Unveiling Other Side of coin: linking SGLT2 Inhibitors to Euglycemic Diabetic Ketoacidosis
India: In a startling revelation, a recent case study has brought to light an uncommon yet potentially life-threatening complication associated with Sodium-Glucose Cotransporter 2 (SGLT2) inhibitors, raising concerns within the medical community. The study emphasizes the importance of vigilance in monitoring patients receiving these medications.
SGLT2 inhibitors, hailed for their efficacy in managing type 2 diabetes by promoting urinary glucose excretion, have gained widespread acceptance in clinical practice. However, emerging evidence suggests a rare but severe adverse effect – euglycemic diabetic ketoacidosis (EDKA), characterized by ketoacidosis with blood glucose levels within the normal or mildly elevated range. With their increasing use in the management of type 2 diabetes mellitus due to long-term beneficial effects, there is a rise in the incidence of this complication.
The recent case, published in Cureus, signifies the importance of awareness of the link between the SGLT2 inhibitors use and EDKA and early recognition of this complication to reduce mortality and morbidity. Furthermore, it also emphasizes the need for clinicians to educate their patients taking these drugs to prevent them during the intercurrent illness to prevent them from developing EDKA.
Sangita D. Kamath, Internal Medicine, Tata Main Hospital, Jamshedpur, IND, and colleagues report the case of a 58-year-old lady with a history of type 2 diabetes mellitus (T2DM) on multiple anti-diabetes medications, including dapagliflozin for one year, who during intercurrent illness developed EDKA.
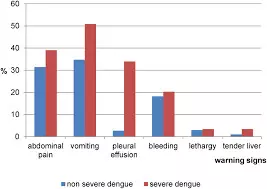
Her blood sugar on admission was 203 mg/dL, and arterial blood gas showed high anion-gap metabolic acidosis (HAGMA) with ketonemia (blood beta-hydroxybutyric (BOHB) acid level: 5.4 mmol/L) and ketonuria. This condition may have been precipitated by dehydration resulting from repeated vomiting, low carbohydrate intake, and skipping the previous two days’ dose of insulin.
She was treated with intravenous fluids, insulin, 5% dextrose infusion, and potassium supplements with complete resolution of acidosis after about 90 hours.
In conclusion, the case report adds to the existing evidence in the literature supporting the relationship between SGLT2 inhibitors use and EDKA.
“Diagnosing this condition without high blood glucose levels may be challenging, as seen in typical DKA. It is imperative to check ketone body and blood gas levels in patients on SGLT2 inhibitors as the diagnosis cannot be excluded based on blood glucose levels alone,” the researchers wrote. This dreaded complication may be excluded by unexplained HAGMA even in the setting of normal levels of blood glucose.
The report also highlights the importance of patient education on the “sick-day rules” before starting this class of drugs. Clinicians should have a high index of suspicion for detecting this complication early and avoid delay in treatment.
Reference:
Kamath S D, Kumar U, Shrivastava V (April 15, 2024) Sodium-Glucose Cotransporter 2 Inhibitor-Induced Euglycemic Diabetic Ketoacidosis: The Other Side of the Coin!. Cureus 16(4): e58341. doi:10.7759/cureus.58341
Powered by WPeMatico