Study finds young girls most sensitive to PFAS ‘forever chemicals’ found in Australian vegetables
Powered by WPeMatico
Powered by WPeMatico

In a recent development, the European Medicines Agency’s safety committee, PRAC, has recommended the suspension of the marketing authorizations for medicines containing 17-hydroxyprogesterone caproate (17-OHPC) across the European Union (EU). This recommendation follows a comprehensive review conducted by PRAC, revealing a potential yet unconfirmed risk of cancer in individuals exposed to 17-OHPC in utero.
In some EU countries, 17-OHPC medicines are authorised as injections to prevent pregnancy loss or premature birth in pregnant women. They are also authorised for the treatment of various gynaecological and fertility disorders, including disorders caused by a lack of a hormone called progesterone.
The PRAC reviewed the results from a large population-based study, which looked at the risk of cancer in people who had been exposed to 17-OHPC in the womb, over a period of about 50 years from the time they were born. Data from this study suggest that these people might have an increased risk of cancer compared with those who were not exposed to the medicines. However, the PRAC noted that there was a low number of cancer cases in the study and that the study had some limitations, such as limited information on risk factors for cancer. The Committee therefore concluded that the risk of cancer in people exposed to 17-OHPC in the womb is possible, but cannot be confirmed due to uncertainties.
In its review, the PRAC also considered data on the effectiveness of 17-OHPC medicines in their authorised uses, including the results from a study looking at how well they prevented premature birth. The study, which involved over 1,700 pregnant women with a history of preterm delivery, found that 17-OHPC is no more effective than placebo (a dummy treatment) in preventing recurrent premature birth or medical complications due to prematurity in newborns. The Committee also reviewed two published meta-analyses (combined analyses of multiple studies), which confirmed that 17-OHPC is not effective at preventing preterm birth. For the other authorised uses of 17-OHPC, the PRAC concluded that there is limited evidence of effectiveness. During the review, input was also sought from experts in obstetrics, gynaecology and fertility treatment, and from patient representatives.
“In terms of efficacy, data from a multicentre, double-blind randomised controlled trial have shown a lack of efficacy of 17-OHPC in the prevention of preterm birth; there are limited data on efficacy in other obstetric, gynaecological and fertility indications authorised in the EU,” the release stated.
In view of the concern raised by the possible risk of cancer in people exposed to 17-OHPC in the womb, together with the data on the effectiveness of 17-OHPC in its authorised uses, the PRAC considered that the benefits of 17-OHPC do not outweigh its risks in any authorised use. The Committee is therefore recommending the suspension of the marketing authorisations for these medicines. Alternative treatment options are available.
“Healthcare professionals should no longer prescribe or dispense 17-OHPC medicines and should consider appropriate alternatives for any indication. Other treatment options are available. If you are using a medicine containing 17-OHPC, your doctor will discuss switching to a suitable alternative with you. The outcome of this review does not affect the use of progesterone, which works in a different way to 17-OHPC,” the release added.
Powered by WPeMatico

Salem: In a remarkable achievement, Dr Venkatesh Karthikeyan has been appointed as the National Convenor of the Indian Medical Association (IMA) Standing Committee for Antimicrobial Resistance.
As the National Convenor, Dr Venkatesh will oversee the increasing problem of antimicrobial resistance (AMR) in India and offer strategies to tackle it. His leadership will undoubtedly contribute positively to the organization and healthcare landscape in the country.
Dr Venkatesh Karthikeyan completed his MBBS from Velammal Medical College & Research Institute in 2020 and his MD in Community & Family Medicine from the prestigious institute, AIIMS Patna. He is currently a senior resident doctor at AIIMS Patna.
Also read- West Bengal: Paediatrician Dr Kaustav Nayek Takes Charge As New DME
According to WHO (World Health Organization), antimicrobial resistance (AMR) causes an estimated 5 million deaths every year globally, with projections suggesting a rise to 10 million by 2050. This escalation is due to the spread of resistant organisms, leading to ineffective treatment of infections and increased mortality.
