Good evidence confuses ChatGPT when used for health information, study finds
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Chennai: Taking cognizance of the complaints from students alleging poor teaching quality, the Directorate of Medical Education in Tamil Nadu has instructed the faculties of the 11 new medical colleges in the State to focus on improving the teaching quality at the medical colleges.
Directions have also been issued to the deans of the concerned new medical colleges to monitor the quality of teaching at the institutes, DT Next has reported.
This comes after the students from the new medical colleges recently raised a complaint to the Health Secretary Gagandeep Singh Bedi alleging poor teaching quality.
The State Health Department set up a panel to look into the issue and new instructions have been issued to the professors and deans of the medical colleges regarding the same.
Commenting on the matter, the Director of Medical Education Dr. J Sangumani told the DT Next, “The deans appointed to all the new medical colleges have been asked to undertake the supervision of the teaching in the college. Any complaints by the students will also be taken seriously. The professors have been instructed to ensure that students do not face any academic pressure and are given due attention.”
As per the Daily, the students alleged that they had to depend on online lectures as the classes were not held properly and they were conveyed mainly as presentations. It was also alleged that the mode of conducting the class was confusing for the students as the staff used to take classes in English and Tamil, thereby making it difficult for the students to understand.
They also raised concerns regarding a lack of transparency in the attendance system by the teachers. Responding to this, the officials from DME informed that the deans of the respective medical colleges and the directorate authorities will monitor the attendance.
The Health Department authorities have taken serious note of these allegations regarding the teaching quality in the medical colleges in Tamil Nadu, especially considering the speculations that the State Government would request more new medical colleges.
Medical Dialogues had earlier reported that with the deferment of the National Medical Commission’s (NMC) rule of capping the total number of MBBS seats in a particular State/UT, the State Health Department of Tamil Nadu was planning to apply for new medical colleges in the State.
Aiming to ensure that there are at least one new medical college in every district, it was being speculated that the State Government would soon apply for new colleges at Tenkasi, Mayiladuthurai, Tirupathur, Perambalur, Ranipet, Kancheepuram, and Kallakurichi.
Also Read: As NMC defers MBBS seat cap rule, Tamil Nadu to Apply for New Medical Colleges
Powered by WPeMatico

New Delhi: In a remarkable medical achievement, doctors at a city hospital successfully conducted a rare combined liver and kidney transplant on a critically ill 46-year-old patient from Uzbekistan. The complex surgery, which lasted 16 hours, utilized organs donated by the patient’s wife and daughter, marking a significant milestone in modern medicine.
Combined organ transplants are rare and challenging and underscore the remarkable feats achievable in modern medicine, doctors said.
According to a PTI report, The patient presented with the history of recurrent ascites (water in tummy), needing multiple admission for draining the water. When he visited Max Hospital, Vaishali, upon evaluation it was found that he had a liver cirrhosis as well as a non-functioning kidney, the hospital said in a statement.
The patient was suffering from advanced kidney failure and both of his kidneys put together were functioning less than 20 per cent of normal.
“The patient, Akhrorjon Khaydarov, already knew about his liver condition but he was shocked when he found about his kidney failure as well. He was anxious and worried. However, we counselled and informed him about possibility of combined liver and kidney transplant. A kidney transplant was likely to contribute to better functioning of the liver transplant as well and thereby save his life,” said Dr Neeru Aggarwal, Principal Director, Nephrology, Max Hospital, Vaishali.
The patient’s daughter donated a part of her liver for the transplant, while the kidney was donated by his wife. The surgery took place last month.
Sharing details about the combined transplant, Dr Subhash Gupta, Chairman, Centre for Liver and Biliary Sciences at the hospital, said that traditionally such cases involve separate surgeries for each organ, with the liver transplant preceding the kidney transplant.
“However, the medical team at Max Hospital, Vaishali, opted for simultaneous surgery on the same operating table, showcasing their expertise and innovation in the field of transplantation,” Dr Gupta said.
Dr Anant Kumar, Chairman – Urology, Kidney Transplant and Robotics at Max Super Speciality Hospital, said the intricate procedures took place in the specialised transplant operating theatre, equipped with three interconnected operating rooms –one for liver donor, one for kidney donor and one for the recipient, news agency PTI reported.
A total of nine highly skilled doctors, including teams from the liver and kidney transplant departments, collaborated seamlessly to ensure the success of the surgeries.
The surgery posed several challenges for the doctors given the prolonged hours and readiness for dialysis during surgery, said Dr Rajesh Dey, Associate Director, Liver and Biliary Sciences at the hospital.
However, we could provide best outcome for the patient with meticulous planning, unwavering focus and collective skill of the multi-disciplinary team, he said.
