Collagen patch cover applied to anastomotic site after laparoscopic colectomy may facilitate recovery of bowel function: Study
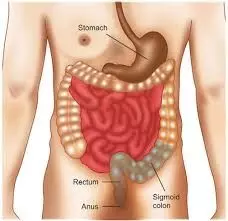
Collagen patch cover applied to anastomotic site after laparoscopic colectomy may facilitate recovery of bowel function suggests a new study published in the BMC Surgery.
Numerous factors can influence bowel movement recovery and anastomotic healing in colorectal surgery, and poor healing can lead to severe complications and increased medical expenses. Collagen patch cover (CPC) is a promising biomaterial that has been demonstrated to be safe in animal models and has been successfully applied in various surgical procedures in humans. This study. A retrospective review of medical records from July 2020 to June 2022 was conducted to identify consecutive patients who underwent laparoscopic colectomy. Patients who received CPC at the anastomotic site were assigned to the collagen group, whereas those who did not receive CPC were assigned to the control group. Results: Data from 241 patients (collagen group, 109; control group, 132) were analyzed. Relative to the control group, the collagen group exhibited a faster recovery of bowel function, including an earlier onset of first flatus (2.93 days vs. 3.43 days, p < 0.01), first defecation (3.73 days vs. 4.18 days, p = 0.01), and oral intake (4.30 days vs. 4.68 days, p = 0.04). CPC use was also associated with lower use of postoperative intravenous analgesics. The complication rates in the two groups did not differ significantly. CPCs can be safely and easily applied to the anastomotic site during laparoscopic colectomy, and can accelerate bowel movement recovery. Further studies on the effectiveness of CPCs in colorectal surgery involving larger sample sizes are required.
Huang, PY., Tsai, MC., Kiu, KT. et al. Collagen patch cover facilitates recovery of bowel function after laparoscopic colectomy. BMC Surg 24, 66 (2024). https://doi.org/10.1186/s12893-024-02339-w
Keywords:
Collagen patch, cover, anastomotic site, laparoscopic colectomy, recovery, bowel function, BMC Surgery, Huang, PY., Tsai, MC., Kiu, K
Powered by WPeMatico