Proteomic signatures may indicate MRI-assessed liver fat
Powered by WPeMatico
Powered by WPeMatico

New Delhi: A fire broke out at a Eye Mantra hospital in west Delhi’s Paschim Vihar area on Tuesday. Six fire tenders were rushed to the spot and the blaze was brought under control, officials said.
No one was injured in the incident as people were safely evacuated from the building, they said.
According to a PTI report, A call was received regarding the incident at 11.35 am. The fire broke out at the second floor of Eye Mantra Hospital, a Delhi Fire Services official said.
Also Read:7 Newborns dead, 5 Injured: What Went Wrong in Delhi’s Neonatal Hospital that Caught Fire?
Six fire tenders were pressed into service and the blaze was doused by 12.30 pm, the official said, adding that the cooling operation is underway.
According to the official, the fire was in a split air conditioner’s wall fixtures and a lasik laser machine. Local police has been informed about the matter for further probe, the official said.
The fire at Eye Mantra Hospital occurred just days after a massive blaze at a hospital in Vivek Vihar resulted in the tragic deaths of six newborns. As per media reports, the hospital authorities did not possess a No-Objection certificate (NOC) from the fire department.
Powered by WPeMatico

Pune: Following the tragic fire incident at a baby care centre in Delhi’s Vivek Vihar where seven newborns lost their lives, the joint director of health services has issued guidelines asking all health officials across the state to adopt proactive measures to avoid the recurrence of such incidents.
In a letter issued by Dr Sunita Golhait, the joint director of health services (Hospitals) has asked all health officers of Municipal corporations, district health officers, civil surgeons, and deputy directors across the state to conduct thorough inspections of all hospitals. These inspections aim to address any electrical capacity issues, verify the existence of valid fire NOCs, and enforce necessary safety protocols to prevent potential hospital fires.
“All the healthcare facilities have been instructed to conduct thorough inspections of all private and government hospitals in their jurisdiction. The officials are directed to address any discrepancies in electrical load capacity, ensure that hospitals have valid fire NOCs from respective fire departments, and implement critical safety measures. Besides, the officials are asked to submit a report on their findings,” reads the letter.
Also read- 7 Newborns Dead, 5 Injured: What Went Wrong In Delhi’s Neonatal Hospital That Caught Fire?
“Conduct comprehensive fire safety audits and on-site inspections of all hospitals to assess fire safety compliance. Ensure that fire-fighting systems, including fire alarms, fire smoke detectors, fire extinguishers, fire hydrants, and fire lifts, are present, fully functional and maintained,” added the letter.
The letter further stated, “Electrical equipment is used in important departments like SNCU, ICU Surgery and Dialysis unit. To avoid threats, ensure electrical load audits and calibration of electrical loads in all departments. Make sure that multiple high-power devices are not connected to a single circuit. Hospitals store a lot of inflammable materials like various chemicals, gas cylinders, heat-dissipating surgical instruments, etc.”
Medical Dialogues team had earlier reported that seven newborns died and five got injured after a baby care centre in Delhi’s Vivek Vihar caught fire. It was revealed that the hospital authorities did not possess a No-Objection Certificate (NOC) from the Fire Department and the hospital was operating despite the expiry of its license. Also, it had no qualified doctors.
According to officials as reported by HT, fire safety assessments of hospitals are essential because most fire accidents are caused by short circuits, overheating, overloading, poor-quality electrical equipment, improper wiring, lack of proper earthing, and increased electrical load from air conditioning systems and other equipment.
The hospitals have received instructions to enforce strict regulations against smoking in areas where hospital oxygen tanks and piped oxygen are present. These designated areas must be identified with appropriate signage, and employees working in these areas should undergo training to understand the potential hazards associated with high levels of oxygen.
Additionally, the department has recommended that hospital staff receive training on fire safety protocols, evacuation procedures for patients, staff, and visitors in the event of unexpected incidents such as fires, and the proper utilization of firefighting equipment.
