Future parents more likely to get RSV vaccine when pregnant if aware RSV can be a serious illness in infants: Study
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
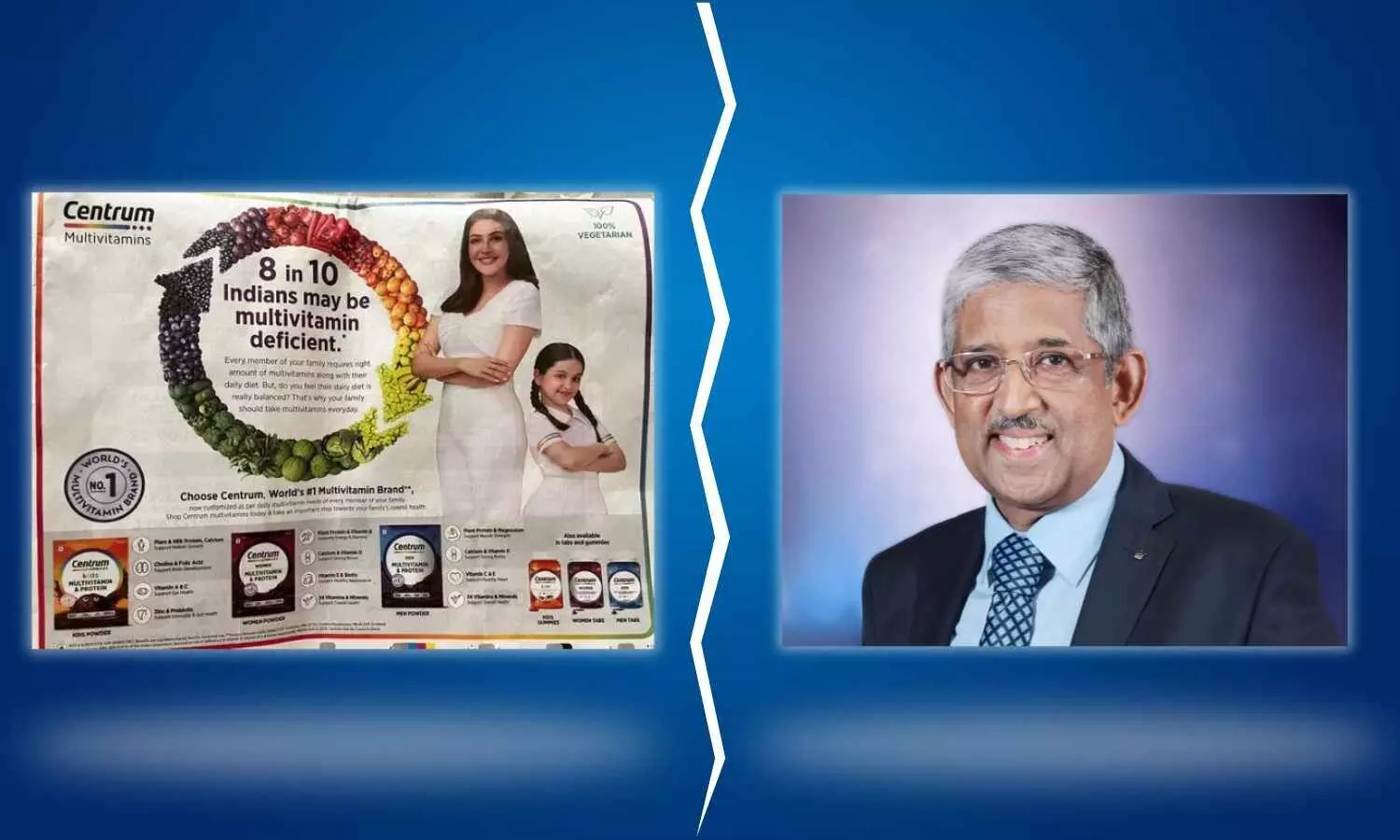
New Delhi: Eminent diabetologist Padmashri Dr V Mohan recently took to social media platform X to rebuke a multivitamin advertisement, asserting that “there’s nothing called multivitamin deficiency.”