Following a successful recovery, the patient has been discharged and is set to return to his home country, marking a triumphant conclusion to his journey towards renewed health and vitality.
Also Read:Nanavati Max super-speciality Hospital inaugurates liver transplant support group
Powered by WPeMatico
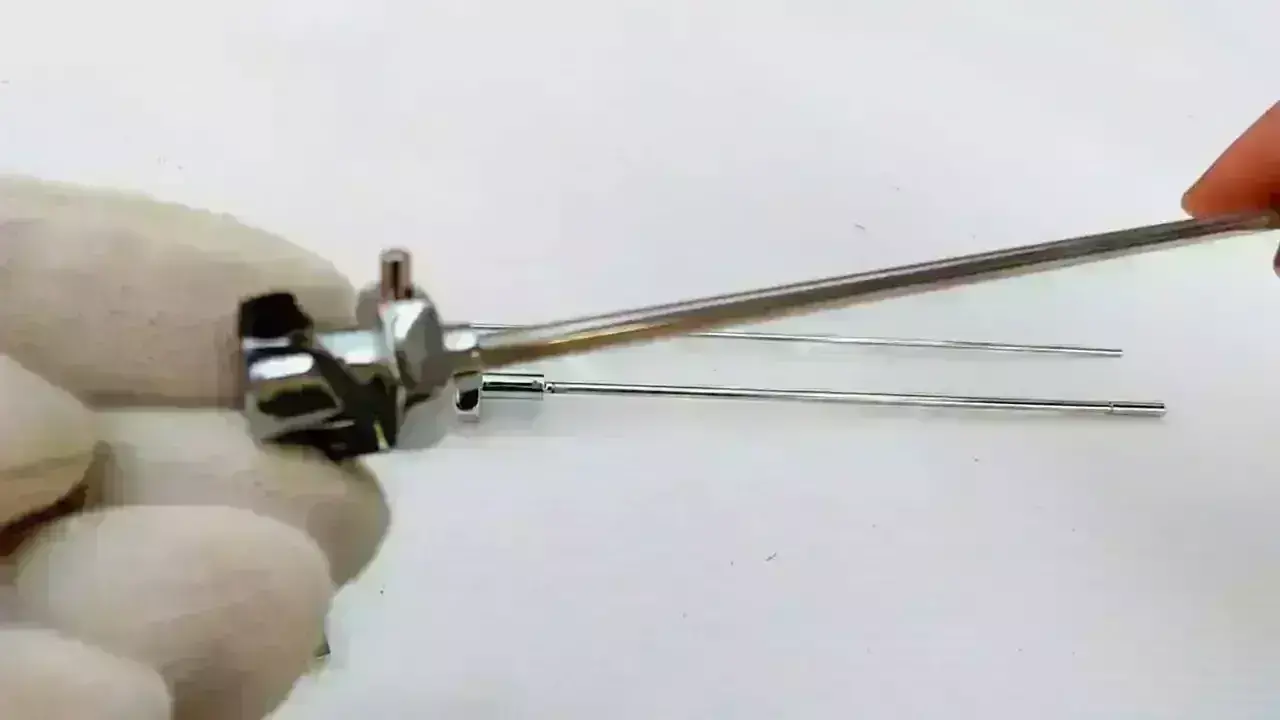
Researchers have found in a small randomized controlled trial that an initial image-assisted Abrams needle biopsy (IA-ANPB) can match medical thoracoscopy (MT) to diagnose people with pleural effusion.
Image-guided or assisted needle biopsies and the increasing use of medical thoracoscopy (MT) have significantly increased the diagnostic accuracy of pleural diseases. However, there is no consensus on which patients should undergo medical thoracoscopy (MT) and which patient should undergo image-guided or assisted needle biopsy as the first procedure to ensure greater diagnostic accuracy in patients with pleural effusion. This prospective, randomized, parallel study included two hundred twenty-eight patients with undiagnosed exudative pleural effusion. Patients were divided into two groups based on computed tomography (CT) findings. Group 1: patients with pleural effusion only; Group 2: patients with pleural thickening or lesion in addition to pleural effusion. Patients in each group were randomly assigned to an image- assisted Abrams needle biopsy (IA-ANPB) or MT arm. The diagnostic sensitivity, reliability, and safety were determined for both groups.
RESULTS: The false negativity rate was 30.3% for the IA-ANPB arm and 3.1% for the MT arm in Group 1. The same rates were 11.9% for IA-ANPB and 4.7% for MT in Group 2. In Group 1, the sensitivity for the IA-ANPB arm was 69.7%, negative likelihood ratio of 0.30. The same rates for the MT arm were 96.9% and 0.03 (p=0.009). In Group 2, these values were 88.1% and 0.12 for the IA-ANPB arm and 95.4% and 0.05 for the MT arm (p=0.207). The rate of complications between the two biopsy methods was not different (8.5% and 15.8%, respectively; p=0.107). MT showed a high diagnostic success in all patients with pleural fluid. On the other hand, IA-ANPB showed similar diagnostic success as MT in patients with pleural effusion and associated pleural thickening/lesions. Therefore, in the latter case, IA-ANPB could be preferable before MT.
