Doctors cite unmedicated mental illness in Sydney mall attack
Powered by WPeMatico
Powered by WPeMatico
Breast cancer is a type of cancer that forms in the cells of the breast tissue. It occurs when abnormal cells in the breast begin to grow uncontrollably, forming a tumour that can invade nearby tissues and potentially spread to other parts of the body.
Breast cancer can affect both men and women, although it is much more common in women. It is the most prevalent cancer among women worldwide, with millions of new cases diagnosed each year.
Early detection through regular screenings and awareness of risk factors is crucial in improving outcomes and reducing mortality rates associated with breast cancer. Breast cancer can arise from a combination of genetic, environmental, and lifestyle factors.
Risk Factors
1. Genetic Mutations: Inherited mutations in genes such as BRCA1 and BRCA2 can significantly increase the risk of developing breast cancer.
2. Age: The risk of breast cancer increases with age, with the majority of cases occurring in women over 50.
3. Family History: Having a first-degree relative (mother, sister, or daughter) with breast cancer can elevate the risk.
4. Hormonal Factors: Prolonged exposure to estrogen, whether through early menstruation, late menopause, or hormone replacement therapy, can increase the risk.
5. Personal History: Women who have previously had breast cancer or certain non-cancerous breast conditions may have a higher risk of developing it again.
6. Dense Breast Tissue: Women with dense breast tissue may have a higher risk of breast cancer.
7. Excessive Alcohol Consumption: Consuming more than one alcoholic drink per day can slightly increase the risk.
8. Obesity: Being overweight or obese, especially after menopause, is linked to an increased risk of breast cancer.
9. Radiation Exposure: Previous radiation therapy to the chest, especially during childhood or adolescence, can raise the risk.
10. Lack of Physical Activity: Leading a sedentary lifestyle with little to no physical activity may contribute to a higher risk of breast cancer.
While these factors may increase the likelihood of developing breast cancer, it’s essential to note that many women diagnosed with breast cancer have no identifiable risk factors. Regular screenings and early detection remain crucial for managing the disease effectively.
Symptoms
Symptoms of breast cancer can vary among individuals, but common signs to watch for include:
A hard lump or mass in the breast or underarm area is often the first noticeable symptom.
The changes in Breast Size or Shape, like Swelling, shrinkage, or changes in contour, especially on one side, may indicate breast cancer.
Redness, dimpling, puckering, or thickening of the breast skin, resembling an orange peel, can be signs of breast cancer.
Changes in the nipple, such as inversion, retraction, or discharge (other than breast milk), should be evaluated by a healthcare professional.
While breast pain is more commonly associated with benign conditions, persistent, unexplained pain should be assessed.
Preventive measures for Breast Cancer
1. Regular Screening: Mammograms and clinical breast exams can help detect breast cancer at early stages when treatment is most effective.
2. Healthy Lifestyle: Maintaining a healthy weight, exercising regularly, limiting alcohol consumption, and avoiding smoking can reduce the risk of breast cancer.
3. Breastfeeding: Women who breastfeed may have a lower risk of developing breast cancer.
4. Know Your Risk: Understanding your personal risk factors, such as family history and genetic mutations, can help guide preventive strategies and screening recommendations.
5. Breast Self-Exams: While not a substitute for regular screening, becoming familiar with the normal look and feel of your breasts can help detect changes early.
6. Genetic Counselling and Testing: For individuals with a strong family history of breast cancer or known genetic mutations, genetic counselling and testing may provide valuable information for preventive measures and screening recommendations.
7. Hormone Therapy: Some women may reduce their risk of breast cancer by avoiding long-term use of hormone replacement therapy.
By being aware of the symptoms and taking proactive steps to reduce risk, individuals can empower themselves in the fight against breast cancer. Early detection and preventive measures are key in improving outcomes and reducing mortality rates associated with the disease.
Disclaimer: The views expressed in this article are of the author and not of Medical Dialogues. The Editorial/Content team of Medical Dialogues has not contributed to the writing/editing/packaging of this article.
Powered by WPeMatico

Jaipur: The incident of a pregnant woman delivering her baby outside the Kanwatia Government Hospital in the city on April 3 after she was allegedly denied admission has brought attention to the lack of a permanent obstetrics and gynaecology unit at the hospital.