The Chennai-based doctor and scientist, who is also the chairman of Dr Mohan’s Diabetes Specialities Centre, criticized the ad’s claim that “8 in 10 Indians may be multivitamin deficient,” deeming it misleading.

In its advertisement, the multivitamin brand Centrum stated that “8 in 10 Indians may be multivitamin deficient*”, followed by stating, “Every member of your family requires the right amount of multivitamins along with their daily diet. But do you think their daily diet is balanced?.That’s why your family should take multivitamins every day, “
” Choose Centrum, World’s #1 Multivitamin Brand**, now customised as per daily multivitamin needs of every member of your family,” the advertisement further reads.
Centrum is a brand of multivitamins produced by Haleon (formerly GlaxoSmithKline Consumer Healthcare)
Responding to the print advertisement given by the company in a leading daily, the internationally acclaimed diabetologist noted that there is nothing called multivitamin deficiency, further stating that unless there is a specific deficiency in vitamins such as D or B12, the indiscriminate use of multivitamins may not be beneficial and may even do harm. He emphasized that multivitamins ususally do not provide enough of the deficient vitamin.
He highlighted the potential harm of indiscriminate multivitamin consumption, noting that in case of deficiency of any vitamin, ” much more of the deficient vitamin will be needed, and much amount may not be available in a multivitamin tablet or capsule. Also, only the deficient vitamin needs to be replaced . Giving all other vitamins and minerals regularly when there is no deficiency can actually cause harm”
In his post, Dr Mohan also tagged Dr KV Babu, a physician from Kerala who sends out RTI (Right To Information) applications on public health issues that concern him as a citizen and a doctor. He is known for challenging Patanjali’s misleading advertisements
There is nothing called multivitamin deficiency. Unless there is deficiency of specific vitamins, Eg. Vit D or B12 , giving multivitamins may not be beneficial and may even do harm. And Multivitamins usually do not provide enough of the deficient vitamin. @drbabukv pic.twitter.com/rwdo9Oe1QI
— Dr.V.Mohan (@drmohanv) April 21, 2024
Responses to Dr Mohan’s post varied, with some individuals expressing gratitude for shedding light on the issue, while others raised concerns about the potential health risks associated with indiscriminate multivitamin consumption. Dr Mohan engaged with commenters, providing further clarification on the limitations of multivitamin supplementation and advocating for targeted vitamin replacement based on individual deficiencies.
Dr Mohan’s insights encourage further research and consideration of individualized approaches to nutrition and supplementation. This exchange drew attention to concerns surrounding multivitamin consumption, particularly in cases where deficiencies are not clearly identified. One user, Dr Gunjan Deshpande further contributed to the discussion by highlighting the high sugar content in certain types of children’s multivitamins, raising additional health considerations.
Another X user, Arun46, suggested that a person could be deficient in multiple vitamins simultaneously, necessitating the use of multivitamins. Dr. Mohan responded by highlighting the challenge of obtaining sufficient amounts of deficient vitamins from multivitamin tablets or capsules. He stressed the importance of replacing only the deficient vitamin rather than administering unnecessary vitamins and minerals.
” But then much more of the deficient vitamin will be needed and that much amount may not be available in a multivitamin tablet or capsule. . Also, only the deficient vitamin needs to be replaced . Giving all other vitamins and minerals regularly when there is no deficiency can actually cause harm,” Dr Mohan noted
The Medical Dialogues team reached out to Haleon for a comment on the matter, but the company had not provided a response at the time of the publication of the story.
Powered by WPeMatico

New Delhi- To submit the requests for verification of credentials issued by the National Board of Examinations in Medical Sciences (NBEMS), the NBEMS has introduced a Credential Verification Online Portal (CVOP). The portal can be accessed through the official website of NBEMS under the “Digital Services” tab.
This portal allows the organisations (Employer/ Public Authority/ Credential Verification Agency) to submit the credential verification requests to NBEMS online as well as the agency to track their submitted requests.
Verification requests submitted through this portal shall be attended by the concerned department at NBEMS and response shall be shared with the Verification Agency concerned at their email ID registered with NBEMS.
With the launch of CVOP, credential verification requests from any agency/organisation through email/by post/any mode other than this portal will not be entertained or responded to.