Since Antimicrobial resistance rising at an alarming rate in India, IMA has decided to appoint him to address the issue that threatens public health and advances in medical treatment. The IMA plays a crucial role in the medical community in India, advocating for the rights of doctors and patients, promoting medical education, and ensuring the delivery of quality healthcare services.
Sharing his achievement on a social media platform Linkedin, Dr Venkatesh said, “Glad to share that I have been appointed as the National Convenor of IMA Standing Committee for Antimicrobial Resistance.
Special thanks to Dr R V Asokan sir, Dr Anilkumar Nayak sir, Dr Shitij Bali sir, Dr Narendra Saini sir, Dr Abul Hasan sir, Dr Hariharan sir and all leaders of IMA for the opportunity. Thankful to Prof (Dr) CM Singh sir, Prof (Dr) Sanjay Pandey sir and my department.”
Also read- New Principal, Medical Superintendent Appointed At SMS Medical College Hospital
Powered by WPeMatico

Regular use of fish oil supplements might increase, rather than lessen, the risk of first time heart disease and stroke among those in good cardiovascular health, but may slow progression of existing poor cardiovascular health and lower the risk of death, suggest the results of a large long term study, published in the open access journal BMJ Medicine.
Fish oil is a rich source of omega 3 fatty acids, and as such, is recommended as a dietary preventive to ward off the development of cardiovascular disease. But the evidence on how much protection it affords is inconclusive, explain the researchers.
To strengthen the evidence base, they set out to estimate the associations between fish oil supplements and new cases of atrial fibrillation; heart attack, stroke, and heart failure; and death from any cause in those with no known cardiovascular disease.
And they assessed the potential role of these supplements on the risk of progressing from good heart health (primary stage), to atrial fibrillation (secondary stage), to major cardiovascular events, such as a heart attack (tertiary stage), and death (end stage).
They drew on 415,737 UK Biobank study participants (55% women), aged 40-69, who were surveyed between 2006 and 2010 to gather basic background information. This included their usual dietary intake of oily and non-oily fish and fish oil supplements.
The participants’ health was tracked until the end of March 2021 or death, whichever came first, using medical records data.
Nearly a third (130,365; 31.5%) of the participants said they regularly used fish oil supplements. This group included higher proportions of older and White people, and women. Alcohol intake and the ratio of oily to non-oily fish eaten were also higher, while the proportions of current smokers and those living in deprived areas were lower.
During an average monitoring period of nearly 12 years, 18,367 participants developed atrial fibrillation, 22,636 had a heart attack/stroke or developed heart failure, and 22,140 died-14,902 without atrial fibrillation or serious cardiovascular disease.
Among those who progressed from good cardiovascular health to atrial fibrillation, 3085 developed heart failure, 1180 had a stroke, and 1415 a heart attack. And 2436 of those with heart failure died, as did 2088 of those who had had a stroke, and 2098 of those who had had a heart attack.
Regular use of fish oil supplements had different roles in cardiovascular health, disease progression, and death, the findings indicated.
For those with no known cardiovascular disease at the start of the monitoring period, regular use of fish oil supplements was associated with a 13% heightened risk of developing atrial fibrillation and a 5% heightened risk of having a stroke.
But among those who had cardiovascular disease at the start of the monitoring period, regular use of fish oil supplements was associated with a 15% lower risk of progressing from atrial fibrillation to a heart attack, and a 9% lower risk of progressing from heart failure to death.
Further in-depth analysis revealed that age, sex, smoking, consumption of non-oily fish, high blood pressure, and use of statins and blood pressure lowering drugs changed the associations observed.
Regular use of fish oil supplements and the risk of transitioning from good health to heart attack, stroke, or heart failure was 6% higher in women and 6% higher in non-smokers. And the protective effect of these supplements on the transition from good health to death was greater in men (7% lower risk) and older participants (11% lower risk).
As this is an observational study, no conclusions can be drawn about causal factors, acknowledge the researchers. And no potentially influential information was available on either dose or formulation of the fish oil supplements. And given that most of the participants were White, the findings might not be applicable to people of other ethnicities, they add.
But they conclude: “Regular use of fish oil supplements might have different roles in the progression of cardiovascular disease. Further studies are needed to determine the precise mechanisms for the development and prognosis of cardiovascular disease events with regular use of fish oil supplements.”
