Why some adults may need another dose of measles vaccine
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Pune: The authorities of B J Medical College (BJMC) and Sassoon General Hospital (SGH) have initiated a probe into the ragging complaint filed by a 24-year-old junior resident doctor.
According to a recent report by HT, officials were informed about the incident after the Junior Resident Doctor, studying in her first year of Doctor of Medicine course in Anaesthesia, complained to the college administration in this regard. As per her complaint, she was allegedly ragged and bullied by seniors while working in the department.
Taking note of her complaint, the BJMC authorities initiated a probe into the incident. Officials have informed the Daily that the matter is being probed by the post-graduate (PG) grievance redressal committee, which will submit a report in this regard.
Commenting on the development, the PG Dean of BJMC, Dr. Shekhar Pradhan informed Hindustan Times that the committee has been constituted to investigate the complaint. He added, “The complaint was received last week and such issues are handled seriously. The complainant said she was harassed and ragged while working in the department. The entire investigation will be headed by the PG redressal committee.”
The PG Dean further informed that the panel in charge of investigating the matter has started to record the statements of junior and senior students. Apart from the students, the committee will also record the statements of the students accused of ragging. Action against the accused doctors will be taken only after considering the report submitted by the committee.
“We are also recording the statements and responses of the faculty members and senior faculties to verify the facts of the complaint. The action will be taken after the report is submitted by the committee,” Dr. Pradhan said.
An incident of harassment of female resident doctors was reported last year on December 31, 2023. Back then, some of the PG students at the male residents’ hostel consumed alcohol, went to the resident hostel for the females and created chaos. After the drunk doctors smashed a window of the female hostel resulting in panic, two female residents lodged a complaint to the college administration.
The Deputy Chief Minister Ajit Pawar also took cognizance of the matter and slammed the college and hospital administration for the liquor party and the chaos that took place on the premises on the occasion of New Year’s Eve. However, HT adds that no action was taken by the college authorities in this regard.
Aiming to prevent ragging in medical colleges across India, the National Medical Commission (NMC) had earlier spelt out the regulations titled “Prevention and Prohibition of Ragging in Medical Colleges and Institutions Regulations, 2021”. It also specified the disciplinary actions to be taken while dealing with incidents of ragging.