STEP BY STEP GUIDE FOR ORGANISATIONS SEEKING VERIFICATION OF CREDENTIALS ISSUED BY NBEMS
1 Please advise the concerned candidate to pay the prescribed Credential Verification Fee to NBEMS through the “Miscellaneous Fee Payment Portal” which can be accessed on the NBEMS website under the tab “Digital Services”.
2 Collect a copy of the payment receipt from the concerned candidate which is generated at the above portal on successful payment of verification fee by the candidate.
3 Keep the above-said payment receipt and a clear scanned copy of the Credentials to be verified ready before you begin to submit the verification request to NBEMS through the Credential Verification Online Portal (CVOP). You would also be required to fill in the Roll Number of the candidate. The roll Number of candidates for the respective examination is mentioned on the credential. If it is not mentioned, the same should be obtained from the concerned candidate.
4 Go to NBEMS official website and visit the tab “Digital Services”. Click on the “Credential Verification Online” link.
5 The organisation has to submit an Online Request form for Credential Verification. Following is a screenshot of the Online Request form for Credential Verification.
6 Select the name of the organisation/verification agency from a drop-down list. A verification code shall be sent by email to the Email ID of the selected organisation/agency as available in the NBEMS record.
7 If the organisation/agency is not listed in the said drop-down, it has to approach NBEMS at email ID by submitting a formal letter to add its details to the said list.
8 Select the type of credential to be verified from the dropdown list.
9 Provide the details of the Verification Fee Receipt number and Roll Number of the applicant candidate for backend verification of the fee paid by the applicant to NBEMS.
10 Upload a clear scanned copy of the credential to be verified.
11 If the organisation/agency requires the verification output in its prescribed format, then upload such format also.
12 After inputting all the required fields, generate the Email Verification Code which shall be mailed to the registered email ID.
13 Enter the verification code on the designated input box and submit the request form.
14 In case the Verification Code is not received in email, the applicant may regenerate the code after a small time instance.
15 After Successful Submission of the form, the organisation/agency shall receive a formal acknowledgement email at its email ID registered with NBEMS.
16 The outcome of verification shall be communicated to the agency concerned by way of an official email from NBEMS email ID.
17 The process of credential verification is usually completed within 4 weeks of receipt of the verification request.
18 Request for Credential Verification submitted to NBEMS through any mode other than the Online Credential Verification Portal shall NOT be entertained.
Concerned candidates whose credentials are to be verified should note that the respective organisation shall be able to submit the request for verification to NBEMS only after the concerned candidate has already paid the prescribed fee for verification to NBEMS through its Miscellaneous Fee Payment Portal. Therefore, candidates are requested to share a copy of the payment receipt with the concerned organisation along with the credentials the candidates want to verify.
For any queries/clarification related to the online submission of verification requests to NBEMS through the Credential Verification Online Portal (CVOP), candidates may write to NBEMS, the notice stated.
To view the notice, click the link below
Powered by WPeMatico

Chennai: In recognition of their exceptional contributions to society and the medical field, the Indian Academy of Neurology Practitioners and the South India Neurological Academic Forum have presented the Legend of Medicine Award to three distinguished medical professionals.
The awards ceremony took place as part of a continuing medical education program held on Sunday, celebrating the notable careers of these medical practitioners. The Legend of Medicine Award acknowledges the impactful work of these doctors, honouring their dedication to advancing healthcare and their significant influence on the medical community.
Dr Devarajan graduated in medicine and went on to take the degrees of MD and DSc in general medicine. He was also awarded the Fellowship of the Royal College of Physicians of Glasgow in 2007. The Government of India honoured him, in 2013, by awarding him the Padma Shri.
Dr D. Shantharam is a Senior Consultant Diabetologist and General Physician at Apollo Hospitals in Greams Road, Chennai. He also practices at Apollo Sugar Clinics in Anna Nagar, Chennai. Dr Shantharam has 38 years of experience and is a renowned endocrinologist in Tamil Nadu. He treats all types of diabetes, including type 1 and type 2, as well as thyroid disorders, hypertension, anaemia, fever, asthma, COPD, and other chronic illnesses.