Reference:
Chen G, Qian Z(, Zhang J, et alRegular use of fish oil supplements and course of cardiovascular diseases: prospective cohort studyBMJ Medicine 2024;3:e000451. doi: 10.1136/bmjmed-2022-000451.
Powered by WPeMatico
Jane Freeston et al conducted a study to develop a novel whole-body MRI protocol capable of assessing inflammatory arthritis at an early stage in multiple joints in one examination.
Forty-six patients with inflammatory joint symptoms and 9 healthy volunteers underwent whole-body MR imaging on a 3.0 T MRI scanner in this prospective study. Image quality and pathology in each joint, bursae, entheses and tendons were scored by two of three radiologists and compared to clinical joint scores. Participants were divided into three groups based on diagnosis at 1-year follow-up (healthy volunteers, rheumatoid arthritis and all other types of arthritis). Radiology scores were compared between the three groups using a Kruskal-Wallis test. The clinical utility of radiology scoring was compared to clinical scoring using ROC analysis.
Key findings of the study:
• Fifty-five participants were included in this study comprising 18 patients with RA (10 cyclic citrullinated peptide (CCP) negative RA patients and 8 CCP positive RA patients), 28 patients with non-RA and 9 HC’s. The non RA group consisted of the following subtypes: 10 persistent undifferentiated arthritis (pUA), 8 resolved undifferentiated arthritis (rUA), 5 spondyloarthritis (SpA), 4 undifferentiated arthritis and 1 crystal arthritis.
• A protocol capable of whole-body MR imaging of the joints with an image acquisition time under 20 min was developed with excellent image quality.
• Synovitis scores were significantly higher in patients who were diagnosed with rheumatoid arthritis at 12 months (p < 0.05).
• Radiology scoring of bursitis showed statistically significant differences between each of the three groups—healthy control, rheumatoid arthritis and non-rheumatoid arthritis (p < 0.05).
• There was no statistically significant difference in ROC analysis between MRI and clinical scores.
The authors concluded –
“In summary, this whole-body multi-joint MRI technique is feasible to use in a clinical setting and produces good quality images. It has the potential to differentiate between RA, non-RA and HC at early presentation. It is potentially useful in identifying disease “load”, including sub-clinical disease and extra-articular inflammation. The technique is transferrable to other MRI scanners and to other patient cohorts where assessment of global joint-based disease is desirable.”
Further reading:
Whole body MRI for the investigation of joint involvement in inflammatory arthritis
Jane Freeston et al
Skeletal Radiology (2024) 53:935–945
https://doi.org/10.1007/s00256-023-04515-0
Powered by WPeMatico

Perinatal mood and anxiety disorders are among the most common complications that occur in pregnancy or in the first 12 months after delivery. Despite the negative effects on maternal, obstetric, birth, offspring, partner, and family outcomes, perinatal mental health disorders often remain underdiagnosed, and untreated or under-treated.Also COVID-19 infection and immunization has exhibited varied effects on maternal mortality.
American College of American College of Obstetricians and Gynecologists has issued Statement on New Data Showing Effect of COVID-19 and Mental Health on Maternal mortality.
Dr. M Christopher Zahn, MD, FACOG, interim CEO and chief of clinical practice and health equity and quality for the American College of Obstetricians and Gynecologists has stated that:
“The latest CDC data provide a closer look at how the tremendous disruption that COVID-19 created within the health care system worsened maternal health outcomes at the start of the pandemic. They also highlight the extent to which COVID-19 disproportionately affected certain racial groups-particularly Black and American Indian or Alaska Native pregnant and postpartum people, who faced elevated rates of maternal mortality. We anticipated at the beginning of the pandemic that social determinants of health would play a large role in determining which groups would suffer more harm from COVID-19 prior to vaccine availability, especially with regard to pregnant individuals, who are at increased risk of severe complications and death from COVID-19; the data bear this out. The tragic disparities in outcomes among racial groups also demonstrates just how important the COVID-19 vaccines were in mitigating those inequities.
