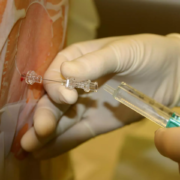
Blood test finds knee osteoarthritis up to eight years before it appears on X-rays: Study

A blood test successfully predicted knee osteoarthritis at least eight years before tell-tale signs of the disease appeared on x-rays, Duke Health researchers report.
In a study appearing in the journal Science Advances, the researchers validated the accuracy of the blood test that identifies key biomarkers of osteoarthritis. They showed that it predicted development of the disease, as well as its progression, which was demonstrated in their earlier work.
The research advances the utility of a blood test that would be superior to current diagnostic tools that often don’t identify the disease until it has caused structural damage to the joint.
“Currently, you’ve got to have an abnormal x-ray to show clear evidence of knee osteoarthritis, and by the time it shows up on x-ray, your disease has been progressing for some time,” said senior author Virginia Byers Kraus, M.D., Ph.D., a professor in the departments of Medicine, Pathology, and Orthopedic Surgery at Duke University School of Medicine. “What our blood test demonstrates is that it’s possible to detect this disease much earlier than our current diagnostics permit.”
Osteoarthritis (OA) is the most common form of arthritis, afflicting an estimated 35 million adults in the U.S. and causing significant economic and societal impacts. While there are currently no cures, the success of potential new therapies could hinge on identifying the disease early and slowing its progression before it becomes debilitating.
Kraus and colleagues have focused on developing molecular biomarkers that can be used for both clinical diagnostic purposes and as a research tool to aid in the development of effective drugs. In previous studies, the blood biomarker test demonstrated 74% accuracy in predicting knee OA progression and 85% accuracy in diagnosing knee OA.
The current study further honed the test’s predictive capabilities. Using a large United Kingdom database, the researchers analyzed serum of 200 white women, half diagnosed with OA and the other half without the disease, matched by body mass index and age.
They found that a small number of biomarkers in the blood test successfully distinguished the women with knee OA from those without it, catching molecular signals of OA eight years before many of the women were diagnosed with the disease by x-ray.
“This is important because it provides more evidence that there are abnormalities in the joint that can be detected by blood biomarkers well before x-rays can detect OA,” Kraus said. “Early-stage osteoarthritis could provide a ‘window of opportunity’ in which to arrest the disease process and restore joint health.”
Reference:
Virginia Kraus, An Osteoarthritis Pathophysiological Continuum Revealed by Molecular Biomarkers, Science Advances (2024). DOI: 10.1126/sciadv.adj6814.
Powered by WPeMatico