He has received many awards for his teaching and service in the field. He is the Joint Secretary for the Diabetes Association of India, Southern Chapter, and the Treasurer for the Diabetes Alumni Association. He is also a well-known member of the JIPMER, MCI Ethical Committee, and Diabetic Association of India. V Sundaravadivelu is a former director-in-charge of the Institute of Internal Medicine at Madras Medical College and Hospital in Chennai.
The Indian Academy of Neurology (IAN) is the umbrella body of all neurologists in India. The genesis of this super speciality association was laid in a meeting on 16th December 1991 where 40 to 50 Neurologists met at Manipal under the leadership of Dr J S Chopra and decided to form this association. Since then, IAN has grown from strength to strength and today has a membership of around 3,000 neurologists from the length and breadth of the country. IAN is focussed on service to patients, teaching neurology to members, students and educating patients as well as pursuing academic excellence in the field of neurology.
Also Read: Dr Manohar Krishna Dole, Dr Zahir Ishaq Kazi conferred with Padma Shri
Powered by WPeMatico

New Delhi: The doctors at Surya Mother and Child Hospital, Pune successfully performed surgery to save the life of a four-year-old boy suffering from Midgut Volvulus, a condition where the intestine becomes twisted.
Midgut volvulus is a severe condition that is common among children and infants and often occurs within the first few weeks of life, caused by a congenital anomaly of the intestines — leaving the child susceptible to sudden twisting of most of the intestines.
Symptoms include upper abdominal distension, bilious vomiting, and abdominal tenderness, signalling the need for immediate medical attention. While the condition is treatable, late detection of the condition could rapidly deteriorate the patient’s health and can be fatal.
Also Read:Medical experts concerned over lack of quality neonatal care
According to an IANS report, The boy, Sankalp, was admitted to Surya Mother and Child Hospital, Pune in an extremely deteriorated condition with wasted muscles, an immensely bloated abdomen, and dehydration.
“Delayed detection of midgut volvulus increases treatment challenges and risks of a high fatality rate,” said Sachin Shah, Director – Neonatal and Pediatric Intensive Care Services, Surya Mother and Child Super Speciality Hospital, Pune.
Sankalp was initially treated at a tertiary care hospital in Varanasi, where he underwent surgery. However, his recovery was fraught with challenges, leading to multiple corrective surgeries that failed to improve his condition.
Despite the efforts, Sankalp’s health continued to deteriorate, and his family was informed that further medical intervention seemed futile.
At the Pune hospital, the team of doctors assessed Sankalp’s condition and opted for a re-surgery to address the condition.
During the extensive four-hour procedure, they encountered adhesions in Sankalp’s abdomen, which had caused the intestines to adhere together, severely impairing their function.
“Despite these odds, the surgical team meticulously separated the intestines, repaired the damage, and restored their function during the extensive surgery,” Sachin said.
With their effort, Sankalp made a “remarkable recovery within 48 hours post-surgery”, reports news agency
After six days of abstaining from solid food, Sankalp was finally able to consume real food again, marking a significant milestone in his journey to health and recovery.
“Following a successful recovery, Sankalp was discharged after 10 days and closely monitored for the next three months. Once the doctors were satisfied with the healthy weight gain after a three-month follow-up period, Sankalp was discharged,” the doctor said.
Powered by WPeMatico

Infants and children who have severe cases of respiratory syncytial virus (RSV) before age 2 are likely to have changes to their lung structure and function that could affect respiratory health later in life. The study is published ahead of print in the American Journal of Physiology-Lung Cellular and Molecular Physiology and has been chosen as an APSselect article for April.
Most children contract RSV, a lower respiratory tract disease, before they are 2 years old. Mild forms of the disease mimic the common cold with symptoms such as coughing, runny nose, congestion and sneezing. Severe forms of RSV can include wheezing, trouble breathing and, when oxygen levels are compromised, a blue tinge to the skin. A severe infection can affect a child’s future health as well. “[S]evere early-life RSV infection is associated with childhood wheezing related to respiratory viral infection exacerbation, allergies and asthma, that is accompanied by compromised lung function,” the researchers wrote.