“While there continue to be competing data sources on maternal mortality, the consistencies among similar trends in the data shine a light on where we can and must make inroads. We are still seeing nearly 50% of maternal deaths occurring between seven days and one year postpartum, with more than 80% of those deaths considered preventable.
“One area in which we can move the needle in addressing preventable maternal deaths is mental health, as mental health conditions continue to be a leading cause of deaths. The new data reinforce the need for obstetric care clinicians to have the skill set necessary to address perinatal mental health conditions. Although obstetrician–gynecologists are not trained to treat all mental health conditions that can occur in the perinatal period, they can successfully address the overall issue of perinatal mental health in their patients with the proper guidance and resources.
“ACOG and others in the maternal heath space have done a lot of work to create clinical guidance and implementation tools on perinatal mental health and other conditions to empower clinicians to improve maternal health outcomes in their practices every day, but our focus needs to be on sustainability. We cannot afford to lose any ground.”
Powered by WPeMatico
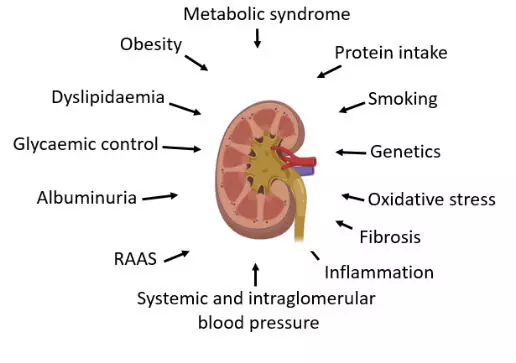
Dietary interventions and salt restriction may significantly improve clinical outcomes in patients with diabetic nephropathy suggests a study published in the Frontiers in Endocrinology.
A study evaluated the quality of evidence, potential biases, and validity of all available studies on dietary intervention and diabetic nephropathy (DN). They conducted an umbrella review of existing meta-analyses of randomized controlled trials (RCTs) that focused on the effects of dietary intervention on DN incidence. The literature was searched via PubMed, Embase, Web of Science, and the Cochrane Database of Systematic Reviews. According to the Grading of Recommendations, Assessment, Development and Evaluation (GRADE), evidence of each outcome was evaluated and graded as “high”, “moderate”, “low” or “very low” quality to draw conclusions. Additionally, we classified evidence of outcomes into 4 categories. They identified 36 meta-analyses of RCTs and 55 clinical outcomes of DN from 395 unique articles. Moderate-quality evidence suggested that probiotic supplementation could significantly improve blood urea nitrogen (BUN), total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) levels in DN patients. Low-quality evidence indicated that probiotic supplementation significantly improved the serum creatinine concentration, urinary albumin–creatinine ratio (UACR), fasting blood glucose (FBG), HbA1c and high-density lipoprotein cholesterol (HDL-C) in DN patients. In addition, low-quality evidence suggested that a salt restriction diet could significantly improve the creatinine clearance rate (CrCl) in patients with DN. Low-quality evidence suggested that vitamin D supplementation could significantly improve the UACR in patients with DN. In addition, low-quality evidence has indicated that soy isoflavone supplementation could significantly improve BUN, FBG, total cholesterol (TC), triglyceride (TG) and LDL-C levels in patients with DN. Furthermore, low-quality evidence suggested that coenzyme Q10 supplementation could significantly improve HbA1c, TC and HDL-C in patients with DN, and dietary polyphenols also significantly improved HbA1c in patients with DN. Finally, low-quality evidence suggested that supplementation with antioxidant vitamins could significantly improve the serum creatinine concentration, systolic blood pressure, and HbA1c level in patients with DN. Given the small sample size, all significantly associated outcomes were evaluated as class IV evidence. Moderate to low amounts of evidence suggest that supplementation with probiotics, vitamin D, soy isoflavones, coenzyme Q10, dietary polyphenols, antioxidant vitamins, or salt-restricted diets may significantly improve clinical outcomes in patients with DN.
Reference:
Cai L, Huang Y, Li X, Cao D, Liu F. Effects of dietary intervention on diabetic nephropathy: an umbrella review of systematic reviews and meta-analyses of randomized controlled trials. Front Endocrinol (Lausanne). 2024 Apr 29;15:1385872. doi: 10.3389/fendo.2024.1385872. PMID: 38742202; PMCID: PMC11089238.
