The US Food and Drug Administration (FDA) has approved oral selective inhibitor of Janus Kinases (JAK) JAK1 and JAK2 deuruxolitinib (Lesqselvi) 8 mg for adult patients with severe alopecia areata.
Deuruxolitinib in twice daily dose functions by disrupting these pathways which are suggested to contribute to severe alopecia areata patients’ loss of hair.
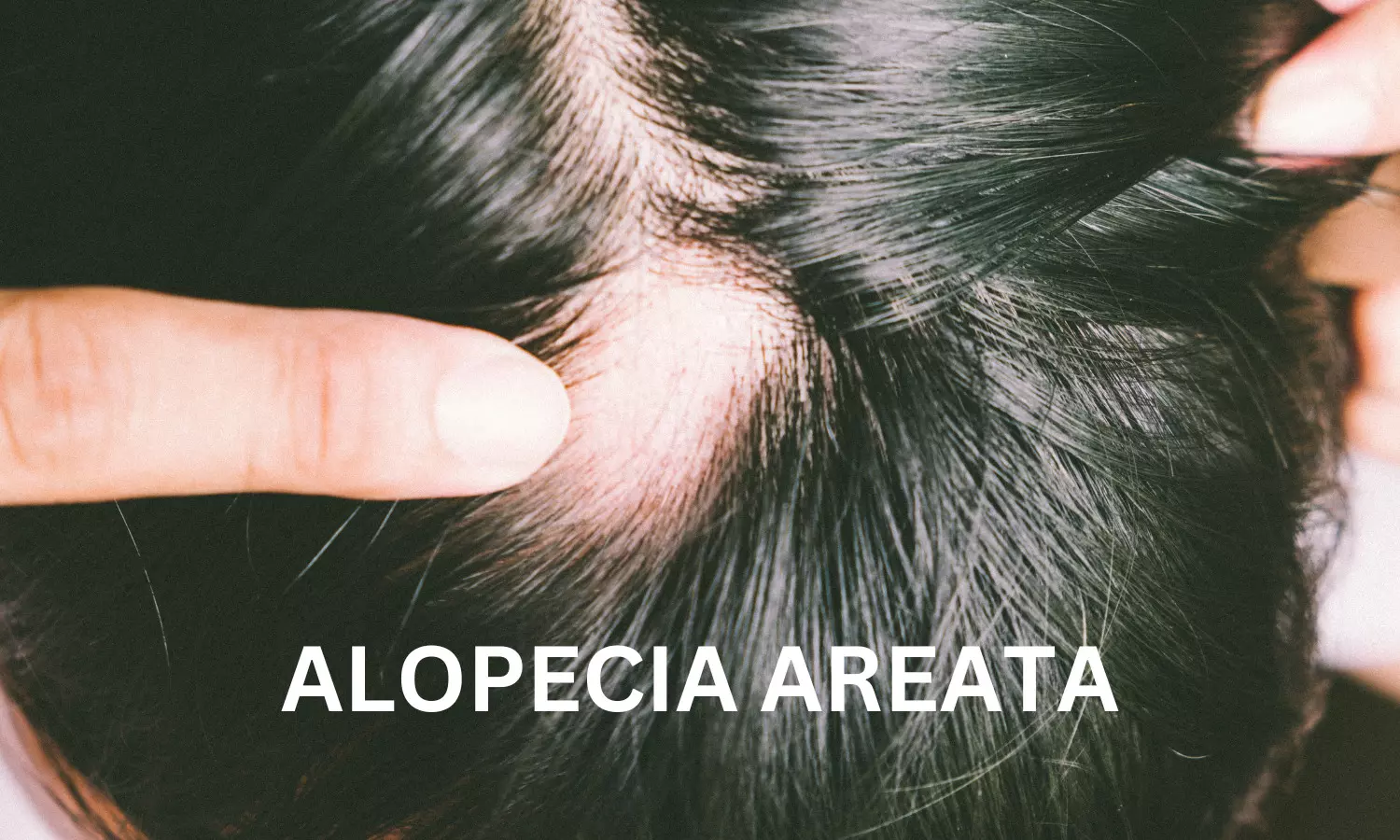
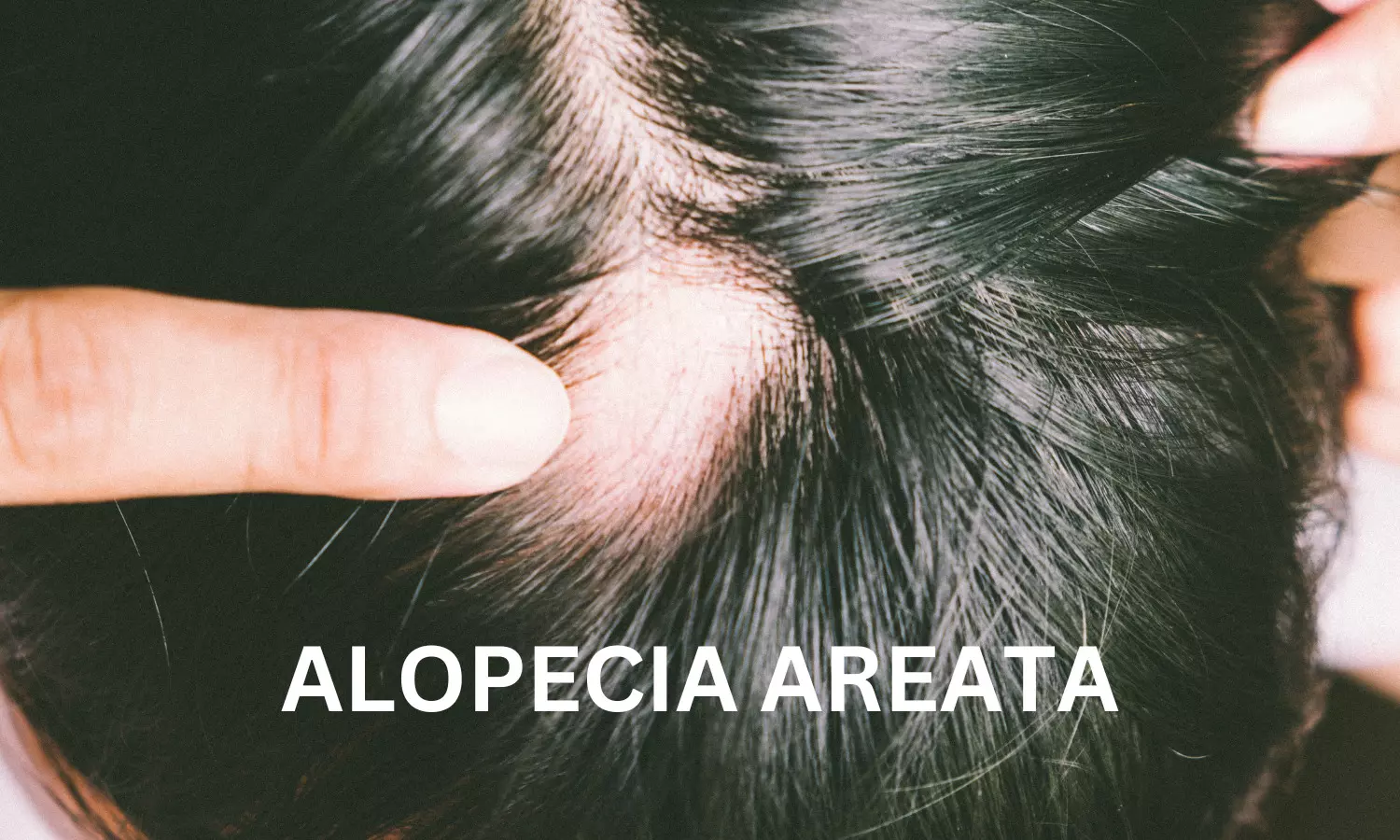
Alopecia areata affects around 700,000 people in the United States, and 300,000 have severe alopecia areata. Alopecia often leads patients to self-treat before seeking professional help, driven by dissatisfaction with the slow progress of existing treatments.
“LEQSELVI offers a new and effective solution that will significantly enhance options for long-suffering patients battling severe alopecia areata and their physicians,” said Abhay Gandhi, CEO, North America Business, Sun Pharma. “Our fast-growing dermatology business is excited to add this novel treatment to its portfolio.”
Alopecia areata is a common autoimmune disease in which hair loss is thought to occur due to the collapse of immune privilege, leading to the immune system targeting the hair follicles and causing sudden hair loss on the scalp, face and sometimes other areas of the body. LEQSELVI is a new, twice-daily oral selective inhibitor of Janus Kinases (JAK) JAK1 and JAK2. As a JAK inhibitor, LEQSELVI interrupts the pathways thought to contribute to hair loss in severe alopecia areata.
“We welcome the approval of LEQSELVI as a significant step for the alopecia areata community,” said Nicole Friedland, President and CEO, National Alopecia Areata Foundation (NAAF). “Alopecia areata is an autoimmune disease, with significant physical, emotional and financial impacts that go beyond hair loss. Today’s announcement empowers the alopecia community with even more choices, to which NAAF is committed, and provides another important option for those living with severe alopecia areata.”
