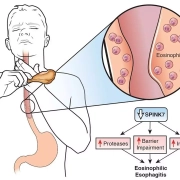
Twice-daily PPI dosage improves outcomes among patients of eosinophilic esophagitis: Study
A recent study by Mayssan Muftah and colleagues explored the most effective dosing strategies for treating Eosinophilic Esophagitis (EoE) which is a chronic immune system disease that affects the esophagus. The key findings of this study were published in the American Journal of Gastroenterology.
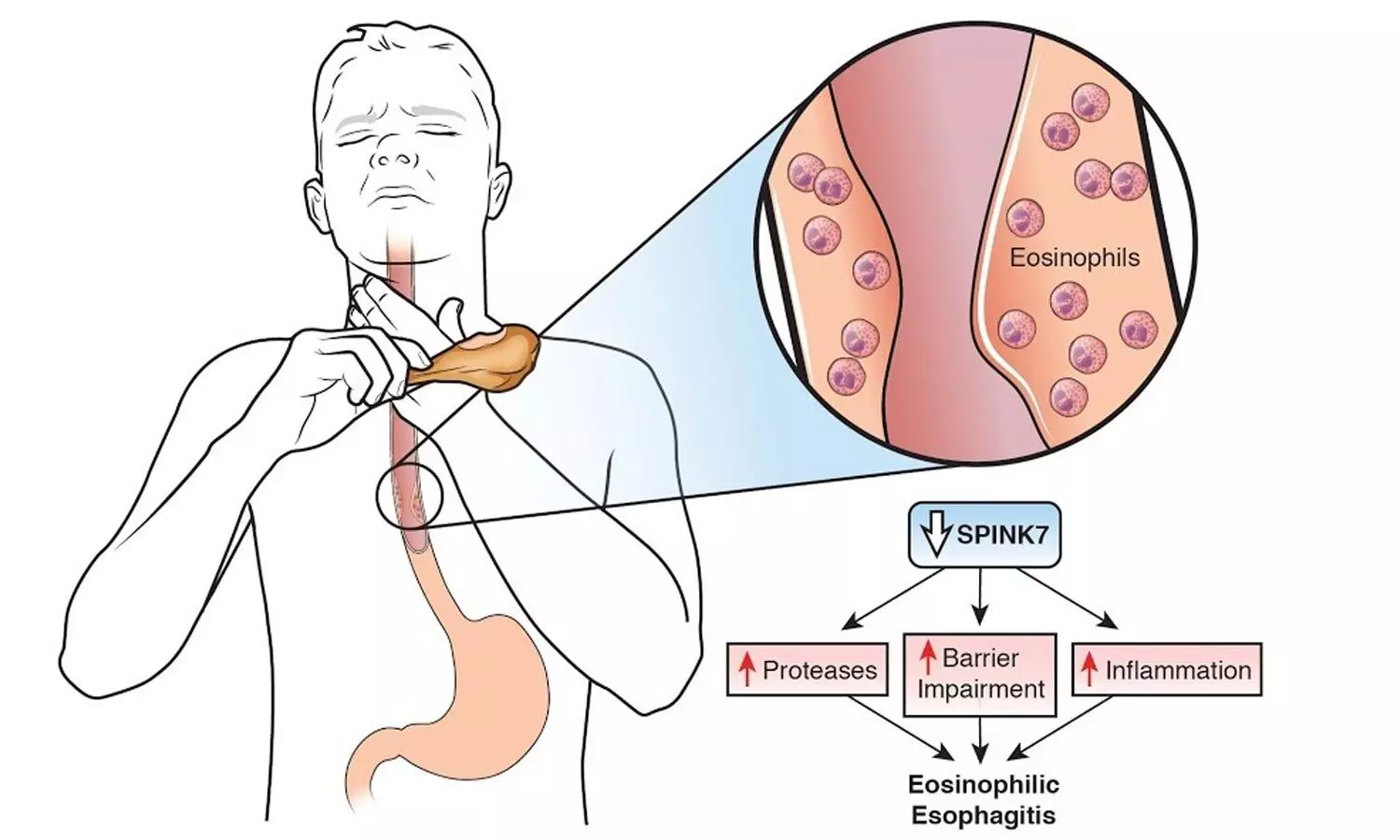
Eosinophilic Esophagitis is marked by the accumulation of eosinophils in the esophagus that leads to inflammation, difficulty swallowing and food impaction. This comprehensive analysis involved a total of 305 newly diagnosed EoE patients and compared their histologic response rates among various dosing regimens of proton pump inhibitors (PPIs), a common treatment for the condition.
This study meticulously evaluated the effects of different PPI dosages including standard (omeprazole 20 mg daily), moderate (either 40 mg once daily or 20 mg twice daily) and high (40 mg twice daily) doses were administered over a period of at least 8 weeks. Remarkably, these findings reveal a significant disparity in the efficacy of treatment which highlights the superiority of twice-daily dosing over once-daily regimens.
About 42.3% of the patients achieved a histologic response to their PPI treatment with response rates that were markedly higher in the twice-daily groups. Also, 52.8% of the patients on the moderate twice-daily dose and 54.3% of the patients on the high twice-daily dose showed histologic improvement. In stark contrast, the once-daily dosing regimens (standard and moderate) had significantly lower response rates of 11.8% and 10%, respectively.
The multivariable analysis further illuminated the advantage of the twice-daily dosing schedule. The moderate twice-daily dose was associated with an adjusted odds ratio of 6.75 for achieving a histologic response. The high twice-daily dose had an even more pronounced effect with an adjusted odds ratio of 12.8. These statistics outcome suggest that patients who were receiving the twice-daily regimens were significantly more likely to express histological improvement by making a compelling case for revisiting current EoE treatment protocols.
This research illuminates the path forward for more effective management of Eosinophilic Esophagitis and also underlines the importance of dosage timing in the treatment regimen. Overall, these findings direct us to the potential of PPI for improved quality of life for EoE patients that offers promise for the individuals with this condition.
Reference:
Muftah, M., Goldin, A. H., Barshop, K., Hsu Blatman, K., Hamilton, M. J., Lo, W.-K., Hornick, J. L., & Chan, W. W. (2024). Twice-Daily Proton Pump Inhibitor Induces Higher Remission Rate in Eosinophilic Esophagitis Than Once-Daily Regimen Regardless of Total Daily Dose. In American Journal of Gastroenterology. Ovid Technologies (Wolters Kluwer Health). https://doi.org/10.14309/ajg.0000000000002712
Powered by WPeMatico