An antibacterial protein provides a new therapeutic target against pancreatic cancer
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Hyderabad: The Telangana Government Doctors Association (TGDA) held a round table
conference on Tuesday at the Superintendent Seminar Hall to discuss the urgent
need for a new Osmania General Hospital (OGH) building.
The current heritage structure, established over a century ago by the
Nizams, is in immediate need of repair, raising serious concerns about patient
safety and the hospital’s ability to serve the increasing number of patients.
Despite assurances from the previous BRS government to address these
issues, no significant progress has been made. The TGDA questioned why the same
urgency applied to building the new Secretariat was not extended to the OGH’s
needs. The association also criticized the government’s non-compliance with the
Heritage Act procedures, reports Deccan Chronicle.
The association proposed alternative locations for the new hospital,
including the Chanchalguda jail area and the nearby government printing press,
which is situated on approximately 35 acres of land. Another suggestion was
converting Goshamahal Stadium into hospital premises which will provide an
additional 30 acres for the construction, reports The Daily. They emphasized that a state-of-the-art
facility can be constructed using the area to offer super-speciality services
across various departments, requiring a total of 40 acres.
Dr Ramesh Barigela, association founding president, highlighting the
inadequacies of the existing structure, said, “The OGH building, both in
terms of treatment capacity and physical space, is grossly insufficient. We
were promised that it would be taken down, yet only drawings and unfulfilled
promises have surfaced.”
The conference was attended by Prof M. Kodandaram, Dr N. Krishna
Reddy, chairman of the OMC Alumni Trust, and Dr S. Krishna Murthy, secretary
of the OMC Alumni Association. Among the key demands from the discussions, the demolition
of the old heritage structure may be mentioned. The structure occupies only six of the 26.5-acre
site and using the area for a modern hospital has been in talks.
The doctors urged the government to take steps to improve the health
sector, stating that their proposals help save Osmania Medical College’s
legacy as well as enable the facility to serve as a leading medical
institution nationwide.
Also Read: Osmania General Hospital inaugurates first state-run transgender clinic
Powered by WPeMatico

Hyderabad: The suspected mastermind in the international organ trafficking racket operating out of Kerala has been arrested by the police and the accused has been identified as a renowned doctor from Hyderabad.
Based on a tip-off, a special investigation team (SIT), headed by Ernakulam Rural SP Vaibhav Saxena travelled to Hyderabad to nab the doctor who is the alleged mastermind in the racket. However, the police have refused to publicly disclose his name citing that the investigation is under process.
The doctor’s involvement was revealed when another person from Kerala, who was first detained by the police, disclosed that three individuals, including a renowned doctor from Hyderabad, were involved in the illegal operation.
Also read- International Organ Trafficking Racket: 2 Accused Arrested, NIA To Take Over Probe
After the doctor’s arrest, the police are now focused on tracing and arresting the two other suspects in the case.
Medical Dialogues team had earlier reported about the incident where the Ernakulam Rural Police Special Investigation Team (SIT) apprehended one more accused in connection with the case after the arrest of Kerala native Sabith Naseer from Cochin International Airport following a tip-off from central agencies regarding his frequent travels to Iran from Kochi and other destinations.
According to his remand report, he admitted to taking 20 people from various states of India to Iran to sell their kidneys. He admitted that he used to get Rs 5 lakh per kidney donor and each donor was paid anywhere between Rs 5 to Rs 10 lakh.
He also admitted that there is an organised network behind this. Based on the complaints filed by the relatives of the organ donors, the central agencies traced the doctor in Hyderabad.
Speaking with Siasat Daily, Ernakulam Rural SP Vaibhav Saxena, who is leading the investigations, said, “Sabit Nasir was arrested at the Kochi International Airport upon his arrival from Iran. He confessed to running an underground network of kidney sales. He also revealed that three people, including a renowned doctor from Hyderabad, were involved in the racket.”
Talking about the increasing number of such illegal activities, Dr Anil Kumar, a consultant senior physician in the city told Deccan Chronicle, “This is a grave issue and calls for immediate attention. We need to raise awareness among the public about the dangers of falling prey to such schemes. Strict laws and severe punishments must be enforced to deter heinous characters.”