NMC, the apex medical education regulatory body mentioned the measures to prohibit and prevent ragging by institutions including the duties and responsibilities of the institutes, measures required to be taken by the medical colleges, issue of migration, transfer or conduct certificates, measures to encourage healthy interaction between freshers and seniors, Sensitisation of institutional employees and staff towards ragging, Institutional committees and related measures, Anti-ragging squad, Student Affairs or Hostel Committee, duties of the universities, etc.
Also Read: NMC Regulations spell out Disciplinary Action for Ragging in Medical Colleges
Powered by WPeMatico
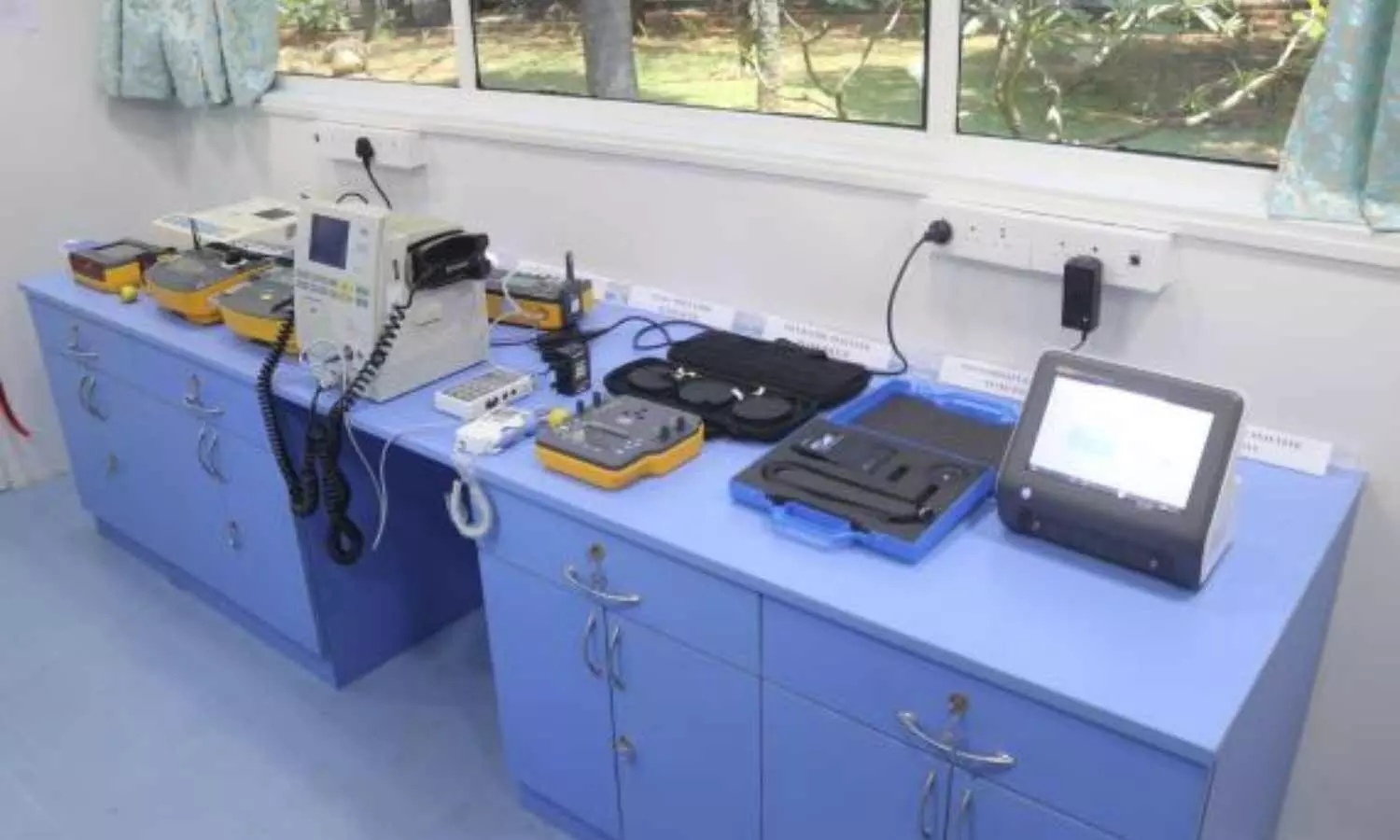
Chennai: Indian Institute of Technology Madras (IIT Madras) has launched India’s First ‘medical devices calibration facility on wheels’. This has been developed by IIT Madras under its ‘Anaivarukkum IITM’ (IITM for all) Initiatives.
Prof. V. Kamakoti, Director, IIT Madras, launched this facility at the campus on 15th April 2024 in the presence of Prof. R. Sarathi, Dean (Planning), Prof. M. Anbarasu (Head, CEC), Prof. S. Ramakrishnan, faculty and students.
Highlighting the importance of this initiative, Prof. V. Kamakoti, Director, IIT Madras, “Proper Diagnosis and treatment are extremely important and for that the medical devices need to be calibrated accurately and frequently.
Also Read: IIT Madras, THSTI Faridabad develop AI model to determine foetus age
With escalating cost for calibration this effort not only reduces the cost of calibration but also the transportation cost and time required. This is a progressive step towards affordable, scalable, quality health care for all.”
Maintenance and quality assurance of life-saving medical devices are of paramount importance for healthcare delivery. Calibration is crucial as it ensures the accuracy of medical instruments for precise disease diagnosis and effectiveness. This facility is first-of-its-kind in India and is geared towards providing an affordable quality calibration facility and enabling accurate disease diagnosis and treatment.
This mobile facility will ensure pervasive quality healthcare irrespective of geographical locations across the country. This will help to test and maintain medical devices that are used in wide range of hospitals including those in villages at their doorsteps.
This initiative boosts the United National Sustainable Development Goal 3, which calls for Health and well-being for all.
The infrastructure available in this mobile unit include state-of-the-art equipment to test the safety of medical devices and their functionalities as per international standards.
Powered by WPeMatico

A recent study published in the Journal of American Medical Association discovered that managing cholesterol levels from childhood could significantly reduce the risk of cardiovascular disease (CVD) in adulthood. The study spanned through several decades and followed participants from childhood through to their 40s to assess how variations in non-high-density lipoprotein cholesterol (non–HDL-C) levels affect the incidence of heart disease later in life.