Reference:
IMAGE-ASSISTED PLEURAL NEEDLE BIOPSY OR MEDICAL THORACOSCOPY: WHICH METHOD FOR WHICH PATIENT? A RANDOMIZED CONTROLLED TRIAL Muzaffer Metintas, MD Guntulu Ak, MD, PhD Huseyin Yildirim, MD Fusun Alatas, MD Senay Yilmaz, MD Selma Metintas, MD, PhD Show all authors Published:March 28, 2024 DOI:https://doi.org/10.1016/j.chest.2024.03.038
Powered by WPeMatico

Geneva: The World Health Organization (WHO) released new guidelines on the prevention, diagnosis, and treatment of chronic hepatitis B (HBV) infection at the 2024 Asian Pacific Conference for the Study of Liver Disease (APASL) in Kyoto, Japan.
The 2024 HBV guidelines provide updated evidence-informed recommendations on key priority topics. These include substantial simplification and expansion of eligibility for treatment to overcome barriers to access to HBV testing and treatment.
The 2024 guidelines include 11 updated chapters with new recommendations and also update existing chapters without new recommendations, such as those on treatment monitoring and surveillance for liver cancer.
More than 250 million people are affected by chronic hepatitis B infection, leading to increasing deaths each year. Most of the global burden of chronic hepatitis B (CHB) is due to mother-to-child transmission at or shortly after birth. WHO’s Global health sector strategy sets actions and targets to eliminate viral hepatitis by 2030 by driving new infections and deaths down to half a million each globally – a reduction of 90% and 65%, respectively.
There has been considerable progress in eliminating mother-to-child transmission of HBV through universal HBV immunization, including the timely hepatitis B birth dose. However, hepatitis B birth-dose coverage is only 45% globally, with less than 20% coverage in the WHO African Region.
For patients with CHB infection, antiviral treatment is highly effective. It can reduce the progression of liver disease and improve survival and liver cancer development. However, major testing and treatment gaps remain.
HBV infection is a major public health problem and cause of chronic liver disease. The new guidelines provide updated evidence-based recommendations on the priority HBV-related topics from the 2015 WHO Guidelines for the care and treatment of patients diagnosed with chronic hepatitis B infection and the 2017 WHO Guidelines on hepatitis B and C testing. These priority areas are:
The recommendations include expanded and simplified treatment criteria for adults but now also for adolescents; expanded eligibility for antiviral prophylaxis for pregnant women to prevent mother-to-child transmission of HBV; improving HBV diagnostics through use of point-of-care HBV DNA viral load and reflex approaches to HBV DNA testing; who to test and how to test for HDV infection; and approaches to promote delivery of high-quality HBV services, including strategies to promote the adherence to long-term antiviral therapy and retention in care.
These guidelines also update existing chapters without new recommendations, such as those on treatment monitoring and surveillance for liver cancer.
Powered by WPeMatico
Iron plays a vital role in the growth and development of young children. In low- and middle-income countries, anaemia is a significant health issue, and young children are vulnerable to iron deficiency anaemia. Previous research studies have shown the association between low iron and poor development outcomes in children.
Powered by WPeMatico
South Korea: A recent study published in the Journal of Clinical Medicine has shed light on the potential application of non-invasive optical imaging methods in orthodontic diagnosis.
Jae Ho Baek from F.E.S. Research Lab in Ulsan, Republic of Korea, found that non-invasive optical diagnostic devices, including optical Doppler tomography (ODT) and optical coherence tomography (OCT), can be used in clinical practice during orthodontic treatment. They also introduced a new diagnostic paradigm differentiating microstructural changes in tissues in orthodontic diagnosis.
The investigator notes the importance of the early diagnosis of microscopic changes in soft and hard tissues, including periodontal tissue during orthodontic treatment to prevent iatrogenic side effects like periodontal diseases and root resorption. Cervical periodontal tissue is suggested to be the most critical area that reacts first to orthodontic forces or mal-habits, and it is also the place of bacteria deposition in the early stage of periodontal diseases.
The early diagnosis of hard tissue changes, such as demineralization is also essential in maintaining a patient’s health during orthodontic treatment. Many diagnostic devices, including radiographic equipment and intra-oral scanners, help diagnose these problems but have certain limitations in precision and invasiveness.