Also read- Mumbai: BHMS Doctor Among 7 Held In Child Trafficking Racket
Powered by WPeMatico

Brazil: In a comprehensive systematic review poised to transform approaches to type 2 diabetes mellitus (T2DM) management, researchers have underscored the pivotal role of dietary fiber in optimizing glycemic control and improving overall health outcomes for individuals with T2DM. This landmark study, encompassing a rigorous analysis of existing evidence, highlights the profound impact of dietary fiber intake on mitigating key risk factors associated with T2DM progression.
The study, published in the World Journal of Diabetes, showed that dietary fiber is a valuable strategy in T2DM treatment, improving health outcomes. DF intake holds the potential to improve quality of life and reduce mortality and complications associated with diabetes.
Similarly, through enriched foods or supplements, DF significantly contributes to the control of several markers, such as blood glucose, HbA1c, low-density lipoprotein, triglycerides, and body weight.
Type 2 diabetes mellitus, a chronic metabolic disorder characterized by insulin resistance and elevated blood sugar levels, represents a significant public health challenge worldwide. While pharmacological interventions remain a cornerstone of T2DM management, emerging research has increasingly emphasized the importance of dietary interventions in complementing traditional treatment modalities and enhancing long-term outcomes.
The etiology of type 2 diabetes is closely related to sedentary lifestyles and imbalanced dietary practices. Conversely, increasing dietary fiber intake has consistently demonstrated health benefits in several studies, including better glycemic control and weight management.
Against the above background, Douglas Nitzke, Department of Nutrition, Centro Universitário CESUCA, Cachoeirinha, Brazil, and colleagues aimed to investigate the efficacy of DF interventions in T2DM management.
For this purpose, the research team conducted a systematic literature review to explore the association between DF intake and type 2 diabetes management. Following the exclusion and inclusion criteria, the review included 26 studies.
The following were the key findings of the study:
The researchers, however, suggest that weight loss is more impacted by calorie restriction rather than by the amount of fiber in the diet.
“Hence, future clinical studies should further explore the combination of increased DF intake and calorie restriction, as this strategy presents the most valuable results in T2DM management,” they wrote.
The systematic review not only elucidates the therapeutic potential of dietary fiber in T2DM management but also underscores the importance of dietary modifications as a cornerstone of personalized treatment approaches. As healthcare providers increasingly recognize the pivotal role of nutrition in chronic disease management, the findings of this landmark study offer actionable insights that can inform clinical practice guidelines and empower individuals with T2DM to take proactive steps toward better health outcomes.