The incident highlights significant gaps in care at the facility, which currently relies on a rotating unit provided monthly by the Sawai Man Singh Medical College.
Four years ago, Kanwatia Government Hospital had a dedicated obstetrics and gynaecology unit, but the current situation has reduced the quality of care for patients. The hospital typically handles around 140 to 150 births monthly, underscoring the need for consistent and reliable maternity services. However, for now, the Sawai Man Singh Medical College provides a rotating unit every month.
In contrast, nearby hospitals such as Gangori Hospital, affiliated with SMS Medical College, maintain dedicated obstetrics and gynaecology units. As per a recent media report by Times of India, recently a meeting was held to talk about improving facilities at Kanwatia Government Hospital. The administration has requested a permanent gynaecology unit that would include a professor, associate, and assistant professors, and senior resident doctors. The hospital argued that such a unit is crucial to adequately care for the 140 to 150 pregnant women it admits each month, helping to prevent further incidents.
In response to the incident on April 3, the medical education department formed a five-member committee to reinvestigate the case. As a result of the inquiry, senior resident Dr Sushma and three other resident doctors were initially suspended. However, Dr Sushma’s suspension was later rescinded following her appeal.
Medical Dialogues team had earlier reported that this move was taken after a preliminary investigation found their action as “serious negligence and insensitivity” and consequently suspended them. In addition to suspending them, the department also served a show cause notice to the medical superintendent Dr Rajendra Singh Tanwar for supervisory negligence in the case.
Powered by WPeMatico

USA: Taichi training or Taichi plus resistance band training effectively improves blood glycemic control and pulmonary diffusion capacity in patients with type 2 diabetes mellitus (T2DM), a recent study published in PLOS One has shown.
Variation of diffusion capacity of the lungs for carbon monoxide (DLCO) is predicted by IL-6, eNOS, vWF, TNF-α, and insulin sensitivity. Insulin sensitivity was shown to be far more important than other factors, which is likely a driving force to benefit anti-inflammation, blood glycemic control, and endothelial function.
“Reciprocally, Taichi training reduced inflammatory markers and enhanced endothelial nitric oxide synthase (eNOS), which reinforces with improved glycemic control, contribute to improved pulmonary diffusion capacity in patients with T2DM,” the researchers wrote.
In the realm of holistic wellness, the ancient practice of Taichi has emerged as a beacon of hope, especially for individuals grappling with Type 2 diabetes mellitus. Recent research has unveiled a promising avenue for managing this metabolic condition: twenty-four weeks of Taichi training. Beyond its renowned benefits for physical and mental well-being, Taichi appears to wield a transformative power over pulmonary diffusion capacity and glycemic control in diabetes patients.
Pulmonary diffusion capacity, a measure of the lung’s ability to exchange gases, is a pivotal aspect of respiratory health often compromised in diabetes patients. Remarkably, Taichi training demonstrated a remarkable enhancement in pulmonary diffusion capacity among participants. The rhythmic movements and controlled breathing inherent in Taichi’s practice fostered lung efficiency, facilitating better oxygenation and carbon dioxide elimination. Such pulmonary function improvements alleviate respiratory distress and bolster overall vitality and resilience.
Against the above background, Xiaoli Liu, University of North Texas Health Science Center, Fort Worth, Texas, United States of America, and colleagues investigated the effect of 24-week Taichi training and Taichi plus resistance band training on pulmonary diffusion capacity and glycemic control in patients with T2DM.
For this purpose, forty-eight patients with T2DM were included. They were randomly divided into three groups: Group A—Taichi training: practiced Taichi 60 min/day, six days/week for 24 weeks; Group B—Taichi plus resistance band training: practiced 60-min Taichi 4 days/week plus 60-min resistance band training two days/week for 24 weeks; and Group C–controls: maintaining their daily lifestyles.
Stepwise multiple regression analysis was applied to predict DLCO by insulin, fasting blood glucose, tumor necrosis factor-alpha (TNF-α), glycosylated hemoglobin (HbA1c), interleukin-6 (IL-6), von Willebrand Factor (vWF), endothelial nitric oxide synthase (eNOS), intercellular adhesion molecule 1 (ICAM-1), endothelin-1 (ET-1), nitric oxide (NO), prostaglandin I-2, and vascular endothelial growth factor.
