Disordered Eating Behaviors Prevalent in T1D Individuals Using Insulin Pumps, claims study

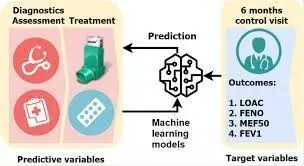
A recent cross-sectional study uncovered a significant connection between disordered eating behaviors (DEB) and diabetes management among young individuals who use insulin pumps. The findings were published in the Diabetes Technology & Therapeutics Journal.
This study included 167 young individuals of age 13 to 21 years who were having with type 1 diabetes (T1D) and used insulin pumps. The outcome yielded crucial insights into the prevalence of disordered eating behaviors and their impact on diabetes outcomes. DEB is more common among those with T1D who were found to be associated with higher HbA1c levels which indicate the potential challenges in diabetes management.
This observational, cross-sectional investigation utilized data from medical records of patients and self-reported questionnaires. Of the participants, 42.5% exhibited DEB, with notable associations found. Female sex, higher BMI-Z-score, elevated HbA1c levels, and increased rates of pump discontinuation were positively linked to the presence of DEB.
Also, this study looked into the use of hybrid closed-loop (HCL) systems by comparing them to traditional insulin pumps. Among individuals without DEB, the HCL system users showed a higher BMI-Z-score and a tendency toward lower HbA1c levels. For those with DEB, HCL system use lowered HbA1c levels. The findings suggest a nuanced relationship between DEB, insulin delivery systems, and the overall diabetes management.
These outcome highlight the prevalence of DEB among young individuals managing T1D with insulin pumps. The association between DEB and higher HbA1c levels underscores the potential hurdles in glycemic control. The introduction of HCL systems into the analysis adds a layer of complexity by revealing differing impacts based on the presence or absence of DEB. This emphasize the importance of regular screening for DEB and associated risk factors to enhance diabetes management.
Reference:
Propper-Lewinsohn, T., Elran-Barak, R., Gillon-Keren, M., Yackobovitch-Gavan, M., Liberman, A., Phillip, M., & Shalitin, S. (2023). Disordered eating behaviors among adolescents and young adults with type 1 diabetes treated with insulin pumps and hybrid closed-loop systems. In Diabetes Technology & Therapeutics. Mary Ann Liebert Inc. https://doi.org/10.1089/dia.2023.0500
Powered by WPeMatico