Reference:
Nitzke, Douglas, et al. “Increasing Dietary Fiber Intake for Type 2 Diabetes Mellitus Management: a Systematic Review.” World Journal of Diabetes, vol. 15, no. 5, 2024, pp. 1001-1010.
Powered by WPeMatico
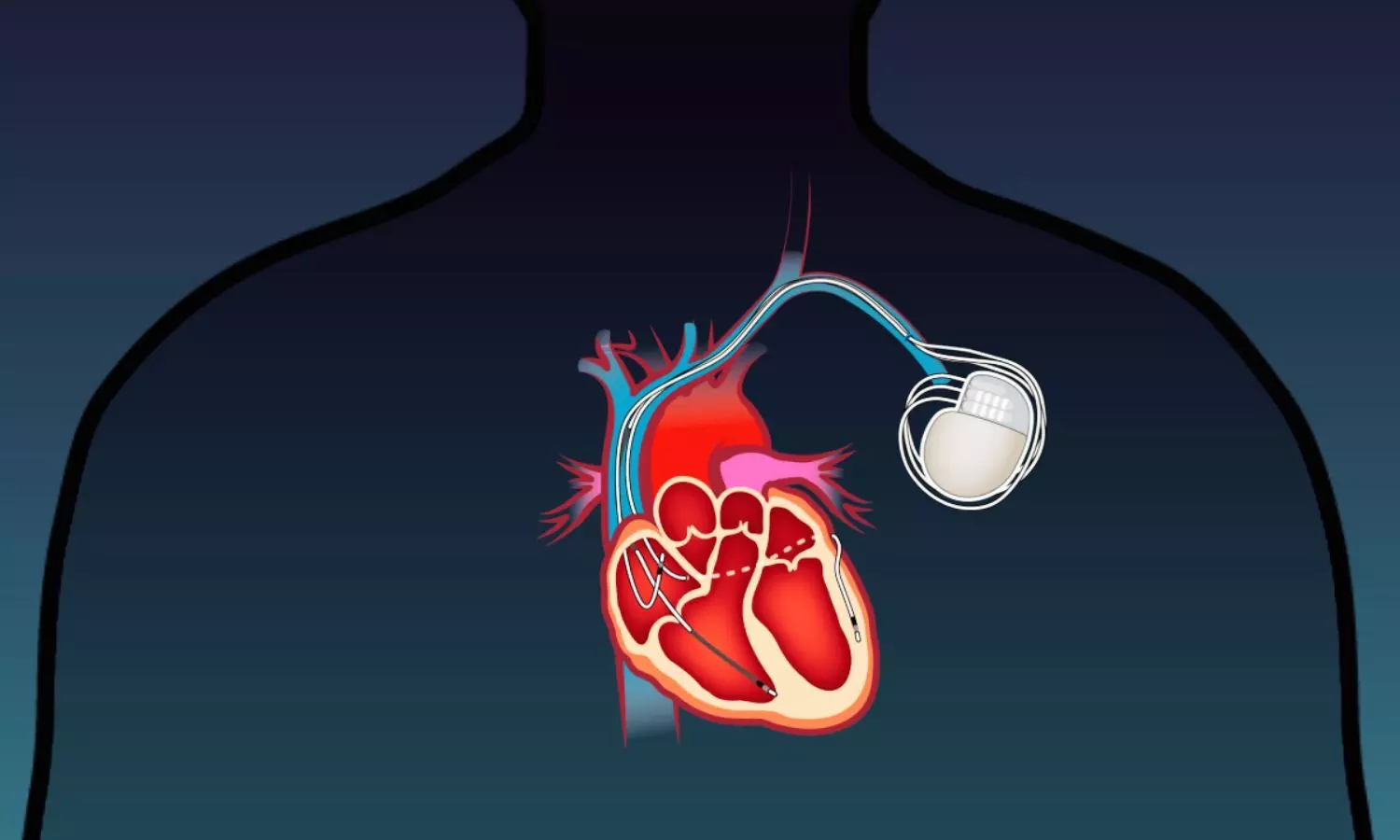
USA: In a significant breakthrough for cardiac care, the Global LEADR pivotal trial has unveiled promising results regarding the safety, efficacy, and reliability of a groundbreaking small-diameter defibrillation lead. The study, conducted across multiple international sites, marks a significant advancement in cardiac device technology and offers new hope for patients with heart rhythm disorders.
The trial published in Heart Rhythm showed that a small-diameter, defibrillation lead that can be delivered through existing commercially available catheters for targeted placement is safe and durable, with no incidence of fractures in 1 year.
“The OmniaSecure lead exceeded prespecified primary endpoint performance goals for efficacy and safety, showing high defibrillation success and a low occurrence of lead-related major complications with zero lead fractures,” the study stated. The OmniaSecure defibrillation lead is a small-diameter, novel, catheter-delivered lead designed for targeted placement as per the established SelectSecure SureScan MRI Model 3830 lumenless pacing lead platform.
Implantable cardioverter-defibrillators last longer, and there is a growing interest in reliable leads with targeted lead placement. Considering this, Pamela K. Mason, University of Virginia Medical Center, Charlottesville, Virginia, and colleagues assessed the safety and efficacy of the OmniaSecure defibrillation lead.
The worldwide LEADR pivotal clinical trial was conducted at 45 global sites and comprised 675 patients (mean age 62; 26% female) with an indication for de novo implantation of a defibrillator or a cardiac resynchronization therapy defibrillator (CRT-D). The mean LVEF was 35.3%, and 26% of patients had atrial fibrillation.
The primary efficacy endpoint was successful defibrillation at implantation per protocol. The primary safety endpoint was freedom from study lead–related major complications at six months. The primary safety and efficacy objectives were met if the lower bound of the 2-sided 95% credible interval was >88% and >90%, respectively.
The researchers reported the following findings:
· 643 patients successfully received the study lead, and 505 patients have completed 12-month follow-up.
· The lead was placed in the desired right ventricular location in 99.5% of patients.
· Defibrillation testing at implantation was completed in 119 patients, with success in 97.5%.
· The Kaplan-Meier estimated freedom from study lead–related major complications was 97.1% at 6 and 12 months.
· The trial exceeded the primary efficacy and safety objective thresholds.