The study led to the following findings:
In conclusion, the study demonstrates that 24-week Taichi training and Taichi plus resistance band training effectively improve blood glycemic control and pulmonary diffusion capacity in patients with T2DM.
DLCO variation is explained by improved endothelial function and insulin sensitivity, and reduced inflammatory markers, including TNF-α, vWF, and IL-6.
Reference:
Liu, X., Zhu, H., Peng, Y., Liu, Y., & Shi, X. (2024). Twenty-Four week Taichi training improves pulmonary diffusion capacity and glycemic control in patients with Type 2 diabetes mellitus. PLOS ONE, 19(4), e0299495. https://doi.org/10.1371/journal.pone.0299495
Powered by WPeMatico
USA: Higher lipoprotein (a) levels are associated with an increased atherosclerotic cardiovascular disease (ASCVD) risk, including in patients with diabetes in a large US pooled cohort, a recent study published in the Journal of the American College of Cardiology has shown.
“The heightened risk with Lp(a) was observed in women and men, in non-Black and Black participants, and in those at low-intermediate and high risk for cardiovascular disease (CVD) over more than 20 years of follow-up,” the researchers reported. Among patients with diabetes mellitus, increases in Lp(a) were linked to an even greater risk of CV events.
ASCVD, characterized by the buildup of plaque in arterial walls, stands as a leading cause of mortality and morbidity worldwide. Individuals with diabetes face a disproportionately higher risk of ASCVD, compounding the already formidable challenges posed by their underlying condition. Against this backdrop, understanding the role of Lp(a) assumes paramount importance.
Lp(a), a unique lipoprotein subclass, has garnered attention for its potential role in atherogenesis. Its structure, consisting of an LDL-like particle linked to apolipoprotein(a), sets it apart from traditional lipid markers.
As noted above, Lp[a] is a causal genetic risk factor for atherosclerotic cardiovascular disease. However, long-term follow-up data from large U.S. population cohorts are limited. Considering this, Nathan D. Wong, Division of Cardiology, University of California—Irvine, Irvine, California, USA, and colleagues aimed to examine the relationship of Lp(a) with ASCVD outcomes in a large, pooled, multi-ethnic U.S. cohort.
The study included data on Lp(a) and ASCVD outcomes from 5 U.S. prospective studies: ARIC (Atherosclerosis Risk In Communities), FHS-OS (Framingham Heart Study-Offspring), JHS (Jackson Heart Study), CARDIA (Coronary Artery Risk Development in Young Adults), and MESA (Multi-Ethnic Study of Atherosclerosis).
Lp(a) levels were classified based on cohort-specific percentiles. Multivariable Cox regression related lipoprotein (a) with composite incident ASCVD events by risk group and diabetes status.
27,756 persons without previous ASCVD who were aged 20 to 79 years were included in the study, including 55.0% women, 35.6% Black participants, and 7.6% patients with diabetes, with a mean follow-up of 21.1 years.
The study led to the following findings:
These new data indicate that Lp(a) is an “equal opportunity risk factor across several demographic and clinical categories,” Gregory G. Schwartz, University of Colorado School of Medicine, Aurora, wrote an accompanying editorial.
Regarding the guidelines, Schwartz also believes the US approach of Lp(a) measurement only in select patients might be too restrictive, including the recommendation only to screen in women with hypercholesterolemia. “Current Canadian and European guidelines that recommend testing in most adults would appear to be supported by the current findings,” he states.
Reference:
Wong ND, Fan W, Hu X, et al. Lipoprotein(a) and long-term cardiovascular risk in a multiethnic pooled prospective cohort. J Am Coll Cardiol. 2024;83:1511-1525.
Powered by WPeMatico

Italy: A recent study published in the European Journal of Pediatrics has shown continuous glucose monitoring (CGM) to be a promising tool for individualizing nutritional strategies in preterm infants during the first weeks of birth.
The study found that macronutrient intakes influence neonatal glucose profile as described by CGM and might contribute to adjusting nutritional intakes in preterm infants.