Non-HDL-C is a critical measure of cholesterol that encompasses all harmful types of blood lipids and it has been identified as a reliable marker for predicting cardiovascular risks in adults. This extensive research was conducted across six prospective cohorts in the US and Finland to analyze data from individuals who were initially examined as children, starting from 1970 to 1996 with the follow-ups that continued until 2019.
The cohort of this study consisted of 5,121 participants with a balanced demographic representation including 60% women and 15% Black participants. This research tracked the non-HDL-C levels of participants from an average starting age of 10.7 years into their mid-adulthood by classifying the levels according to age- and sex-specific z-scores and existing clinical guidelines for dyslipidemia.
Over an average follow-up period of 8.9 years when the participants reached 40 years of age, 147 CVD events were observed. The analysis showed a strong association between both childhood and adult non-HDL-C levels and the elevated risk of CVD, with a more pronounced risk noted in the individuals with high non-HDL-C levels that persisted into adulthood. The hazard ratios (HR) were significantly high for individuals with sustained high non-HDL-C levels from childhood through to adulthood by indicating a fivefold increase in the risk of CVD events when compared to the individuals whose levels remained within the recommended range.
This study also found that individuals who managed to bring their non-HDL-C levels back to within the recommended range by adulthood did not face a significantly increased risk of heart disease which demonstrated similar risk levels to the individuals who never had dyslipidemia.
They suggest that interventions reduce elevated non-HDL-C levels in children could play a critical role to prevent the development of cardiovascular diseases later in life. Overall, the findings emphasize the importance of regular cholesterol monitoring from early childhood and continuing through adulthood along with lifestyle adjustments and medical interventions as required.
Source:
Wu, F., Jacobs, D. R., Jr, Daniels, S. R., Kähönen, M., Woo, J. G., Sinaiko, A. R., Viikari, J. S. A., Bazzano, L. A., Steinberger, J., Urbina, E. M., Venn, A. J., Raitakari, O. T., Dwyer, T., Juonala, M., & Magnussen, C. G. (2024). Non–High-Density Lipoprotein Cholesterol Levels From Childhood to Adulthood and Cardiovascular Disease Events. In JAMA. American Medical Association (AMA). https://doi.org/10.1001/jama.2024.4819
Powered by WPeMatico

Mexico: SITA-PLUS hospital trial published in the Journal of Diabetes and its Complications has shed light on the safety and efficacy of sitagliptin with basal-plus (BP) insulin regimen versus insulin alone in non-critically hospitalized patients with type 2 diabetes (T2D).
The study revealed that the sitagliptin and BP regimen combination is safe and more effective than insulin therapy alone for inpatients with type 2 diabetes and hyperglycemia.
“Combining sitagliptin with a basal-plus insulin regimen leads to a comparable risk of hypoglycemia, lower daily blood glucose levels, and lower insulin doses than the basal-plus regimen alone,” the researchers reported.
The recommended method for insulin administration is a basal-bolus regimen, which involves the daily subcutaneous injection of basal insulin, along with rapid-acting insulin before meals for prandial and correctional doses. However, its application is limited by the complexity of this approach and the risk of hypoglycemia.
Previous studies have revealed that basal and correctional insulin doses (basal-plus regimen) with sitagliptin are similar to the basal-bolus insulin regimen in hyperglycemia management in a hospital setting. However, no clarity exists on whether this combination is better than a basal-plus regimen alone. Therefore, Abraham Edgar Gracia-Ramos, Instituto Mexicano del Seguro Social, Mexico City, Mexico, and colleagues aimed to compare the safety and efficacy of basal-plus insulin regimen with or without sitagliptin in non-critically ill patients with type 2 diabetes.
For this purpose, the researchers conducted an open-label, randomized clinical trial comprising patients with a previous diagnosis of T2D and blood glucose (BG) between 180 and 400 mg/dL. Participants received basal and correctional insulin doses (BP regimen) either with or without sitagliptin. The study’s primary outcome was the difference in the mean daily blood glucose among the groups. Seventy-six patients (mean age 60 years, 64 % men) were randomized.