Against the above background, the study was conducted to verify the possible utilities of non-invasive diagnostic devices in the orthodontic field that can compensate for these limitations.
For this purpose, non-invasive optical diagnostic devices were used in vivo with human and animal examinations for soft and hard tissues, including optical Doppler and coherence tomography. These devices can provide real-time three-dimensional images at the histological scale.
In conclusion, optical diagnostic imaging devices have sufficient objective potential for diagnosing soft tissue, including periodontal tissue and hard tissue, in orthodontics. In addition to solving some technical problems, the study results open a new horizon in orthodontic diagnosis through ongoing research to understand the correlation between changes in periodontal tissue and tooth movements during orthodontic treatment or pathologic progress.
The investigator found ODT and OCT can provide two-dimensional or three-dimensional images of hard tissue and periodontal changes during orthodontic treatment at the histological level non-invasively in both animal experiments and humans in vivo.
Specifically, it was found that these devices can be used during orthodontic treatment in several areas, such as estimating microscopic changes in periodontal tissue, which are essential to evaluate biomechanical effects, enamel demineralization, and the early diagnosis of periodontal diseases.
“It is a task that must be solved in the future to collect more data by applying these devices to orthodontic patients with removable or fixed appliances and then verifying the correlation between the results and existing information to establish standards for objective data analysis,” the study stated.
Reference:
Baek, J. H. (2023). Potential Application of Non-Invasive Optical Imaging Methods in Orthodontic Diagnosis. Journal of Clinical Medicine, 13(4), 966. https://doi.org/10.3390/jcm13040966
Powered by WPeMatico

University of New Mexico researchers have found that even low to moderate alcohol use by pregnant patients may contribute to subtle changes in their babies’ prenatal development, including lower birth length and a shorter duration of gestation.
In a new paper published in the journal Alcohol Clinical & Experimental Research, a team led by Ludmila Bakhireva, MD, PhD, MPH, professor and assistant dean for Clinical and Translational Research in the UNM College of Pharmacy, also reported some sex-related differences in the effects of drinking during pregnancy on the developing baby.
“In exploratory analyses, the effect on gestational age was more pronounced in male infants, and for birth length it actually was stronger in females,” Bakhireva said. She cautioned that these effects should be interpreted with caution because of the study’s limited statistical power to conduct sex-specific analyses and the challenges of accounting for other contributing factors.
The paper reported on three prospective studies conducted at UNM over the course of 10 years that followed 281 participants, most of whom were recruited in the second trimester of their pregnancies and then followed, along with their children, for some time afterward, she said.
There is a good deal of research on the prenatal effects of heavy alcohol use, usually defined as 14 drinks per week, or binge drinking, defined as four drinks or more per occasion, Bakhireva said.
“We know quite a bit from these earlier studies of heavy alcohol use about the effect on prenatal outcomes, especially preterm delivery and growth restriction, as well as neurodevelopmental outcomes, but we specifically focused on more moderate alcohol exposure because it’s much more prevalent,” she said.
Early pregnancy is a critical period for the formation of organs in the developing fetus, making it a particularly vulnerable window for alcohol exposure, Bakhireva said.
“Almost everybody drinks before they know they are pregnant, and risky drinking before pregnancy is predictive of drinking later on,” she said. “That’s a unique aspect of the study. We carefully looked at the patterns of drinking around conception and early pregnancy.”
Most of the participants substantially reduced their drinking or stopped altogether once they learned they were pregnant, Bakhireva said. Even with reduced alcohol there were some deficits seen in both male and female infants, however.
She emphasizes that larger studies that combine samples across the country are needed to replicate the findings and examine sex-specific effects further.
Bakhireva is the principal investigator of the HEALthy Brain and Child Development study at UNM, part of a national initiative that will recruit 7,500 parent-child pairs and follow them for up to 10 years. “With that type of multi-site study, we’ll have sufficient power to look at the effects of different patterns and timing of alcohol use in even a more nuanced way,” she said.
The paper underscores messaging from the National Institute of Alcohol Abuse and Alcoholism-that no amount of drinking during pregnancy is safe, she said.
“I think this study, as well as prior preclinical studies, show that even moderate alcohol use might have negative effects. The degree of negative effects might vary, and it is important to address alcohol use without the stigma often associated with it, but overall, if we try to encourage abstinence from alcohol during pregnancy, we will maximize positive health and developmental outcomes for the children.”
Reference:
Ludmila N. Bakhireva, Xingya Ma, Alexandria Wiesel, Fiona E. Wohrer, Jared DiDomenico, Sandra W. Jacobson, Melissa H. Roberts, Dose–response effect of prenatal alcohol exposure on perinatal outcomes, Alcohol Clinical and Experimental Research, https://doi.org/10.1111/acer.15284.
Powered by WPeMatico