There are a total of 899 private hospitals and nursing homes registered under the Maharashtra Nursing Home Registration Act 1949 that fall under the jurisdiction of the PMC. At the same time, the Pimpri Chinchwad Municipal Corporation (PCMC) has 617 private hospitals and 1,456 clinics registered with the civic body. However, fire safety is neglected in many clinics and small and medium-sized hospitals.
Similarly, Dr Kalpana Baliwant, deputy health officer of PMC told The Daily, “Fire and electrical audits are mandatory for private hospitals seeking new registration or renewal under the Bombay Nursing Home Act. While most private hospitals and all PMC-run hospitals have valid fire NOCs and electrical audits, we will instruct ward medical officers to conduct thorough inspections to ensure compliance with fire safety and electrical standards. Ward medical officers regularly carry out inspections for fire safety compliance.”
Powered by WPeMatico

A study of adults aged 60 years and older found that the use of statin therapy as primary cardiovascular disease (CVD) prevention was effective for preventing CVD and all-cause mortality, even in adults aged 85 years and older. The study is published in Annals of Internal Medicine.
Researchers from the University of Hong Kong used a target trial emulation design to investigate the relationship between statin therapy and CVD risk using electronic health records (EHRs) from the Hong Kong Hospital Authority. Thes study included adult patients over 60 without preexisting diagnosed CVDs who met indications for statin treatment from January 2008 to December 2015. Patients with prior statin use, lipid-lowering drug use, cancer, myopathies, or liver dysfunction were excluded.
Statin therapy was defined as specific statin drugs, and outcomes included major CVDs, all-cause mortality, and adverse events. Follow-up was conducted until outcomes, death, loss to follow-up, or the end of the study. The data showed that in all age groups, initiating statin therapy was associated with lower incidence of CVD and all-cause mortality, even among the older population aged 85 years or older. In addition, statin use did not increase the risk for adverse events, such as myopathies and liver dysfunction.
Reference:
Ingigerdur Sverrisdottir, Sigrun Thorsteinsdottir, Sæmundur Rognvaldsson, Thor Aspelund, Brynjar Vidarsson, Pall Torfi Onundarson, Bjarni A. Agnarsson, Association Between Autoimmune Diseases and Monoclonal Gammopathy of Undetermined Significance: An Analysis From a Population-Based Screening Study, Annals of Internal Medicine, https://doi.org/10.7326/M23-2867.
Powered by WPeMatico

Japan: A groundbreaking post hoc analysis of the BRIGHTEN study has shed light on the intricate relationship between proteinuria and rapid kidney function decline in chronic kidney disease (CKD). The findings, published in Diabetes Research and Clinical Practice, challenge conventional wisdom by highlighting the nuanced impact of proteinuria based on the underlying cause of CKD.
The study found a greater risk than initially predicted of rapid kidney function decline in nephrosclerosis without diabetes (NS-DM) patients with low proteinuria levels.
There is no clarity on whether the effect of proteinuria on rapid kidney function decline is equivalent among non-DKD with diabetes (NDKD+DM), diabetic kidney disease (DKD), and nephrosclerosis without diabetes, particularly in patients with advanced chronic kidney disease (CKD). To clarify the same, Tomohito Gohda, Juntendo University Faculty of Medicine, Bunkyo-ku, Tokyo, Japan, and colleagues conducted a post hoc analysis using BRIGHTEN study data to compare the eGFR slope and the rapid kidney function decline prevalence, in addition to kidney and cardiovascular (CV) outcomes, in Japanese CKD patients among these three CKD categories.
The study included 1038 CKD patients who participated in the BRIGHTEN study. A linear mixed-effect model was applied to estimate each disease group’s annual glomerular filtration rate (eGFR) decline.
The following were the key findings of the study:
The findings showed that although NS-DM has a better kidney prognosis owing to its low proteinuria level, the kidney prognosis in NS-DM patients with a proteinuria level (0.5–1.0 g/g) may be worse than assumed.