· There were zero study lead fractures, and electrical performance was stable throughout the mean follow-up 12.7.
The findings showed that the unique design and small diameter of the OmniaSecure lead have the potential to offer significant clinical benefits for physicians and patients, such as comprehensive reliability, low complication rate, and ability to position the lead in the physician’s desired RV location, while exceeding or maintaining performance of historical larger diameter, stylet-delivered transvenous defibrillation leads.
Reference:
Crossley GH, Sanders P, Hansky B, De Filippo P, Shah MJ, Shoda M, Khelae SK, Richardson T, Philippon F, Zakaib JS, Tse HF, Sholevar DP, Stellbrink C, Pathak RK, Milašinović G, Chinitz JS, Tsang B, West MB, Ramza BM, Han X, Bozorgnia B, Carta R, Geelen T, Himes A, Platner M, Thompson AE, Mason P; Lead EvaluAtion for Defibrillation and Reliability Trial Investigators. Global LEADR pivotal trial results. Heart Rhythm. 2024 May 7:S1547-5271(24)02395-6. doi: 10.1016/j.hrthm.2024.04.067. Epub ahead of print. PMID: 38762820.
Powered by WPeMatico
USA: Recent findings from a multicohort analysis have shed new light on the relationship between high-density lipoprotein (HDL) parameters and the risk of heart failure. The study, published in JACC: Heart Failure, conducted across multiple cohorts, offers valuable insights into the role of HDL cholesterol in cardiovascular health.
The researchers found that HDL particle concentration (HDL-P) is associated with a lower risk of heart failure (HF). In contrast, larger HDL size was tied to a higher HF risk, and they observed no significant association between HDL-C and HF risk after accounting for cardiovascular (CV) risk factors.
High-density lipoprotein (HDL) is commonly characterized by its cholesterol concentration (HDL-C) and an inverse association with atherosclerotic cardiovascular disease (ASCVD). Ambarish Pandey, the University of Texas Southwestern Medical Center, Dallas, Texas, USA, and colleagues sought to evaluate the association of HDL particle concentration (HDL-P), HDL-C, HDL particle size (HDL-size), and cholesterol content per particle (HDL-C/HDL-P) with risk of overall heart failure and subtypes.
The study led to the following findings:
Higher HDL-P and smaller HDL-size were each associated with a lower risk of overall HF, and these associations do not seem to be driven by ASCVD events in a diverse cohort of community-dwelling adults.
“There is a need for additional studies to evaluate further the implications of modulating HDL-size and HDL-P and the potential utility for HF prevention,” the researchers wrote.
In conclusion, the multicohort analysis provides compelling evidence of the inverse association between HDL parameters and the risk of heart failure. Higher levels of HDL cholesterol and increased HDL particle concentration appear to confer protection against heart failure incidence. These findings underscore the importance of promoting cardiovascular health through strategies that enhance HDL levels, potentially offering avenues for reducing the incidence of heart failure and improving overall cardiovascular outcomes.
Reference:
Pandey, A., Patel, K. V., Segar, M. W., Shapiro, M. D., Ballantyne, C. M., Virani, S. S., Nambi, V., Michos, E. D., Blaha, M. J., Nasir, K., Cainzos-Achirica, M., Ayers, C. R., Westenbrink, B. D., Flores-Guerrero, J. L., Bakker, S. J., Connelly, M. A., Dullaart, R. P., & Rohatgi, A. (2024). Association of High-Density Lipoprotein Parameters and Risk of Heart Failure: A Multicohort Analysis. JACC: Heart Failure. https://doi.org/10.1016/j.jchf.2024.03.007
Powered by WPeMatico

Bengaluru: In a first reported case across the globe, Fortis Hospital Cunningham Road successfully conducted three simultaneous complex procedures – Coronary Artery Bypass Grafting (CABG), gallbladder stone removal, and colon cancer surgery in one session.
Under the multi-disciplinary expertise of Dr Vivek Jawali, Chairman-Cardiac Sciences, Fortis Hospitals, Bengaluru and Dr Ganesh Shenoy, Director-GI, Minimal Access & Bariatric surgery, Fortis Hospital, Cunningham Road Bengaluru, the complex procedures were successfully completed in mere 7 hours.