To study severe RSV, the researchers measured lung function and alveolarization in infant mice. Alveolarization is the development of alveoli, the sacs in the lungs responsible for exchanging oxygen and carbon dioxide. “Alveolarization continues into adulthood with maximum alveolarization occurring between [2 and 3 years old] in humans,” the team wrote. Production of large numbers of immune cells occurs around the same time.
The researchers measured these markers at five weeks and three months after the initial RSV infection and again after a reinfection with the virus. They found “significant defects” in the ability of the lungs to stretch and expand during breathing. Structural changes to the mice’s lungs included an increase in alveoli size but fewer individual alveoli after RSV infection.
“These data indicate that the lungs of mice following an early-life RSV infection have a decreased lung function even at [three months] postinfection,” the research team wrote. “Importantly, the structural defects of the early-life infected mice largely mimic the clinical setting where severe exacerbations are observed in children for several years following a severe early-life respiratory infection, especially RSV.”
Reference:
Carrie-Anne Malinczak et al, Early-life pulmonary viral infection leads to long-term functional and lower airway structural changes in the lungs, American Journal of Physiology-Lung Cellular and Molecular Physiology (2024). DOI: 10.1152/ajplung.00300.2023.
Powered by WPeMatico

Sweden: Fractional flow reserve (FFR)-guided complete revascularization does not result in better outcomes compared with primary percutaneous coronary intervention (PCI) of the culprit lesion among patients with STEMI or very-high-risk NSTEMI and multivessel coronary artery disease, randomized FULL REVASC trial has shown.
“At a median follow-up of 4.8 years, a primary outcome event — myocardial infarction, death from any cause, or unplanned revascularization — occurred in 19% of patients in the complete-revascularization group versus 20.4% of those in the culprit-lesion-only group (HR 0.93),” the researchers reported during the American College of Cardiology annual meeting. The findings were subsequently published in The New England Journal of Medicine.
Also, there were no differences in the composite of death from any cause or myocardial infarction between the complete-revascularization group and the culprit-lesion-only group (16.5% vs 15.3%; HR 1.12) or unplanned revascularization (9.2% vs 11.7%; HR 0.76).
When a patient presents with myocardial infarction, the urgency to restore blood flow to the affected area is paramount. PCI has long been the standard of care, but the debate continues between complete revascularization and culprit-only intervention. FFR has emerged as a valuable tool in guiding this decision-making process, offering insights into the hemodynamic significance of coronary lesions.
Against the above background, Felix Böhm, the Karolinska Institutet and Danderyd Hospital in Sweden, and colleagues explored the role of FFR guidance in determining whether complete or culprit-only PCI is more appropriate for patients with MI.
For this purpose, the researchers conducted a multinational, registry-based, randomized trial, including patients with STEMI or very-high-risk non-STEMI (NSTEMI) and multivessel disease undergoing primary PCI of the culprit lesion. A total of 1542 patients underwent randomization, 764 were assigned to receive FFR-guided complete revascularization, and 778 were assigned to receive culprit-lesion-only PCI.
The two key secondary outcomes were a composite of death from any cause or myocardial infarction and unplanned revascularization.
The following were the key findings of the study:
In conclusion, among patients with STEMI or very-high-risk NSTEMI and multivessel coronary artery disease, FFR-guided complete revascularization did not result in a lower risk of a composite of death from any cause, myocardial infarction or unplanned revascularization than culprit-lesion-only PCI at 4.8 years.
The study’s main limitation was that it had to be terminated early for feasibility and ethical reasons, which resulted in a long duration of follow-up for enough events to accrue.
Reference:
Böhm F, Mogensen B, Engstrøm T, Stankovic G, Srdanovic I, Lønborg J, Zwackman S, Hamid M, Kellerth T, Lauermann J, Kajander OA, Andersson J, Linder R, Angerås O, Renlund H, Ērglis A, Menon M, Schultz C, Laine M, Held C, Rück A, Östlund O, James S; FULL REVASC Trial Investigators.. FFR-Guided Complete or Culprit-Only PCI in Patients with Myocardial Infarction. N Engl J Med. 2024 Apr 8. doi: 10.1056/NEJMoa2314149. Epub ahead of print. PMID: 38587995.
Powered by WPeMatico