“We propose a new concept that the effect (and weighting) of proteinuria on rapid kidney function decline may be different and greater in NS-DM patients with low proteinuria (0.5–1.0 g/g) levels compared with DKD or NDKD+DM patients with the same proteinuria level,” the researchers wrote.
They suggested that even a relatively low proteinuria level of up to 0.5 g/g should be given more aggressive treatment in patients with NS-DM because they are more likely to experience a rapid eGFR decline versus patients with DKD or NDKD+DM.
Reference:
Gohda, T., Murakoshi, M., Suzuki, Y., Kagimura, T., Wada, T., & Narita, I. (2024). Effect of proteinuria on the rapid kidney function decline in chronic kidney disease depends on the underlying disease: A post hoc analysis of the BRIGHTEN study. Diabetes Research and Clinical Practice, 212, 111682. https://doi.org/10.1016/j.diabres.2024.111682
Powered by WPeMatico
New Delhi: Amid rising heatwave conditions, the Ministry of Health, on Sunday, advised employers to implement essential heat safety measures in the workplace.
“From providing hydration stations to scheduling outdoor tasks during cooler hours, let’s ensure our workers stay cool, healthy, and productive,” the ministry said in a post on social media platform X.com.
In an animated post, the ministry called on employers to provide proper drinking water facilities at the workplace, news agency IANS reported.
Also Read:Amid Heatwave in Rajasthan: Leaves of doctors, paramedics cancelled
“Schedule strenuous and outdoor jobs in cooler times of the day, increase the frequency of rest breaks,” were some tips shared by the ministry.
It also advised employers to train workers to recognise symptoms of heat-related illness.
Exposure to extreme heat can affect health, ranging from rashes to serious and potentially fatal health problems such as heat exhaustion and heatstroke.
Headache, feeling dizzy, dehydration, and breathing problems are the common symptoms of heat-related illness, said the ministry.
Meanwhile, the India Meteorological Department (IMD) on Sunday issued a ‘red alert’ for many states in north India, including Delhi, over persistent heatwave and high temperatures.
