diabetes mellitus were significantly associated with increased incidence of ASCVD.
In this regard, the results from the current study support the need for stratification of MHD patients using the measurement of serum Lp(a). The close relationship between high levels of Lp(a) and increased incidence of ASCVD suggests that, in fact, Lp(a) may stand as a good early marker for the identification of at-risk individuals. This becomes rather more important in the case of MHD, where cardiovascular complications are among the leading causes of death in such patients.
Practical clinical implications of the findings The regular monitoring of serum Lp(a) could provide risk stratification and early intervention, hence improving outcomes in MHD patients. In view of already high mortality related to ASCVD in this population, adding screening for Lp(a) in routine practice can become an important addition to the algorithm of cardiovascular risk management.
This is, therefore, a positive evidence study associating elevated serum Lp(a) levels with an increased risk of ASCVD in MHD patients. The results gave an indication that serum Lp(a) levels could be useful clinical indicators in estimating ASCVD risk and thus require monitoring with early interventions in this vulnerable population.
Reference:
Liang, Q., Zhang, G., & Jiang, L. (2024). Association between lipoprotein (a) and risk of atherosclerotic cardiovascular disease events among maintenance hemodialysis patients in Beijing, China: a single-center, retrospective study. BMC Nephrology, 25(1). https://doi.org/10.1186/s12882-024-03690-z
Powered by WPeMatico