Keywords:
Dietary, interventions, salt restriction, significantly, improve, clinical, outcomes, patients, diabetic nephropathy, study, Frontiers in Endocrinology, diets, DN, umbrella review, meta-analysis, systematic review
Powered by WPeMatico

Vijayawada: A Non-Resident Indian (NRI) Gastroenterologist, Dr Uyyuru Lokesh Kumar who holds American Citizenship was taken into police custody after security personnel at Gannavaram airport on Sunday found him carrying a satellite phone in his baggage.
During the check-in process for his flight to Delhi, which was part of his journey back to the United States, the security personnel became suspicious of him when he was wandering in the airport following which they interrogated him and found that Dr Lokesh did not have required permission to use the satellite phone.
In India, possession and use of satellite phones require authorization from the appropriate government department as the use of Satellite Phones is unauthorised/illegal in India under Section 6 of the India Wireless Act and Section 20 of the Indian Telegraph Act.
The government strictly banned the use of satellite phones in the country and instructed all foreigners or travellers to not carry such phones in India. If found, then the person would be detained/confiscated and the passenger can be penalised under the abovementioned section of the Indian Telegraph Act.
Upon discovering the unauthorized satellite phone, airport security handed him over to the Gannavaram police. Dr Lokesh explained to the police that he had purchased the phone in Virginia and brought it with him to India without knowing the regulations.
After being detained, Dr Lokesh was released on the condition that he would cooperate with the ongoing investigation. The police have stated that carrying a satellite phone through domestic airports without proper authorization is against Indian regulations, TOI reports.
Hence, they are considering registering a case against Dr Lokesh after seeking legal advice. Following his release, Dr Lokesh took a flight to Delhi from where he had a connecting flight to the US.
According to the Deccan Chronicle news reports, Lokesh, who belongs to Venkatayapalem of Thullur mandal of Amaravati in Guntur district, went to America and settled there by getting US citizenship. He worked as a gastroenterologist in Richmond; he worked there for 38 years, and his license was reportedly cancelled by the local authorities due to a violation of norms.
Earlier, he was taken into preventive custody at Gannavaram airport for exhibiting “suspicious behaviour” while Chief Minister YS Jagan Mohan Reddy was about to board a flight to London on Friday night. It was found that Dr Lokesh sent messages to the TDP cadre for a protest call while the CM was at the airport but no one turned up.
Powered by WPeMatico
Researchers have found that identifying symptomatic individuals with undiagnosed asthma and chronic obstructive pulmonary disease (COPD) and linking them with specialty care significantly reduces healthcare utilization and symptom burden. This finding stems from a randomized trial conducted in Canada, which highlights the benefits of early diagnosis and pulmonologist-directed care. This trial was published in The New England Journal Of Medicine by Aaron SD. and colleagues.
Undiagnosed respiratory diseases such as asthma and COPD are common in the community, often leading to poor quality of life and increased healthcare utilization. Early diagnosis and appropriate treatment can mitigate disease progression and reduce acute care needs. The Undiagnosed COPD and Asthma Population (UCAP) Study aimed to assess the impact of specialist care on healthcare utilization and symptom management in patients with newly diagnosed asthma or COPD.
The UCAP trial involved over a million households near 17 trial sites in Canada, screened through automated telephone calls to identify individuals with respiratory symptoms. Ultimately, 508 adults with newly diagnosed COPD (n=258) or asthma (n=250) were randomized to receive pulmonologist-directed care or usual care with a primary care provider. Participants were followed for one year, and primary outcomes included the annualized rate of healthcare utilization for respiratory illness. Secondary outcomes focused on disease-specific quality of life, symptom burden, and lung function.
Intervention group had 0.53 vs. 1.12 events per person-year (IRR 0.48, 95% CI 0.36-0.63, P<0.001).
Significant reduction in primary care visits (0.36 vs. 0.91 per person-year; IRR 0.39, 95% CI 0.29-0.53).
SGRQ total score improvement of -3.5 points (95% CI -6.0 to -0.9).