“Continuous glucose monitoring describes the relationship between the intake of daily parenteral nutrients and time spent in hypo and hyperglycemic ranges,” the researchers reported.
Preterm infants, born before 37 weeks of gestation, often face numerous challenges in adapting to extrauterine life, including the regulation of blood sugar levels or glycemic homeostasis. Adequate nutrition has a pivotal role in supporting their growth and development, with macronutrients such as carbohydrates, proteins, and fats being key components of their diet. Recent advancements in medical technology, particularly CGM, have provided unprecedented insights into the intricate interplay between macronutrient intake and glycemic control in these vulnerable neonates.
As described above, nutritional intake could influence the blood glucose profile during the early life of preterm infants. Alfonso Galderisi from the Institute for Pediatric Research (IRP) in Padua, Veneto, Italy, and colleagues aimed to investigate the impact of macronutrient intake on glycemic homeostasis using continuous glucose monitoring.
For this purpose, the researchers analyzed macronutrient intake in infants born ≤ 32 weeks gestational age (GA) and/or with birth weight ≤ 1500 g. CGM was initiated within 48 hours of birth and maintained for five days.
Mild and severe hypoglycemia were defined as sensor glucose (SG) < 72 mg/dL and <47 mg/dL, respectively, while mild and severe hyperglycemia were SG > 144 mg/dL and >180 mg/dL. Data from 30 participants were included (age 29.9 weeks, birthweight 1230.5 g).
The study led to the following findings:
In conclusion, the study demonstrates the relationship between macronutrient intake and glucose homeostasis during the first days of life of very low birth weight infants wearing a CGM. Higher amino acid intake is associated with reduced time spent in the hypoglycemic range, while greater lipids intake increases exposure to hyperglycemia.
Amino acid and lipid intakes largely impact insulin sensitivity, which in turn, is a major determinant of hyper and hypoglycemia in the first days of birth of preterm infants, explaining this apparent contradiction. Transient glucose fluctuations are mainly due to procedures and the multiple stressors occurring during the first days of life and directly impact insulin sensitivity.
“We hypothesize that amino acid and lipid intakes, in turn, impact glucose fluctuations by directly acting on insulin sensitivity,” the researchers wrote.
Reference:
Guiducci, S., Res, G., Bonadies, L. et al. Impact of macronutrients intake on glycemic homeostasis of preterm infants: evidence from continuous glucose monitoring. Eur J Pediatr (2024). https://doi.org/10.1007/s00431-024-05532-4
Powered by WPeMatico

Lower urinary tract symptoms are significantly associated with anxiety suggests a study published in the Prostate International.
Patients with lower urinary tract symptoms (LUTS) often experience comorbid depression and anxiety, yet the mechanisms underlying this association remain incompletely understood. This prospective study aimed to investigate the relationship between depression, anxiety, and LUTS in men. A prospective study was conducted with 350 male patients who underwent urologic examinations at our institution from January 2021 to December 2021. Of these, 131 patients meeting the inclusion criteria were included. Various questionnaires, including the International Prostate Symptom Score (IPSS) and the Hospital Anxiety and Depression Scale (HADS), as well as LUTS examinations (prostate-specific antigen test, transrectal ultrasonography, and urine flowmetry), were administered.
Results: Among the 350 patients, 131 were included in the analysis, with an average age of 58.0 ± 13.69 years. The total IPSS was 18.0 ± 8.69, with the average voiding symptom score at 8.7 ± 5.19 and the average storage symptom score at 6.0 ± 3.27. Both anxiety and depression were found to be correlated with LUTS (P < 0.05). After adjusting for age, hypertension, and diabetes, anxiety (but not depression) was significantly associated with LUTS based on regression analysis. Men with LUTS are more likely to experience anxiety. Therefore, it is essential to assess and address anxiety when managing men with LUTS.
Reference:
Yu Seob Shin, Kiran Kumar Soni, Dong Yun Lee, Sung Chul Kam. The relationship between depression, anxiety and lower urinary tract symptoms in men, Prostate International, 2024, ISSN 2287-8882, https://doi.org/10.1016/j.prnil.2024.02.002. (https://www.sciencedirect.com/science/article/pii/S2287888224000047)
Powered by WPeMatico

A new study sheds light on the impact of delayed appendicitis diagnosis on hospital care costs, revealing implications for healthcare reimbursement policies and disparities in patient care. Delayed diagnosis of appendicitis is associated with adverse outcomes, prolonged hospital stays, and increased likelihood of readmissions.