Patient Mr. Kopparam, had a medical history of diabetes and heart disease – diagnosed 36 months ago. He was suffering from persistent abdominal pain and underwent an ultrasound examination at Fortis Cunningham Road. The diagnosis revealed the presence of gallstones, prompting further evaluation. However, subsequent tests resulted in a more concerning situation.
Also Read:Fortis Hospital Bannerghatta Road performs two complex Robotic Kidney Transplants
He had cancerous growth in the colon, which posed a significant challenge in Mr. Kopparam’s treatment plan, particularly due to his pre-existing heart condition, which was being managed with blood thinners. The co-existence of colon cancer and heart disease necessitated a carefully orchestrated approach to treatment, considering the potential risks associated with the patient’s condition during surgery.
Performing the Coronary Artery Bypass Grafting (CABG) first, was crucial to ensure the patient’s heart was stable before proceeding with the colon cancer surgery. If the cardiac surgery had been done first, there would have been a 3-month wait for the colon cancer surgery, but delay wasn’t an option because of the progressive growth in the tumour. Post multiple evaluations and consultations with the doctors’ team, and post the patients and family’s consent, it was decided to proceed with all the three surgeries simultaneously, under general anaesthesia.
Dr Vivek Jawali, Chairman – Cardiac Sciences, Fortis Hospitals, Bengaluru, said, “We employed a specialized surgical technique known as OPCAB (Off-Pump Coronary Artery Bypass) with 4 grafts (blood vessels that are transplanted into a patient’s body to repair or replace damaged ones) to perform the heart surgery. This method, unlike traditional approaches, eliminates the need for a heart-lung machine.
We carefully monitored the heart and gave medications to keep the blood pressure and sugar levels normal during the surgery. We took 4 blood vessels from the patient’s body to create new pathways around the blocked arteries in the heart. This helped improve blood flow to the heart muscle. The whole surgery took about 260 minutes (a little over 4 hours), and the patient was stable.”
Dr Ganesh Shenoy, Director – GI, Minimal Access & Bariatric Surgery, Fortis Hospital, Cunningham Road Bengaluru, said, “We are proud that we could successfully perform this one-of-a-kind simultaneous triple surgery on a 44-year-old patient, skilfully addressing his complex medical conditions, all in a single surgical session. Utilizing advanced laparoscopic techniques, we executed a laparoscopic extended right hemicolectomy (LERHC) to remove a portion of the colon affected by cancer, along with a laparoscopic cholecystectomy (LC) for the removal of gallbladder stones.
This intricate procedure demanded precise coordination and multi-disciplinary approach due to the complexity of colon cancer surgery, yet it minimized surgical risks and facilitated a smoother and faster recovery for the patient. This comprehensive approach was essential to address all his health concerns at once.”
The patient was discharged from the hospital 15 days after the surgery and has since resumed his normal daily activities without any complications.
Mr. Akshay Oleti, Business Head, Fortis Hospitals Bengaluru, said, “This ground-breaking surgery, marks the world’s first such procedure conducted and demonstrates the exceptional skill of our medical team in handling complex procedures. It represents the dedication and expertise of our doctors, as well as our hospital’s commitment to pushing boundaries and innovative approaches in healthcare.”