Based on the study, the researchers reported the following findings:
“These results are significant because using DPP-4 inhibitors with basal-plus insulin therapy simplifies hospital diabetes management for healthcare professionals, improves treatment adherence, and leads to better patient outcomes,” the researchers wrote.
Reference:
Gracia-Ramos, A. E., Cruz-Dominguez, M. D. P., Madrigal-Santillán, E. O., Rojas-Martínez, R., Morales-González, J. A., Morales-González, Á., Hernández-Espinoza, M., Vargas-Peñafiel, J., & Tapia-González, M. D. L. Á. (2024). Efficacy and safety of sitagliptin with basal-plus insulin regimen versus insulin alone in non-critically ill hospitalized patients with type 2 diabetes: SITA-PLUS hospital trial. Journal of Diabetes and its Complications, 38(5), 108742. https://doi.org/10.1016/j.jdiacomp.2024.108742
Powered by WPeMatico

India: A recent in vivo study published in Frontiers in Nutrition has shed light on the effect of quinoa (Chenopodium quinoa W.) flour supplementation in breads on the lipid profile and glycemic index (GI).
The study showed that quinoa-incorporated bread possessed a low glycemic index (42.00 ± 0.83) compared to the control (69.20 ± 1.84) and long-term consumption proved to contain functional efficacies, in terms of hypolipidemic effect.
“Incorporating quinoa into bread formulations not only enhances their nutritional content but also offers potential health benefits, particularly in managing cardiovascular health and blood sugar levels,” the researchers wrote. The findings highlight the positive effects of quinoa flour supplementation in bread on lipid profile and glycemic index.
Quinoa has recently gained significant popularity as a nutritious and versatile grain alternative. Beyond its use as a standalone dish, researchers have been exploring its potential as a functional ingredient in various food products. One such avenue of investigation is its incorporation into bread, a staple food consumed worldwide.
Quinoa (Chenopodium quinoa W.) is a pseudo-cereal rich in protein, vitamins, dietary fiber, and minerals. Its nutritional profile makes it an attractive candidate for improving the health properties of baked goods like bread.
Against the above background, Natasha R. Marak, Central Agricultural University, Tura, Meghalaya, India, and colleagues aimed to investigate the effects of quinoa bread on physical, chemical, and bioactive components, glycaemic index, and biochemical parameters.
For this purpose, the researchers fed human subjects aged between 20 and 50 years with the absence of morbid factors daily with quinoa bread for 3 months to study its pre-and post-treatment effects on lipid profile, glycosylated hemoglobin, and blood glucose.
The effort was made to incorporate the maximum amount of quinoa into the bread without compromising the bread’s acceptability. Of the 14 formulations, TQ13, containing 20% quinoa flour with 3% wheat bran, was selected for further analysis.
Based on the study, the researchers reported the following findings:
According to the study, these benefits have proved crucial in the dietary treatment of diabetes mellitus by resulting in improved glycaemic control and several metabolic parameters, such as improved blood lipid levels.
Based on the data obtained in the study, the researchers concluded that quinoa incorporation into wheat bread results in essential health benefits.
High consumption of phenolic compounds has long been associated with reduced risk of cardiovascular diseases and certain cancers. “Current trends in the enhancement of the antioxidant capacity of wheat bread by quinoa flour addition rich in phenolic compounds might be beneficial in the health status of a population,” the researchers concluded. “The results obtained in the present study corroborate the data reported in the literature, indicating that quinoa bread can be used in glycemic control and plasma lipids.”
Reference:
Marak, N. R., Das, P., Das Purkayastha, M., & Baruah, L. D. (2024). Effect of quinoa (Chenopodium quinoa W.) flour supplementation in breads on the lipid profile and glycemic index: An in vivo study. Frontiers in Nutrition, 11, 1341539. https://doi.org/10.3389/fnut.2024.1341539
Powered by WPeMatico
A recent research identified a potential breakthrough in diagnosing a novel form of asthma in children known as Chest Tightness-Variant Asthma (CTVA). CTVA is characterized by chest tightness as the primary symptom and presents a diagnostic challenge due to its atypical nature. However, a recent study published in the recent edition of Respiratory Medicine journal illuminates the promise of this diagnostic approach.
The study was conducted on a total of 95 children aged 6 to 14 years with chest tightness as their only symptom for more than four weeks. Tengteng Zhang and team evaluated the efficacy of combining bronchial provocation testing with fractional exhaled nitric oxide (FeNO) measurement for the diagnosis of CTVA.
