Flow cytometry useful alternative to microscopy for differentiation of bronchoalveolar lavage fluid leukocytes: Study
Flow cytometry useful alternative to microscopy for differentiation of bronchoalveolar lavage fluid leukocytes suggests a study published in the Chest.
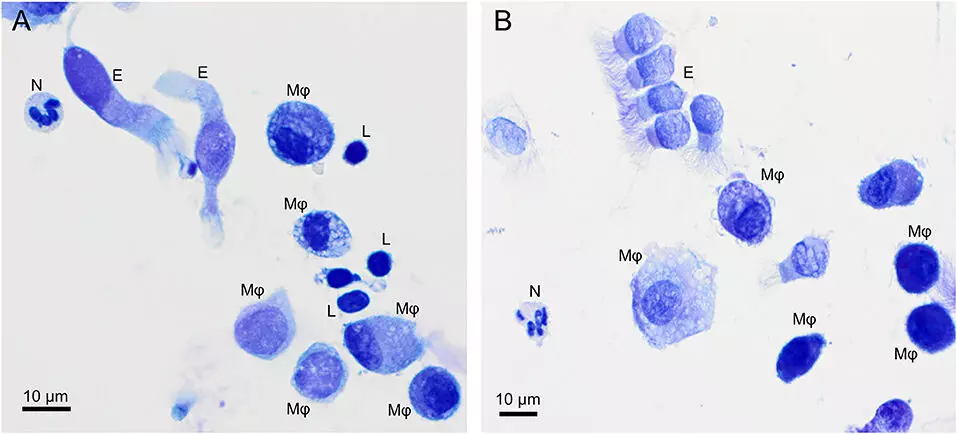
Microscopy is currently the gold standard to differentiate BAL fluid (BALF) leukocytes. However, local expertise for microscopic BALF leukocyte differentiation is often unavailable in clinical practice. A new automated flow cytometric method for BALF leukocyte differentiation, using four antibodies (anti-CD45, anti-CD66b, anti-HLA-DR, anti-CD52) given to human BALF in one tube, was developed and prospectively validated in 745 unselected, subsequent BALF samples from patients with interstitial lung diseases (455 patients), infectious diseases (196 patients), and other diseases (94 patients). Flow cytometry and traditional microscopy were performed by separate investigators in a double-blind fashion. Results were compared using Spearman`s correlation, Deming regression, and Bland-Altman analysis. Results: There was a strong correlation between flow cytometric and microscopic results regarding macrophage/monocyte, lymphocyte, eosinophil, and neutrophil percentages in BALF (P < .001 for all leukocyte subpopulations). Bland-Altman analyses showed that the mean differences between the methods were ≤2% for all four cell types. Flow cytometric results differed less than 20% from microscopic results in more than 95% of all samples. Subgroup analyses confirmed that these results were independent from total leukocyte counts in BALF. They report the first validated flow cytometric method for BALF leukocyte differentiation, which can be used in clinical settings where local expertise for microscopic analysis is unavailable and which can be combined easily with lymphocyte surface marker analysis.
Reference:
Bratke K, Weise M, Stoll P, Virchow JC, Lommatzsch M. Flow Cytometry as an Alternative to Microscopy for the Differentiation of BAL Fluid Leukocytes. Chest. 2024 Mar 26:S0012-3692(24)00426-4. doi: 10.1016/j.chest.2024.03.037. Epub ahead of print. PMID: 38548099.
Keywords:
Flow cytometry, alternative, microscopy, differentiation, bronchoalveolar, lavage fluid leukocytes, Study, Bratke K, Weise M, Stoll P, Virchow JC, Lommatzsch M, BAL fluid; flow cytometry; leukocytes; microscopy.
Powered by WPeMatico