Powered by WPeMatico
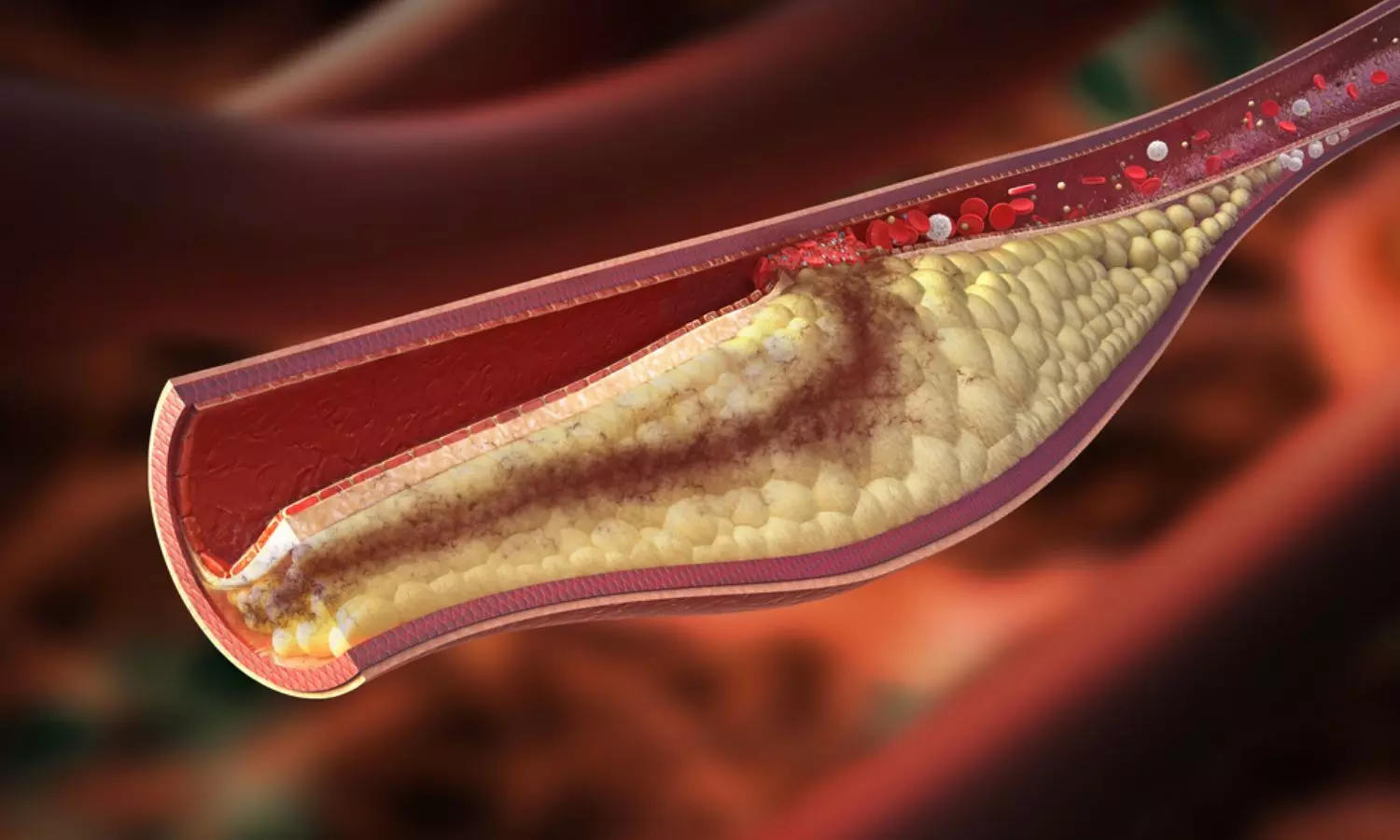
Bulgaria: In a quest to unravel the intricate links between metabolic health and cardiovascular risk, a recent study has delved into the common carotid artery intima-media thickness (CIMT) in individuals with prediabetes and those newly diagnosed with type 2 diabetes mellitus (T2DM). The findings, published in the Journal of Diabetes and its Complications, offer valuable insights into early vascular changes associated with these conditions, potentially paving the way for enhanced risk stratification and preventive interventions.
The study found significantly greater intima-media thickness of the common carotid artery and a greater frequency of abnormal CIMT values in patients with new-onset diabetes compared to those with prediabetes and normoglycemia.
“CIMT has a high predictive value for the presence of sudomotor dysfunction, diabetic neuropathy, and the risk of new-onset diabetes,” the researchers wrote.
Antoaneta Gateva, University Hospital Alexandrovska, Bulgaria, and colleagues aimed to evaluate the relationship between common carotid artery intima-media thickness in patients with prediabetes and new-onset diabetes mellitus without proven cardiovascular disease (CVD) and some classic cardio-metabolic risk factors.
The study included 461 obese patients with an average age of 53.2 ± 10.7 years. They were divided into three groups – group 1 without carbohydrate disturbances (n = 182), group 2 with prediabetes (n = 193), and group 3 with newly diagnosed diabetes mellitus (n = 86).
Based on the study, the researchers reported the following:
The findings show a clear association between increased IMT and the presence of sudomotor dysfunction and diabetic neuropathy. A high predictive value was also found for the presence of these complications. As CIMT is much easier to measure than a full Ewing battery, the study findings can be used to select patients for further evaluation for autonomic dysfunction.
