Omega-3 Fatty Acids fail to provide protection against retinopathy among diabetes patients
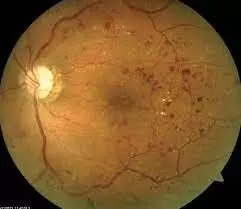
Omega-3 Fatty Acids fail to provide protection against retinopathy among diabetes patients suggests a new study published in the Ophthalmology.
Results from a substudy of the ASCEND trial suggest that the use of omega-3 fatty acids had no clinically meaningful benefit compared to placebo for the development of diabetic retinopathy.
“Preclinical studies demonstrate a protective role for omega-3 fatty acids in diabetic retinopathy, but these observations have not been confirmed in randomized trials,” the researchers write.
The safety and effectiveness of omega-3 fatty acids on health has been under the microscope of cardiometabolic health study participants for a decade. Although much of the attention has been devoted to the REDUCE-IT and STRENGTH studies, which examined icosapent ethyl (Vascepa) and an EPA/DHA agent, respectively, several other studies have been initiated to further explore the associations between different forms of omega to study -3 fatty acids, like the ASCEND study.
In a double-blind, randomized, placebo-controlled trial of adult patients aged 40 years and older with diabetes but no apparent cardiovascular disease, the A Study of Cardiovascular Events in Diabetes (ASCEND), 15,480 patients were randomized to a 1st course -gram capsule containing 460 mg eicosapentaenoic acid and 380 mg docosahexaenoic acid or equivalent placebo with olive oil daily. The study’s primary outcome of interest was first major vascular event and median follow-up duration of 7.4 years.
The results of the study indicate that a major vascular event occurred in 8.9% of the omega-3 fatty acid group and 9.2% of the placebo group (rate ratio). [RR], 0.97; 95% confidence interval [CI]0.87 to 1.08; P=.55). Further analysis showed that all-cause deaths occurred in 9.7% of the omega-3 fatty acid group and 10.2% of the placebo group (RR: 0.95; 95% CI: 0.86 to 1, 05).
In a substudy of the ASCEND trial called ASCEND-EYE, a team of researchers led by Jane Armitage, FRCP, FFPH, from the Nuffield Department of Public Health, used linked data from the records of the NHS Diabetic Eye Screening Program in England and Wales to To identify participants from the study who developed diabetic retinopathy. The investigators noted that ocular events reported were assessed through medical record review.
The primary efficacy outcome of interest for the subsidy was time to first record of a communicable disease after randomization, which researchers defined as a combination of communicable retinopathy or communicable maculopathy based on evaluation criteria established by the UK National Screening Committee . The sub-study also included several secondary and tertiary outcomes, such as: B. Transferable disease outcomes stratified by baseline DR severity, any progression of retinopathy grade, and incident diabetic maculopathy.
A total of 7360 participants with linkage data were included in the current study, representing 48% of those randomized in ASCEND. At baseline, this cohort had a mean age of 63.5 (standard deviation: 8.9) years, 62% of the group were male, 96% were white, and 95% had type 2 diabetes. The median follow-up duration in this cohort was 6.5 years.1.4
In the analysis, 14.8% of the omega-3 fatty acid group and 13.9% of the placebo group experienced a transmissible disease event (RR: 1.07; 95% CI: 0.95-1.20 ; P=.29). Further analysis revealed that there were no statistically significant differences between groups in
the proportion of events for the secondary or tertiary endpoints.
Reference:
Sammons EL, Buck G, Bowman LJ, et al. ASCEND-Eye: Effects of Omega-3 Fatty Acids on Diabetic Retinopathy. Ophthalmology. Published online December 3, 2023. doi:10.1016/j.ophtha.2023.11.030
Keywords:
Omega-3, Fatty, Acids, fail, provide, protection, against, retinopathy, among, diabetes, patients, Sammons EL, Buck G, Bowman LJ, Ophthalmology
Powered by WPeMatico