The results revealed that while lung function remained normal in both CTVA and non-CTVA groups, the FeNO levels significantly differed. The children in the CTVA group expressed FeNO levels averaging 22.35 parts per billion (ppb) that was markedly higher than the average of 14.85 ppb in the control group. This discrepancy in FeNO levels proved statistically significant (P < 0.05).
Utilizing the receiver operating characteristic (ROC) curves, further analysis demonstrated that FeNO could help in diagnosing CTVA, with an optimal cutoff point of 18.5 ppb. At this threshold, FeNO expressed a sensitivity of 60.3% and specificity of 77.8%. Additionally, a negative correlation was observed between FeNO levels and bronchial hyperresponsiveness parameters such as Dmin and PD15 (P = 0.006).
Despite these promising findings, it is essential to note that FeNO alone does not serve as a definitive diagnostic marker for CTVA. Instead, it should be utilized alongside bronchial provocation testing to enhance the diagnostic accuracy. The integration of FeNO measurement into the diagnostic process provides the clinicians with a supplementary tool to help in the identification of CTVA that offers a non-invasive and relatively simple approach for pediatric patients.
This development in CTVA care holds significance for the clinicians with the challenges of diagnosing atypical asthma presentations in children who present solely with the chest tightness symptoms. Overall, the healthcare professionals can expedite appropriate treatment strategies by refining diagnostic methods which in turn improves the outcomes and quality of life of patient. Further research and clinical validation is mandated for this innovative approach that could potentially transform the management of CTVA by benefiting children globally.
Reference:
Zhang, T., Xu, L., Zhang, Y., & Zhen, L. (2024). The diagnostic value of bronchial provocation testing combined with fractional exhaled nitric oxide (FeNO) in children with chest tightness-variant asthma (CTVA). In Respiratory Medicine (Vol. 223, p. 107543). Elsevier BV. https://doi.org/10.1016/j.rmed.2024.107543
Powered by WPeMatico

WASHINGTON: A third of the nearly 20 million women who participated in a national health survey report migraines during menstruation, and of them, 11.8 million, or 52.5%, were premenopausal.
The analysis was conducted by researchers at Georgetown University Medical Center and Pfizer, Inc., which makes a migraine medication.
Because of the underuse of medications to help treat or prevent menstrual migraines, investigators wanted to understand how common menstrual migraines were and which groups of women could most benefit from potential therapies. The study will be presented April 16, at the American Academy of Neurology 2024 Annual Meeting in Denver.
“The first step in helping a woman with menstrual migraine is making a diagnosis; the second part is prescribing a treatment; and the third part is finding treatments patients are satisfied with and remain on to reduce disability and improve quality of life,” says the study author, Jessica Ailani, MD, professor of clinical neurology at Georgetown University School of Medicine and director of the MedStar Georgetown Headache Center at Medstar Georgetown University Hospital.
The researchers used the 2021 U.S. National Health and Wellness Survey, conducted by the National Center for Health Statistics, to analyze responses from women who reported their current migraine treatments, frequency and disabilities via the Migraine Disability Assessment Test (MIDAS), a five-question survey. A migraine headache can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound.
“Discrepancies in the incidence of who gets migraine attacks associated with menses is likely due to premenopausal women having more regular menstrual cycles and thus more menstrual-related migraines,” says Ailani. “Additionally, as women move into their 40’s and become peri-menopausal, there tends to be a greater shift through the month in hormone levels also leading to frequent migraine attacks.”
The survey found that for all women during their menstrual periods, migraine attacks occurred as frequently as 4.5 times and that monthly only migraine headaches lasted 8.4 days, on average; 56.2 % of women had moderate-to-severe migraine-specific disabilities that ranked highest on the MIDAS scale.
When looking at treatments women in the survey used to help control their migraine symptoms, 42.4% used over-the-counter medications while 48.6% used prescription medications. Of the 63.9 % of women who used migraine treatments for acute symptoms, the most commonly used were triptans, a class of drugs developed in the 1990s to quiet overactive nerves associated with migraines and cluster headaches.
Sara’s story
Sara, a 38 year old mother of two, says her migraines are predictably and consistently worse during her period.