In Delhi, the temperatures are likely to range between 43 and 47 degrees Celsius, the IMD said.
Powered by WPeMatico
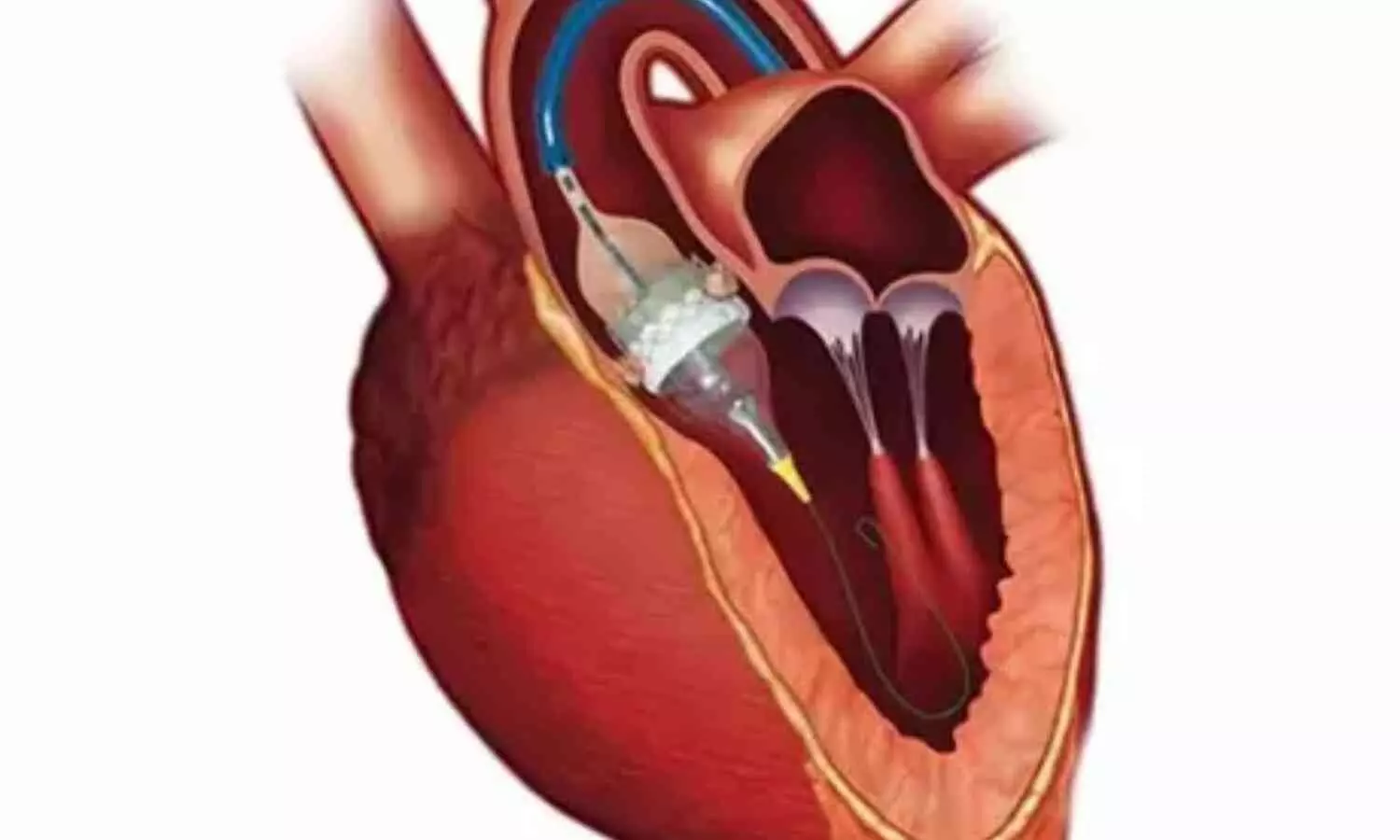
The Course Directors have selected 3 major Late Breaking Trials (LBTs) that were presented for the first time during the 2024 edition of EuroPCR. These trials were selected on account of their design, outcomes and potential to influence daily clinical practice. Among them is the NOTION-2 randomised clinical trial (RCT).
Evidence comparing the use of transcatheter aortic valve implantation (TAVI) and surgical aortic valve replacement (SAVR) in low-risk patients with aortic stenosis (AS) has led to the European Society of Cardiology (ESC) Clinical Practice Guideline recommendation1 that TAVI is indicated as the primary treatment option in patients older than 75 years, who are anatomically suitable for the procedure (Class I recommendation, level of evidence A).
In the NOTION-2 study, investigators from Denmark randomised patients ≤75 years of age to TAVI or SAVR – unlike previous RCTs, those with bicuspid valve anatomy were not excluded. The primary endpoint at 1 year included all-cause mortality, stroke and rehospitalisation (related to procedure/valve or heart failure).
TAVI and SAVR showed similar rates of the primary endpoint at 1 year (TAVI 10.2%, SAVR 7.1%; p=0.3), but this interpretation is limited by the small sample size, and the hypothesis of TAVI being noninferior to SAVR was formally not met. The mean age was 71.1 years. Among the secondary endpoints, TAVI resulted in a lower incidence of new onset atrial fibrillation and major bleeding, but a higher incidence of non-disabling stroke, paravalvular leak (PVL) and pacemaker implantation. A post hoc analysis demonstrated comparable results between TAVI and SAVR for tricuspid aortic valves (73% of all cases). However, in a non-prespecified analysis of the limited number of patients with bicuspid valves, outcomes were less favourable after TAVI (including the primary endpoint and the incidence of stroke).
Expanding TAVI indications to young patients with AS and longer life expectancy imposes specific challenges.