The approval is based on data from two multicenter, randomized, double-blind, placebo-controlled Phase 3 clinical trials THRIVE-AA1 and THRIVE-AA2, which enrolled a total of 1,220 patients with alopecia areata who had at least 50% scalp hair loss as measured by Severity of Alopecia Tool (SALT) for more than six months. Data were also collected from two open-label, long-term extension trials in which patients were eligible to enroll upon completion of the 24-week trials.
At study baseline, the average patient had only 13% of their scalp hair coverage. In the trials, at 24 weeks, the primary endpoint was met, with more than 30% of patients taking LEQSELVI experiencing 80% or more scalp hair coverage (SALT ≤20).1 The number of patients taking LEQSELVI and achieving a SALT score of ≤20 showed a consistent upward trend with no plateau through 24 weeks.1 Additionally, up to 25% of patients had almost all of their scalp hair back at 24 weeks (≥90% coverage).
“For many people with severe alopecia areata, early intervention with effective treatment is critical,” said Natasha Mesinkovska, MD, PhD, Associate Professor and Vice Chair for Clinical Research of Dermatology, University of California, Irvine, and investigator in the LEQSELVI clinical development program. “An oral JAK that delivers proven results will be impactful for the alopecia areata community.”
Across the Phase 2 dose-ranging study and Phase 3 randomized, placebo-controlled trials, few patients (3.1%) receiving LEQSELVI 8 mg twice daily were discontinued from the trials due to adverse reactions.1 In clinical trials, more than 100 people continued taking deuruxolitinib for more than three years.
LEQSELVI may cause serious side effects including serious infections, malignancies, thrombosis, gastrointestinal perforations, and certain laboratory abnormalities. There also may be an increased risk of mortality and major cardiovascular events. LEQSELVI should not be used in patients who are CYP2C9 poor metabolizers or who are taking moderate or strong CYP2C9 inhibitors. In placebo-controlled trials, the three most common adverse events were headache (12.4% as compared to 9.4% with placebo), acne (10% as compared to 4.3% with placebo), and nasopharyngitis (8.1% as compared to 6.7% with placebo). Please see full Prescribing Information Including BOXED WARNING and Medication Guide and see below for Important Safety Information.
“We are pleased with the timely approval of LEQSELVI by the U.S. FDA,” said Marek Honczarenko, MD, PhD, Senior Vice President, Head of Development, Sun Pharma. “This validates our team’s capability to effectively bring treatments from research and development to approval in a way that is meaningful for physicians and patients. I want to thank all the investigators and patients for their participation in the clinical trials.”
Sun Pharma is committed to delivering support to the alopecia areata community and will introduce an access program to help eligible patients get started and stay on track with their treatment.
About LEQSELVI™ and alopecia areata
LEQSELVI (deuruxolitinib) 8 mg tablets is an oral selective inhibitor of Janus kinases JAK1 and JAK2 approved for the treatment of adult patients with severe alopecia areata. Alopecia areata is an autoimmune disease in which the immune system attacks hair follicles, resulting in partial or complete loss of hair on the scalp and body. Alopecia areata may affect up to 2.5% of the United States and global population during their lifetime.3,6,7 The scalp is the most commonly affected area, but any hair-bearing site can be affected alone or together with the scalp. Onset of the disease can occur throughout life and affects both women and men. Alopecia areata can be associated with serious psychological consequences, including anxiety and depression. There are currently limited approved treatment options available for alopecia areata.
About THRIVE-AA1 and THRIVE-AA2 trial design
THRIVE-AA1 and THRIVE-AA2 (NCT04518995 and NCT04797650) were randomized, double-blind, placebo-controlled clinical trials in 1223 adult patients ages 18-65 with severe alopecia areata at sites in the U.S., Canada and Europe evaluating the regrowth of scalp hair after 24 weeks of dosing using the SALT score. Patients were randomized to receive either 8 mg twice daily or 12 mg twice daily of deuruxolitinib or placebo for 24 weeks. The primary endpoint was the percentage of patients achieving a SALT score of 20 or less at 24 weeks. Patients enrolled in THRIVE-AA1 and THRIVE-AA2 were required to have at least 50 percent scalp hair loss due to alopecia areata, as measured by SALT. A SALT score of 100 represents total scalp hair loss, whereas a score of 0 represents no scalp hair loss. The average baseline SALT score across all patients in THRIVE-AA1 and THRIVE-AA2 was approximately 85.9 and 87.9 respectively.