“It definitely disrupts my ability to go about my normal activities including at work,” Sara says. “I’m pretty lucky that I’m generally responsive to prescription medication, but I often still have to lie down for an hour or so while the medicine kicks in.”
Sara is being treated preventatively for migraines with Botox. She says over the past couple of months, she’s had a couple of migraines outside of when she gets her period, but that the headaches are definitely worse during menstruation.
“While I had my last period, I had a migraine every day for a week,” Sara says. “It’s starkly different [during menstruation].”
Prevention Possibilities
Non-steroidal anti-inflammatory drugs (NSAIDs), such as naproxen or ibuprofen, are sometimes used as preventive medications for women with regular menstrual periods. In this study, 21.1% of women reported use of any migraine prevention medications or therapies.
“Preventive treatments are used less frequently than acute treatment for migraine,” Alaini said.
“In my opinion, this is because preventive therapy is a long-term commitment by both a woman and her clinician to improving the disease process. Migraine is a life-long brain disease without a cure, and the goal of preventive therapy is to reduce disease burden and improve quality of life. Unfortunately, newer disease-specific treatments are costly, so generic older treatments are often used and come with greater side effects.”
Next Steps
The researcher’s next steps involve looking at larger databases to see if they can mimic findings on a global scale. They want to determine if women with menstrual-related migraine are frequently turning to non-migraine treatments as was seen in around 53% of their current study group.
“As a headache specialist in the U.S., I know I can do better for women in my clinic, but what can be done for the millions of women who don’t get into a headache clinic? That is our true next step,” says Ailani. “If you have migraines related to your menstrual cycle, discuss this with your gynecologist or neurologist. There are treatments that can help and if the first treatment tried does not work, do not give up.”
Powered by WPeMatico

Premature menopause linked to negative work ability and higher disability retirement suggests a new study published in the Menopause.
A study was done to study the association between an advanced climacteric status at 46 years of age and current perceived work ability, the consequent 2-year accumulation of disability and unemployment days, and the 7-year incidence of disability pensions. Study participants (n = 2,661) were recruited from the Northern Finland Birth Cohort 1966 study’s 46-year follow-up in 2012. The participants’ perceived work ability was investigated using the Work Ability Score (0-7 = poor vs 8-10 = good), along with potential covariates. Data concerning their consequent disability days, unemployment days, and disability pensions were collected from national registers. The association between their climacteric status at age 46 years, work ability, and working life participation was assessed using regression models. Results: The climacteric women were more often smokers and more often had a lower level of education. The odds ratio for poor perceived work ability was 1.41 (95% CI, 1.06-1.87), and the incidence rate ratios for disability and unemployment days during the 2-year follow-up were 1.09 (95% CI, 1.07-1.11) and 1.16 (95% CI, 1.14-1.18), respectively, for the climacteric women compared with the preclimacteric women in models adjusted for smoking and education. The 7-year hazard ratio for disability pensions was 1.72 (95% CI, 1.02-2.91) for the climacteric women. An earlier menopausal transition is associated with poorer perceived work ability, and it predicts lower recorded work participation and a higher disability pension rate in subsequent years.
Reference:
Saarinen, Tiia BM1,2,3; Savukoski, Susanna M. MD, PhD1,2,3; Pesonen, Paula MSc4; Vaaramo, Eeva MSc4; Laitinen, Jaana MSc, PhD5; Varanka-Ruuska, Tuulia MD5,6; Ala-Mursula, Leena MD, PhD6; Niinimäki, Maarit MD, PhD1,2,3. Climacteric status at age 46 is associated with poorer work ability, lower 2-year participation in working life, and a higher 7-year disability retirement rate: a Northern Finland Birth Cohort 1966 study. Menopause 31(4):p 275-281, April 2024. | DOI: 10.1097/GME.0000000000002327
Keywords:
Premature menopause, negative work ability, higher disability, retirement, Saarinen, Tiia BM1,2,3; Savukoski, Susanna M. MD, PhD1,2,3; Pesonen, Paula MSc4; Vaaramo, Eeva MSc4; Laitinen, Jaana MSc, PhD5; Varanka-Ruuska, Tuulia MD5,6; Ala-Mursula, Leena MD, PhD6; Niinimäki, Maarit MD
Powered by WPeMatico