Despite evidence of disparities in diagnosis rates, hospitals serving minority populations often receive lower reimbursement, raising concerns about equitable healthcare quality metrics. This study was published in the journal JAMA Network Open. The study was conducted by Kulaskera and colleagues.
Researchers conducted a retrospective cohort study of 76,173 patients aged 18-64 who underwent appendectomy across multiple states in the US. The study analyzed data from 2016 to 2017, focusing on the association between delayed appendicitis diagnosis and hospital care costs. Patients with delayed diagnosis were identified based on prior abdominal diagnoses without appendicitis and no intervention seven days before appendectomy admission.
The key findings of the study were as follows:
Patients with delayed diagnosis had 1.23 times increased hospital care costs compared to those without delayed diagnosis.
Median unadjusted costs for delayed diagnosis were $11,099, significantly higher than $9177 for non-delayed diagnosis.
Adjusted analysis revealed a 1.23 times higher likelihood of increased hospital costs for delayed diagnosis patients.
Non-Hispanic Black individuals experienced 1.22 times higher appendicitis hospital care costs compared to non-Hispanic White patients.
Older age groups and patients on Medicare disability or Medicaid had significantly greater costs.
The study underscores the importance of timely diagnosis in appendicitis management and its impact on healthcare costs. It highlights disparities in care quality and reimbursement policies, particularly affecting minority populations. Understanding the mechanisms behind delayed diagnosis among minority patients is crucial for addressing healthcare disparities effectively.
Delayed appendicitis diagnosis significantly increases hospital care costs, with implications for healthcare reimbursement policies and disparities in patient care. Addressing disparities in diagnosis rates and implementing equitable quality metrics are essential steps toward improving healthcare outcomes for all populations.
Reference:
Kulasekere, D, Royan, R, Shan Y. Appendicitis Hospitalization Care Costs Among Patients With Delayed Diagnosis of Appendicitis. JAMA Network Open. 2024;7(4):e246721. doi:10.1001/jamanetworkopen.2024.6721.
Powered by WPeMatico
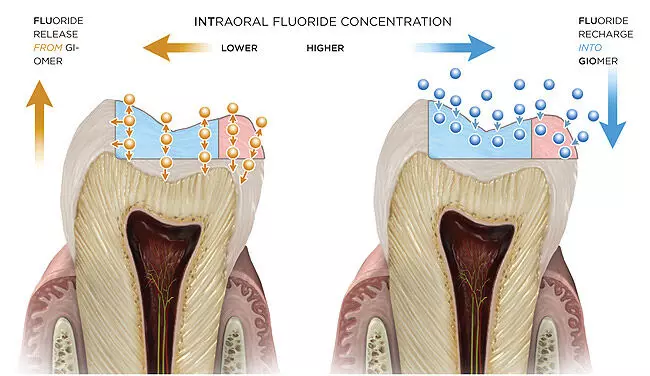
Surface pre-reacted glass-ionomer filler containing topical applications may prevent caries suggests a study published in the Journal of Dentistry.