CAT total score improvement of -1.3 points (95% CI -2.4 to -0.1).
Pre-bronchodilator FEV1 improvement of 94 ml (95% CI 50-138).
92% of the intervention group vs. 60% of the usual-care group started new asthma or COPD medications.
14% of active smokers in the intervention group quit smoking vs. 7% in the usual care group.
The findings indicate that specialized care significantly reduces healthcare utilization and improves quality of life and lung function in patients with newly diagnosed asthma or COPD. Participants in the intervention group benefited from guideline-based treatment, including medication prescriptions, disease education, behavioral counseling, and recommendations for vaccinations and smoking cessation.
The study revealed some limitations, including potential biases due to the requirement for a registered telephone number and the higher willingness of older adults to participate. The approach may also be less feasible in healthcare systems with limited access to specialty care. Despite these challenges, the results emphasize the potential benefits of early diagnosis and specialized care in managing asthma and COPD.
The UCAP trial demonstrates that linking symptomatic individuals with undiagnosed asthma or COPD to pulmonologist-directed care significantly reduces healthcare utilization and improves disease-specific outcomes. This study highlights the need for effective case-finding strategies and specialized care to enhance the management of respiratory diseases in the community.
Reference:
Aaron, S. D., Vandemheen, K. L., Whitmore, G. A., Bergeron, C., Boulet, L.-P., Côté, A., McIvor, R. A., Penz, E., Field, S. K., Lemière, C., Mayers, I., Bhutani, M., Azher, T., Lougheed, M. D., Gupta, S., Ezer, N., Licskai, C. J., Hernandez, P., Ainslie, M., … Mulpuru, S. (2024). Early diagnosis and treatment of COPD and asthma — A randomized, controlled trial. The New England Journal of Medicine. https://doi.org/10.1056/nejmoa2401389
Powered by WPeMatico
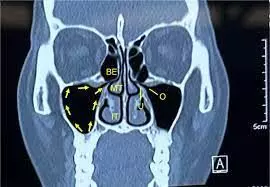
Maxillary MRONJ patients benefit from sinus evaluation and concurrent surgical intervention suggests a study published in the Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.
Maxillary sinusitis can be a sequela of medication-related osteonecrosis of the jaw (MRONJ). This study aims to characterize the microbiome of maxillary MRONJ with concurrent maxillary sinusitis and radiographic maxillary sinus opacification to determine if there is a relationship between the microbiome of MRONJ and sinus disease. This retrospective case series was conducted using electronic health records from the University of Pennsylvania and affiliated hospitals. The target population was surgically managed maxillary MRONJ patients. The primary predictor variables were tissue culture results. The primary outcomes were maxillary sinusitis or maxillary sinus opacification. Statistical analysis was performed using chi-squared tests at the 95% confidence interval. Results: Thirty-nine subjects were selected: 25 had sinus opacification and 11 had sinusitis. Resident bacteria were present in 90% of subjects, nonresident bacteria in 74%, and opportunistic organisms in 15%. There were significantly more subjects with chronic sinusitis microbes (79%) than without. There were significantly more gram-positive anaerobes, specifically Propionibacterium, as well as the gram-negative facultative anaerobe, Capnocytophaga, in subjects with concurrent sinusitis.Maxillary MRONJ with concurrent maxillary sinusitis may be associated with gram-positive anaerobic species, Propionibacterium, and Capnocytophaga colonization. Maxillary MRONJ patients may benefit from sinus evaluation and concurrent surgical intervention.
Reference:
Hershberger MW, He P, Francois K, Lerner D, Bear A, Adappa N, Panchal N. Is maxillary sinusitis and radiographic maxillary sinus opacification associated with an altered microbiology of MRONJ? Oral Surg Oral Med Oral Pathol Oral Radiol. 2024 Apr;137(4):345-354. doi: 10.1016/j.oooo.2023.12.003. Epub 2023 Dec 9. PMID: 38443234.
Keywords:
Maxillary, patients, benefit, sinus evaluation, concurrent, surgical intervention, study, Hershberger MW, He P, Francois K, Lerner D, Bear A, Adappa N, Panchal N, Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology
Powered by WPeMatico