“The results show that the significant predictive value of CIMT is present in patients above 45 years of age, so according to us, CIMT measurement should be performed in obese patients over 45 years of age and in cases where abnormal results are present (≥0.7 mm), the patients should be referred to carbohydrate and autonomic function evaluation,” the researchers wrote.
“Despite the abundance of data on the relationship between CIMT, carbohydrate disturbances, and the CVD risk progression, we demonstrate for the first time its predictive role for progression to diabetes in obese patients,” they concluded.
Reference:
Gateva, A., Assyov, Y., Karamfilova, V., & Kamenov, Z. (2024). Common carotid artery intima media thickness (CIMT) in patients with prediabetes and newly diagnosed type 2 diabetes mellitus. Journal of Diabetes and its Complications, 38(7), 108766. https://doi.org/10.1016/j.jdiacomp.2024.108766
Powered by WPeMatico

Researchers from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, have found links between heart failure and kidney disease that support new approaches for integrating the care of these conditions. In an analysis that included adults ages 65 and older who were hospitalized for heart failure from across 372 sites in the U.S., researchers found that patients had a substantial risk of kidney complications, with approximately 6 percent progressing to dialysis within a year of being hospitalized for heart failure. The new results are published in JAMA Cardiology.
“We know that heart and kidney health are highly interconnected, but management of heart and kidney disease remains relatively siloed, and kidney health often isn’t prioritized in patients with heart disease until advanced stages,” said first author John Ostrominski, MD, a fellow in Cardiovascular Medicine and Obesity Medicine at the Brigham. “Declining kidney function is often asymptomatic until late in the disease course, but even less advanced stages of kidney impairment can have important implications for cardiovascular health. Hence, there’s a need for analyses that assess kidney outcomes in people with heart failure.”
About two thirds of older adults with heart failure have abnormal kidney function. However, few analyses to date have investigated the occurrence of clinically relevant kidney outcomes, such as hospitalization for acute kidney injury or dialysis, in patients with heart failure. Evaluating these more recognizable and patient-centered outcomes, according to Ostrominski, may result in substantial changes to the way that heart and kidney disease are managed together in the clinic.
The study analyzed Medicare claims data from 85,298 patients over the age of 65 who were hospitalized with heart failure between 2021 and 2024. The data was sourced from the Get with the Guidelines-Heart-Failure Registry, an initiative supported by the American Heart Association that seeks to connect hospitals with current evidence-based guidelines and accurate measurement tools to improve care quality and industry practices. The registry is also proving a valuable source of information for researchers examining trends in health outcomes for patients with heart failure.
In the present study, 63 percent of patients were discharged with significantly impaired kidney function, as measured by their rate of filtration. The researchers also found that the risk of adverse kidney outcomes increased steeply in patients with lower kidney function. By one year after discharge, 6 percent of patients were on dialysis, and 7 percent of patients were either on dialysis or had progressed to end stage kidney disease.
The findings suggest that at the individual provider level, cardiologists should prioritize assessing kidney function-including measuring kidney filtration and looking for evidence of protein in the urine, also known as albuminuria-in all patients with heart failure, and, when indicated, consider heart therapies that are known to improve kidney outcomes.
More broadly, the study emphasizes the need for systemic changes that better support the simultaneous management of heart and kidney disease, including establishing clinics focused on integrating these two care areas, incorporating kidney outcomes into health care performance metrics for cardiovascular diseases, and expanding Medicare reimbursement protocols for interdisciplinary chronic care management.
Researchers at Mass General Brigham are actively engaged as sites for clinical trials evaluating newer treatment strategies for individuals with cardiovascular and kidney disease. The Accelerator for Clinical Transformation team is also developing new ways of delivering care-including medications with established kidney benefits-to eligible patients with and without heart failure.
“The trends we’ve observed aren’t especially surprising given what we know about the links between heart and kidney health, but what’s important is that this research emphasizes the scope of the problem and gives us information we can act upon to directly improve clinical outcomes in patients with heart failure,” said Ostrominski. “There are important opportunities for patients and providers, healthcare institutions, and, at the broader state and national levels, in terms of healthcare policy that could make a big difference for patients.”
Reference:
Ostrominski JW, Greene SJ, Patel RB, et al. Kidney Outcomes Among Medicare Beneficiaries After Hospitalization for Heart Failure. JAMA Cardiol. Published online May 29, 2024. doi:10.1001/jamacardio.2024.1108.
Powered by WPeMatico