Firstly, a larger proportion of these young AS patients have bicuspid valve anatomy (27% in NOTION-2), and this group has been largely excluded from prior “low-risk” trials. Therefore, NOTION-2 provides new insights concerning the respective value of SAVR and TAVI in this anatomical setting. Given the strong indication of less favourable results with TAVI in this cohort, dedicated and larger randomised studies comparing TAVI and SAVR for this specific indication are now needed.
Secondly, achieving optimal results of TAVI (with low rates of pacemaker implantation, stroke and PVL) is particularly important in younger patients, given that these expectations are already provided by SAVR (as confirmed in NOTION-2).
Finally, the longer life expectancy of this cohort is likely to portend higher rates of a second TAVI procedure (namely TAV-in-TAV). Long-term follow-up and outcome analysis of NOTION-2 and other similar randomised trials (as well as larger scale registries) are therefore mandatory.
Self-expanding devices were used in 72.7% of patients in NOTION-2, and long-term follow-up will be very informative, since TAV-in-TAV procedures can be more challenging with these platforms. The results of the present study should not be extrapolated to the use of balloon-expandable devices; dedicated studies using these devices in patients with bicuspid AS are also required.
NOTION-2 provides further short-term data concerning the 1-year outcome of younger AS patients with tricuspid valve anatomy treated with TAVI compared to SAVR. Secondary clinical endpoints show mixed outcomes after TAVI and SAVR, which is consistent with previous randomised trials.
NOTION-2 also provides a “word of caution” concerning the use of TAVI in younger AS patients with bicuspid valve anatomy. Dedicated randomised trials comparing optimal TAVI with SAVR in younger patients with bicuspid aortic valve stenosis are now required.
Powered by WPeMatico

USA: Advancements in medical technology are rapidly transforming the landscape of cardiovascular health screening and diagnosis. Among these breakthroughs, artificial intelligence (AI) is taking center stage, particularly in cardiac magnetic resonance imaging (MRI).
An artificial intelligence-based cardiac MRI interpretation outperformed cardiologists in diagnosing pulmonary arterial hypertension and showed promise in a proof-of-concept study.
“This proof-of-concept study holds the potential to substantially advance the scalability and efficiency of CMR interpretation, thereby improving screening and diagnosis of cardiovascular disease (CVD),” the researchers wrote in their study published in Nature Medicine.
Cardiovascular diseases remain a leading cause of mortality worldwide, underscoring the critical need for accurate and timely detection. Traditional screening and diagnosis methods often rely on invasive procedures or lack the precision necessary for early intervention. However, AI algorithms integration into cardiac MRI promises to revolutionize this process, offering unprecedented accuracy and efficiency.
Cardiac MRI is the gold standard for cardiac function assessment and is crucial in CVD diagnosis. However, its widespread application is limited by the heavy resource burden of CMR interpretation.
To address this challenge, Yan-Ran (Joyce) Wang, School of Medicine, Stanford University, Stanford, CA, USA, and colleagues developed and validated computerized CMR interpretation for screening and diagnosis of 11 types of CVD in 9,719 patients.
The research team proposed a two-stage paradigm consisting of noninvasive cine-based CVD screening followed by cine and late gadolinium enhancement-based diagnosis.
The following were the key findings of the study:
The findings demonstrate that end-to-end video-based deep learning models can detect cardiac anomalies and further classify distinct CVDs from CMR with high classification performance.
“If confirmed in clinical settings, our study has the potential to substantially advance the scalability and efficiency of CMR interpretation, paving the way for widespread CMR use in CVD screening and diagnosis,” the researchers wrote.
In conclusion, AI-enabled cardiac MRI represents a paradigm shift in the screening and diagnosis of cardiovascular disease. By harnessing the power of artificial intelligence, healthcare providers can achieve earlier detection, more accurate diagnosis, and personalized treatment strategies. As this technology continues to evolve, it holds the potential to revolutionize cardiovascular care and improve patient outcomes globally.