The objective of this systematic review was to assess the efficacy of topical applications containing surface pre-reacted glass-ionomer filler on dental hard tissues. A comprehensive literature search was conducted in PubMed, MEDLINE, Embase, Scopus, ClinicalTrials.gov, Lilacs and Cochrane Central Register of Controlled Trials (until 15.08.2022). Google and Open Grey were used to search for grey literature and handsearching was conducted. Clinical and in vitro studies conducted on human adult teeth were considered eligible without date and language restrictions. The electronic database generated 2,488 results. In total, 227 studies were found to be relevant from which 71 duplicates were removed. Title and abstract screening were then conducted, and a total of 33 studies met the inclusion criteria were assessed for full text screening. Two authors concluded that 11 studies satisfied the eligibility criteria. In vitro studies were evaluated using an accepted quality assessment tool for dental studies. Cochrane risk of bias tool was used for quality assessment of clinical randomised studies, whilst ROBINS-I tool was used for non-randomised studies. Results: Nine in vitro and only two non-randomised clinical trials were reported to meet the eligibility criteria. Results were grouped and analysed separately according to the study design. Different modes of surface pre-reacted glass-ionomer filler delivery were reported in the included studies. Three studies tested the effect of surface pre-reacted glass-ionomer filler containing toothpastes, whilst three studies investigated the effect of polishing pastes with surface pre-reacted glass-ionomer filler, three studies used eluates as surface pre-reacted glass-ionomer filler delivery method and two studies reported the effect of the coatings. The effect of those vehicles was tested on enamel, dentine or oral biofilm. Each study was analysed individually, and heterogeneity was detected among in vitro and clinical studies. Half of the in vitro studies were medium risk, whilst three were low and two studies presented with high risk. In clinical trials, outcome, confounding, selection biases were reported. Meta-analysis was therefore unable to be carried out. Regardless of the mode of delivery and type of studies, all included studies demonstrated the efficacy of surface pre-reacted glass-ionomer filler containing topical applications to inhibit demineralisation of dental hard tissues at a dose dependant manner. Antimicrobial properties towards cariogenic species were also reported. Surface pre-reacted glass-ionomer filler containing topical applications may serve as potential caries preventive and cariostatic tools.
Reference:
Eleni Dimopoulou, Aylin Baysan. Effect of topical applications containing surface pre-reacted glass-ionomer filler on dental hard tissues-A systematic review, Journal of Dentistry,
2024, 104904, ISSN 0300-5712, https://doi.org/10.1016/j.jdent.2024.104904.
(https://www.sciencedirect.com/science/article/pii/S0300571224000745)
Keywords:
Surface, pre-reacted, glass-ionomer filler, topical applications, prevent, caries, Study, Journal of Dentistry, remineralisation; demineralisation; S-PRG filler; enamel; dentine
Powered by WPeMatico

Supplementation with probiotics and vitamin D may benefit cognitive function in schizophrenia patients suggests a new study published in the Neuropsychopharmacology Reports.
Manipulation of the intestinal microbiome and supplying vitamin D can attenuate psychiatric symptoms in schizophrenic patients. The current study tried to evaluate the effects of probiotic/vitamin D supplementation on the cognitive function and disease severity of schizophrenic patients. In the present study, 70 patients (aged 18–65) with schizophrenia were recruited. Participants were randomly allocated to the placebo (n = 35) and intervention (probiotic supplements+400 IU vitamin D, n = 35) groups. Severity of disease and cognitive function (primary outcomes) were evaluated by Positive and Negative Syndrome Scale (PANSS) and Montreal Cognitive Assessment (MoCA) tests, respectively. Moreover, lipid profile, body mass index (BMI), gastrointestinal (GI) problems, serum C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were evaluated as secondary outcomes. Results: A total of 69 patients completed the study. The MoCA score was increased by 1.96 units in the probiotic-containing supplement group compared to the placebo (p = 0.004). Also, the percentage of subjects with MoCA score ≥ 26 rose significantly in the intervention group (p = 0.031). Moreover, TC (p = 0.011), FBS (p = 0.009), and CRP (p < 0.001) significantly decreased in the supplement group compared to the placebo. Although the probiotic supplement reduced PANSS score by 2.82 units, the difference between the study groups was not statistically significant (p = 0.247). Co-administration of probiotics and vitamin D has beneficial effects on the improvement of cognitive function in schizophrenic patients.
Reference:
Mohammadi A, Sadighi G, Nazeri Astaneh A, Tajabadi-Ebrahimi M, Dejam T. Co-administration of probiotic and vitamin D significantly improves cognitive function in schizophrenic patients: A double-blinded randomized controlled trial. Neuropsychopharmacol Rep. 2024; 00: 1–10. https://doi.org/10.1002/npr2.12431
Keywords:
Supplementation, probiotics, vitamin D, benefit, cognitive, function, schizophrenia patients, Mohammadi A, Sadighi G, Nazeri Astaneh A, Tajabadi-Ebrahimi M, Dejam T, Neuropsychopharmacology Reports
Powered by WPeMatico
