Elevated serum androgen levels in patients with PCOS associated with multiple metabolic abnormalities: Study
Elevated serum androgen levels in patients with PCOS associated with multiple metabolic abnormalities suggest a study published in the Gynecological Endocrinology.
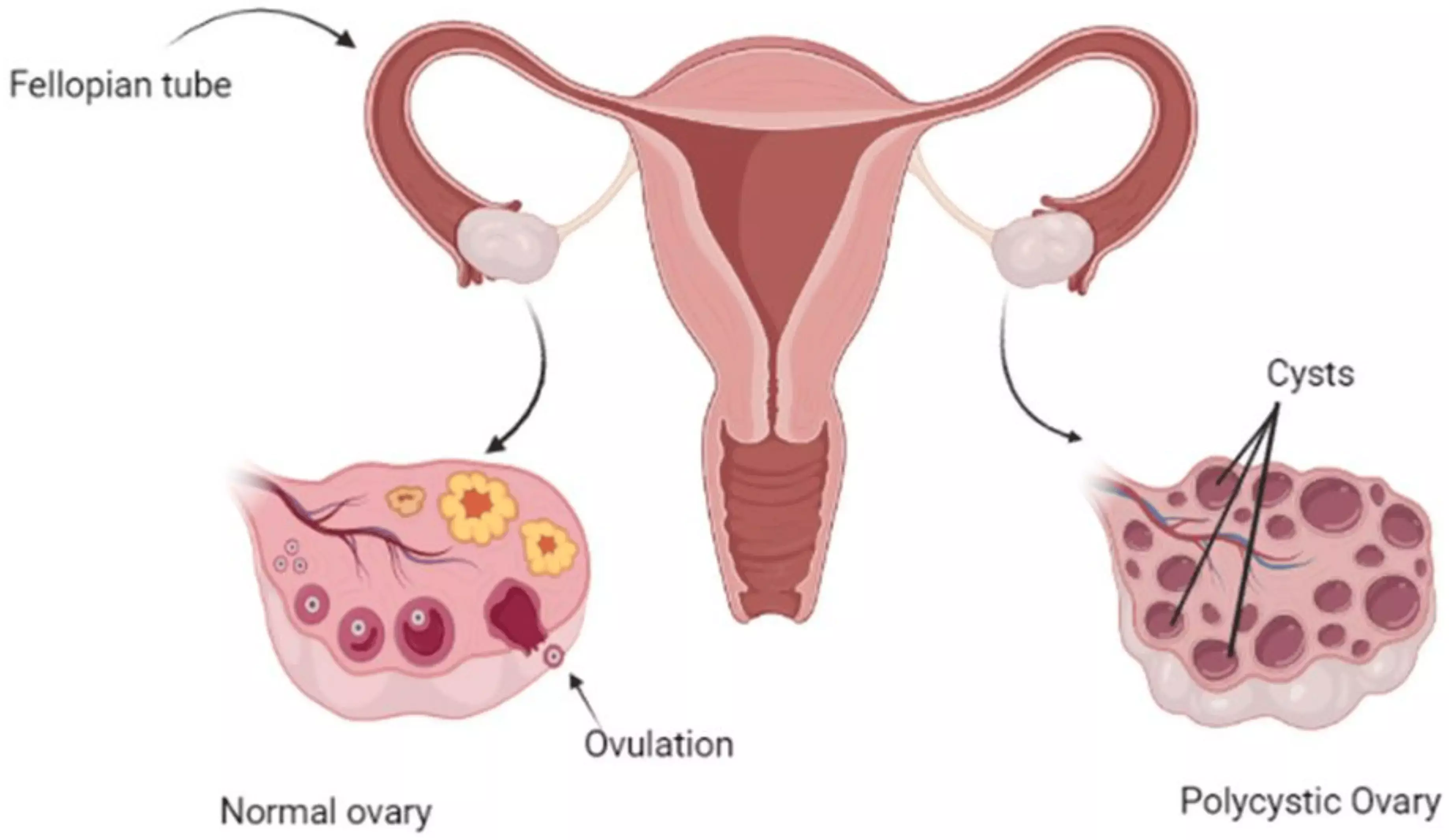
This study aimed to investigate the impact of serum androgen levels on metabolic profiles in patients with polycystic ovary syndrome (PCOS). They included 216 patients with PCOS and 216 healthy individuals selected as the control group. According to the measured serum androgen levels, patients with PCOS were divided into the hyperandrogenism group and non-hyperandrogenism group. Clinical metabolic indicators were assessed and compared between the two groups. Additionally, they assessed the correlation between androgen levels and clinical metabolic indicators.
Results: The body mass index, waist-to-hip ratio, mF-G score, and acne score, as well as T, LH, LSH/FSH, FPG, Cr, UA, TG, TC, and LDL-C levels were significantly higher in the PCOS group than in the control group. The incidence of hyperandrogenism and clinical hyperandrogenism in the PCOS group was significantly higher than that in the control group. Regarding clinical hyperandrogenism, hirsutism, acne, and acanthosis nigricans were significantly more common in the PCOS group than in the control group. Serum androgen levels were significantly correlated with the mF-G score, acne score, FSH, glucose concentration at 30 min, glucose concentration at 60 min, glucose concentration at 120 min, FINS, N120, HOMA-IR, HbA1c, AUCG, UA, TG, and hHDL-Clevels. Elevated serum androgen levels are commonly observed in patients with PCOS and are associated with multiple metabolic abnormalities. Therefore, it is recommended to regularly monitor glucose and lipid metabolism-related indicators in patients with PCOS who have elevated androgen levels.
Reference:
Ting Z, Xinghua T, Xiao X, Lingchuan L, Xiaomei W, Tao Y. The impact of androgen levels on serum metabolic profiles in patients with polycystic ovary syndrome. Gynecol Endocrinol. 2024 Dec;40(1):2352136. doi: 10.1080/09513590.2024.2352136. Epub 2024 May 11. PMID: 38733359.
Powered by WPeMatico