Reference:
Wang, Y., Yang, K., Wen, Y., Wang, P., Hu, Y., Lai, Y., Wang, Y., Zhao, K., Tang, S., Zhang, A., Zhan, H., Lu, M., Chen, X., Yang, S., Dong, Z., Wang, Y., Liu, H., Zhao, L., Huang, L., . . . Zhao, S. (2024). Screening and diagnosis of cardiovascular disease using artificial intelligence-enabled cardiac magnetic resonance imaging. Nature Medicine, 1-10. https://doi.org/10.1038/s41591-024-02971-2
Powered by WPeMatico

Powered by WPeMatico

Researchers have found that suprazygomatic maxillary nerve (SZMN) blocks can significantly reduce postoperative opioid consumption and pain in children undergoing intracapsular adenotonsillectomy. This recent study was conducted to address the complications arising from opioid use in pediatric pain management post-surgery. The study was published in JAMA Otolaryngology- Head and Neck Surgery and was conducted by Carole Lin and colleagues.
Adenotonsillectomy, a common pediatric surgical procedure, often necessitates effective pain management. Traditional methods include opioids, which carry risks of adverse effects and potential complications. The use of nerve blocks presents an alternative for managing postoperative pain without relying heavily on opioids.
This prospective, randomized, blinded clinical trial was conducted at a single tertiary pediatric hospital from November 2021 to March 2023. Sixty pediatric patients aged 2-14 years, scheduled for intracapsular adenotonsillectomy, were included. Exclusion criteria included combined surgical procedures, developmental delay, coagulopathy, chronic pain history, known or predicted difficult airway, and unrepaired congenital heart disease. Participants were randomized into two groups: one receiving bilateral SZMN blocks (block group) and the other not receiving the blocks (control group).
Under general anesthesia, the block group received bilateral SZMN blocks. The primary outcomes measured were opioid consumption, FLACC (Face, Legs, Activity, Cry, Consolability) scores, and the rate of opioid-free stays in the postanesthesia care unit (PACU). Secondary outcomes included recovery duration and the incidence of adverse effects such as nausea, vomiting, block site bleeding, and emergency delirium.
The final analysis included 53 patients (mean age 6.5 years; 55% female, 45% male), with 26 in the block group and 27 in the control group.
The block group demonstrated a mean opioid morphine equivalent consumption of 0.07 mg/kg during PACU stay, significantly lower than the 0.15 mg/kg in the control group (mean difference, 0.08; 95% CI, 0.01-0.15; Cohen d, 0.64).
Additionally, 58% of patients in the block group had opioid-free PACU stays, compared to 26% in the control group (mean difference, 32%; 95% CI, 5%-53%).
FLACC scores were lower in the block group (0.7 vs. 1.6; mean difference, 0.9; 95% CI, 0.2-1.6; Cohen d, 0.7), indicating less pain.
Both groups had similar rates of adverse events, and no nerve block-related complications were reported.
The study’s findings support the use of SZMN blocks as an effective method for reducing opioid use and managing pain in pediatric intracapsular adenotonsillectomy. The nerve blocks provided meaningful reductions in postoperative opioid consumption and pain scores without increasing adverse effects.
Suprazygomatic maxillary nerve blocks are a valuable adjunct tool for managing postoperative pain in pediatric intracapsular adenotonsillectomy. They significantly reduce opioid consumption and pain scores, offering a safer and effective alternative to opioid-inclusive pain management strategies. Further research may solidify their role in pediatric surgical care.
Reference:
Lin, C., Abboud, S., Zoghbi, V., Kasimova, K., Thein, J., Meister, K. D., Sidell, D. R., Balakrishnan, K., & Tsui, B. C. H. (2024). Suprazygomatic maxillary nerve blocks and opioid requirements in pediatric adenotonsillectomy: A randomized clinical trial. JAMA Otolaryngology– Head & Neck Surgery. https://doi.org/10.1001/jamaoto.2024.1011
Powered by WPeMatico
